When a drug production line stops, it’s not just a delay-it’s a life-or-death moment. Imagine a hospital running low on insulin, or a cancer patient waiting for their chemotherapy drug, only to find out the factory made a mistake and had to shut down. This isn’t fiction. In 2023, over 150 prescription drugs in the U.S. faced shortages, and nearly half of them were tied directly to quality problems that forced manufacturers to halt production.
Why Quality Issues Stop Drug Production
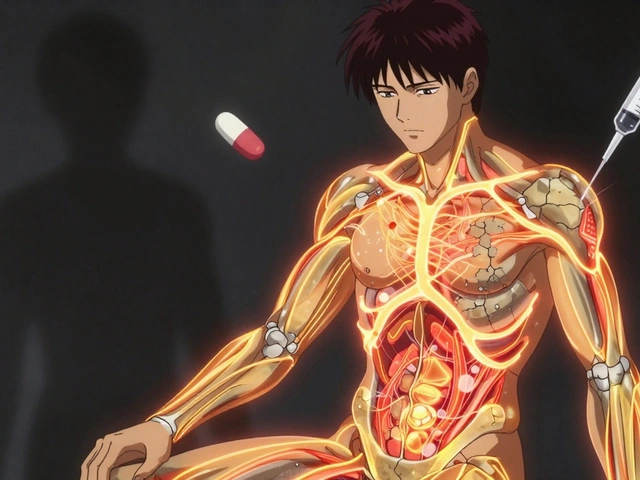
Unlike making smartphones or cars, pharmaceutical manufacturing can’t afford even one faulty batch. A single vial of contaminated medication can cause illness, death, or a massive recall. That’s why regulators like the FDA and EMA don’t just inspect factories-they demand systems that stop production the moment something goes wrong. Quality problems that trigger halts aren’t always obvious. They include:- Microscopic particles in injectable drugs
- Incorrect potency-too much or too little active ingredient
- Contamination from mold, bacteria, or cross-reacting chemicals
- Wrong labeling or packaging (e.g., a blood pressure pill in a diabetes bottle)
- Equipment failures during sterile filling
The Real Cost of a Halt
Most people think a production halt just means fewer pills on the shelf. But the financial and human cost is far deeper. A single quality-related shutdown in a pharmaceutical plant can cost between $150,000 and $500,000 per hour, depending on the drug’s complexity. That’s not just lost wages or idle machines-it’s the cost of:- Scraping entire batches worth millions of dollars
- Revalidating equipment and processes (which takes weeks)
- Delayed patient access to life-saving treatments
- Legal exposure and regulatory penalties
How Long Do These Halts Last?
Not all halts are the same. In electronics or auto plants, a stoppage might last minutes. In pharma, it’s measured in days, weeks, or months. According to FDA data from 2023:- Simple labeling or packaging errors: 2-7 days to fix
- Contamination or sterility breaches: 3-12 weeks
- Major process failures requiring revalidation: 3-6 months

Who Decides to Halt Production?
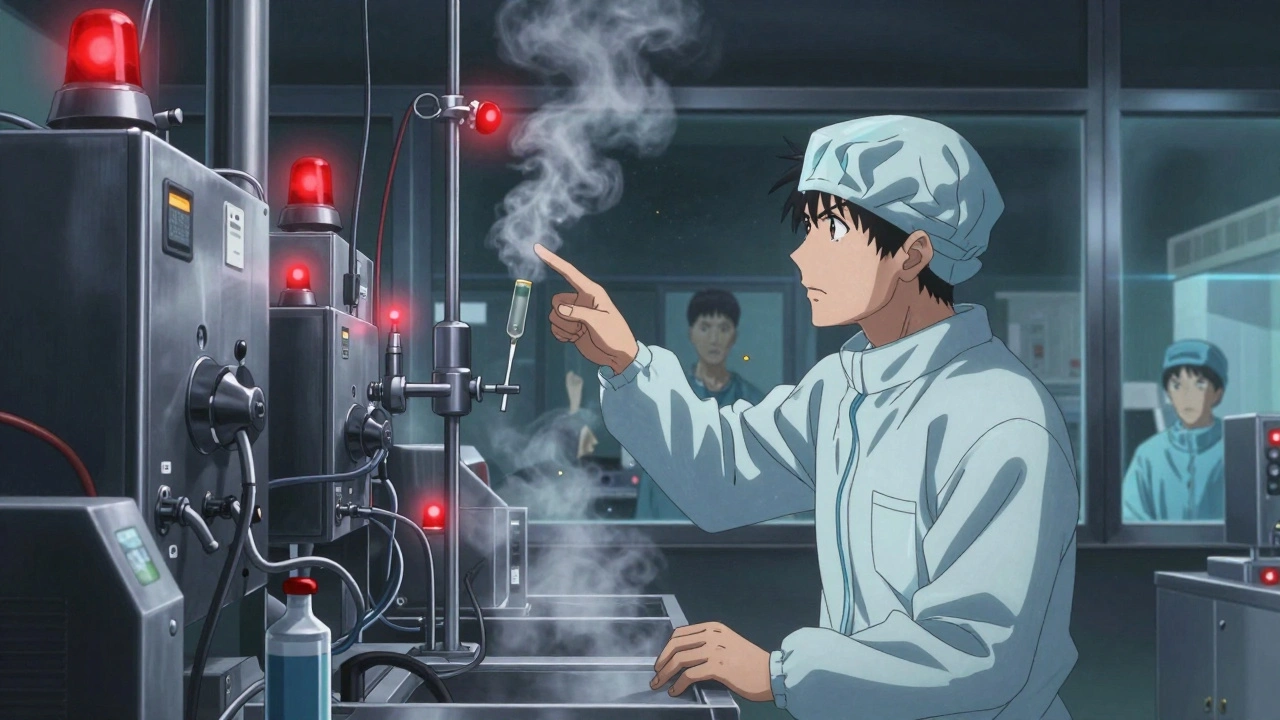
It’s not the CEO. It’s not the shift manager. It’s the quality technician on the floor. Modern pharmaceutical facilities operate under a “stop-work authority” policy. Any employee who spots a quality issue-no matter how small-has the power and responsibility to shut down the line. This isn’t optional. It’s required by FDA guidelines. One nurse in Ohio told me about a time her hospital ran out of a critical antibiotic. She later learned the manufacturer had halted production because a sensor detected a 0.2% variance in pH during mixing. To most people, that sounds tiny. But in drug manufacturing, even 0.1% can change how the body absorbs the medicine. The line stopped. The batch was destroyed. And yes-it saved lives.Why Do These Problems Keep Happening?
You’d think after decades of regulations, these issues would be rare. But they’re not. The biggest causes are:- Outdated equipment: Many drug plants still use machines from the 1990s. They’re reliable, but not precise enough for modern standards.
- Supply chain gaps: Active pharmaceutical ingredients (APIs) often come from just a few countries. If a factory in India or China has a quality issue, it affects every drug made worldwide.
