Supply Chain Disruption: How Drug Shortages and Pharmacy Delays Affect Your Medications
When supply chain disruption, a breakdown in the movement of medicines from manufacturers to pharmacies. It’s not just a business problem—it’s a health crisis. happens, you don’t get your pills on time. That’s not a delay. It’s a risk. Think about people who rely on insulin, blood pressure meds, or even generic antibiotics. When factories shut down, shipping routes get blocked, or raw materials run out, those pills vanish from shelves. And it’s not rare. In 2023, over 300 drugs had reported shortages in the U.S. alone. Some lasted weeks. Others dragged on for months.
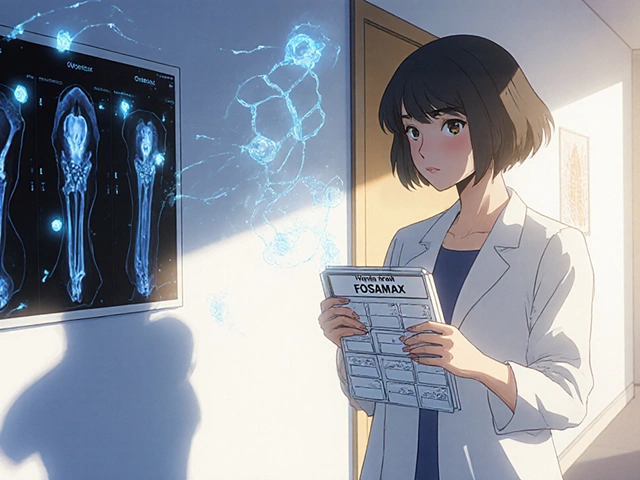
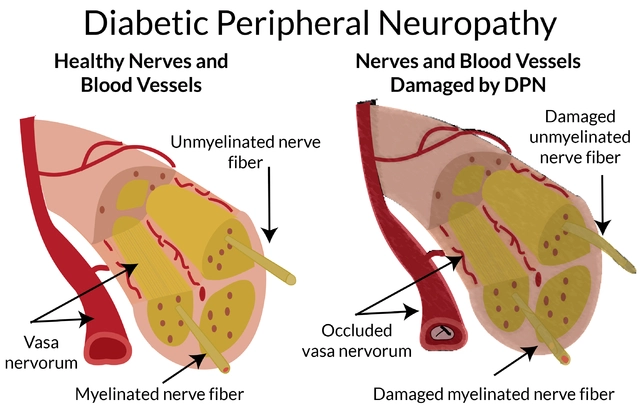
drug shortages, when a medication isn’t available in sufficient quantities to meet patient demand. This isn’t about stockpiling—it’s about daily survival. hit hardest with drugs that have few alternatives. Take digoxin, for example. Its narrow therapeutic index means switching brands or generics can cause toxicity or treatment failure. Or venlafaxine—when supply falters, patients face sudden mood swings or withdrawal. Even common drugs like alendronate (Fosamax) or tamsulosin (Temsujohn) aren’t safe from this. And it’s not just the big names. Generic versions, which most people depend on for affordability, are often the first to disappear because manufacturers cut corners to save costs. Pharmacist substitution authority helps sometimes, but only if the generic is actually in stock. When it’s not, you’re stuck waiting—or paying more for the brand.
pharmaceutical distribution, the complex network of manufacturers, wholesalers, and pharmacies that deliver medicines to patients. This system is fragile. One factory in India or China shuts down due to inspections or labor issues, and the ripple effect hits U.S. pharmacies in weeks. Even weather events or port strikes can delay shipments. And when that happens, pharmacies can’t just order more. Many are locked into contracts with single suppliers. No backup means no pills. Meanwhile, medication access, a patient’s ability to obtain prescribed drugs without delay or financial hardship. This isn’t just about money—it’s about timing. gets worse for seniors, rural patients, and those on fixed incomes. They can’t fly to another state or pay triple for a brand-name substitute. And when pharmacists try to swap meds under collaborative practice agreements, they’re often blocked by insurance rules or lack of stock.
What’s behind all this? It’s not one thing. It’s a mix: over-reliance on overseas suppliers, thin profit margins on generics, lack of regulatory oversight in production, and no real contingency planning. The system was built for efficiency, not resilience. And now, every natural disaster, political shift, or factory fire puts lives at risk. You might think this is a distant issue—something that happens in headlines. But if you’ve ever waited weeks for a refill, switched meds mid-treatment, or had your doctor call because the pharmacy had nothing—you’ve felt it. This isn’t theoretical. It’s personal.
The posts below show you exactly how this plays out in real life: from counterfeit pills flooding online pharmacies to bioavailability issues with digoxin generics, from pharmacist substitution rules that vary by state to how drug interaction checkers can’t help when the medicine simply isn’t there. You’ll see how supply chain breakdowns connect to everything—from insulin stacking risks to herbal supplement dangers. This isn’t just about logistics. It’s about safety, control, and survival. What you find here isn’t theory. It’s what’s happening to real people right now.