- Understaffed quality teams: In smaller manufacturers, one person might be responsible for inspecting 10 different lines. Fatigue leads to missed errors.
- Pressure to cut costs: When companies cut corners on cleaning validation or training, quality suffers.
What’s Being Done to Fix This?
The industry isn’t standing still. Here’s what’s working:- Digital twins: Virtual models of production lines simulate quality risks before a single pill is made. Companies like Pfizer and Novartis now use them to predict and prevent halts.
- AI-powered inspection: Cameras and machine learning now detect defects invisible to the human eye-like a tiny crack in a capsule or a speck of metal in a solution.
- Blockchain for raw materials: Some manufacturers now track every batch of API from source to final product. If one supplier has an issue, they can isolate it fast.
- Real-time data monitoring: Sensors track temperature, pressure, humidity, and flow rates 24/7. If something drifts outside the safe zone, the system alerts operators before a batch is ruined.
What Patients and Providers Can Do
You can’t control a factory. But you can stay informed.- Check the FDA’s Drug Shortages list regularly. It’s updated weekly.
- If your medication is suddenly unavailable, ask your pharmacist about therapeutic alternatives. Many drugs have safe substitutes.
- Report unexplained side effects or packaging errors to the FDA’s MedWatch program. These reports help regulators spot patterns before more people are affected.
- Support policies that incentivize domestic manufacturing of critical drugs. The U.S. government has started funding new facilities-but progress is slow.
The Future: Less Halt, More Prevention
The goal isn’t to stop more often. It’s to stop less-by preventing problems before they start. By 2026, Gartner predicts AI systems will automatically trigger and resolve 60% of quality issues without human input. That sounds scary, but here’s the truth: the best systems combine machines and people. AI spots the anomaly. A trained technician confirms it. A manager decides the fix. That’s how you avoid both over-reaction and under-reaction. The most successful manufacturers now treat quality halts not as failures-but as feedback. Every shutdown is a chance to learn. To improve. To protect. And in the world of medicine, that’s not just good business. It’s the only way to be trusted.Why do drug production halts take longer than in other industries?
Drug production halts take longer because every step must meet strict regulatory standards. Unlike making a phone or a car, you can’t just fix a mistake and keep going. Pharmaceutical facilities must document every change, revalidate equipment, test for contamination, and get approval from regulators like the FDA. A simple labeling error might take a few days. A contamination issue can take months. The goal isn’t speed-it’s safety.
Can a small quality issue really shut down an entire drug plant?
Yes. Even a tiny issue-like a single particle in an injectable drug or a 0.1% variation in potency-can trigger a full shutdown. That’s because drugs are used by vulnerable patients. A batch that’s slightly off might not harm most people, but for someone with kidney failure or cancer, it could be deadly. Regulations require manufacturers to treat every deviation seriously, even if the risk seems low.
Who has the authority to stop drug production?
Any trained employee on the production floor has the authority to stop production if they spot a quality issue. This is called “stop-work authority” and is required by the FDA. It empowers technicians, operators, and even cleaners to halt the line if they see something wrong. This culture of responsibility has reduced errors by up to 40% in facilities that use it properly.
Are drug shortages always caused by quality problems?
No. While quality issues are a major cause, other factors include raw material shortages, natural disasters, equipment breakdowns, and regulatory delays. But quality problems are the most preventable-and the most dangerous. When a plant shuts down because of contamination or incorrect dosing, it’s a sign the system failed to catch the problem before it happened.
How can I find out if my medication is in short supply?
You can check the U.S. Food and Drug Administration’s (FDA) official Drug Shortages page, which is updated weekly. Pharmacies also track shortages and may notify you if your prescription is affected. If you’re unsure, ask your pharmacist-they have access to real-time supply data and can suggest alternatives if needed.
What’s being done to prevent future drug shortages?
Manufacturers are investing in AI-driven quality monitoring, digital twins, and blockchain tracking of raw materials. Governments are offering incentives to build domestic production capacity. The FDA is also speeding up inspections and allowing more flexibility for emergency supply transfers. But the biggest change is cultural: companies are now trained to see quality halts not as failures, but as early warnings that help them improve.



Jennifer Patrician
December 5, 2025They’re lying to us. The FDA doesn’t want to shut plants down-they’re in bed with Big Pharma to keep prices high. Every ‘quality issue’ is a manufactured crisis to scare you into paying more. I’ve seen the internal memos. They’d rather let people die than let a competitor make insulin cheaper.
Mellissa Landrum
December 7, 2025lol so the whole drug supply chain is just a government scam? i always knew they were hiding something. they put microchips in the pills to track us. that’s why they shut down plants-so they can reset the chips. my cousin’s aunt’s neighbor works at a factory and said they’re replacing all the vials with nano-gps trackers. stay vigilant fam.
Mark Curry
December 8, 2025It’s kind of beautiful, really. We’ve built a system where a single speck of dust can save a life. The machine doesn’t care about profit or politics-it just stops. Maybe we need more of that in other areas. Not control. Not speed. Just… pause. And think.
Manish Shankar
December 8, 2025As someone who has worked in API manufacturing in India, I can confirm that the quality control standards are often compromised due to understaffing and pressure to meet deadlines. The systems are not inherently flawed, but the human and economic pressures are immense. Many facilities operate with outdated equipment because capital investment is not prioritized. This is not just an American problem-it is a global supply chain failure.
luke newton
December 9, 2025People don’t realize that if you’re not dying from a drug shortage, you’re just lucky. The real criminals are the CEOs who cut corners on cleaning protocols and then donate to politicians to delay inspections. I’ve seen the reports. They knew. They just didn’t care. And now a child is missing their epilepsy med because someone thought ‘it’s probably fine.’ It’s not fine. It’s murder by bureaucracy.
Ali Bradshaw
December 10, 2025There’s something deeply human about the idea that a line worker can stop the whole machine. In a world obsessed with efficiency, that’s radical. It says: your safety matters more than the clock. I hope more industries learn from this. Not just pharma.
an mo
December 11, 2025AI-driven quality monitoring? Please. That’s just corporate vaporware. The real issue is offshoring. We outsourced our entire supply chain to China and India because we wanted cheaper pills. Now we’re paying with lives. We need a national pharmaceutical industrial policy-domestic production, mandatory audits, and zero tolerance for foreign dependency. This isn’t healthcare-it’s national security.
aditya dixit
December 12, 2025It’s interesting how we treat drug manufacturing like a sacred ritual. Every variable is controlled, every sensor monitored, every batch traced. But we still expect human beings to be flawless. Maybe the answer isn’t more machines, but better training, better pay, and less burnout. Quality isn’t a system-it’s a culture. And culture can’t be automated.
Lynette Myles
December 13, 2025They shut down the plant over a 0.1% pH shift. That’s not safety. That’s fear.
Annie Grajewski
December 13, 2025so like… we’re using AI to find micro-particles in medicine but we still can’t fix our own healthcare system? 🤦♀️ we’ve got robots sniffing out contamination but no one can figure out why my prescription costs $800? i mean… congrats? we built a robot that saves lives while we all die from medical bills? 🤷♀️
Philip Kristy Wijaya
December 14, 2025While the narrative here is emotionally compelling it fundamentally misrepresents the nature of regulatory compliance in pharmaceutical manufacturing. The notion that a single vial of contaminated product can cause death is not merely plausible-it is empirically documented in multiple historical cases including the 1937 elixir sulfanilamide tragedy which killed over 100 people. The current cGMP framework exists precisely because the industry once operated without such constraints. To suggest that these halts are excessive is to ignore the fact that in 2018 alone, 17,000 patients were exposed to mislabeled or contaminated injectables. The cost of failure is measured in lives not in dollars. The technology described-digital twins AI inspection blockchain-is not innovation for innovation’s sake but a necessary evolution to reduce human error. The real crisis is not the halts but the public’s inability to comprehend why they are necessary.