Pharmacist Substitution: What It Means for Your Medications and Safety
When a pharmacist gives you a generic version of your prescription instead of the brand name, that’s pharmacist substitution, the practice of replacing a prescribed brand-name drug with a chemically identical generic version at the pharmacy level. Also known as drug substitution, it’s meant to cut costs—but not all substitutions are created equal. Some states force it, others leave it up to the pharmacist, and a few don’t allow it at all for certain drugs. This isn’t just paperwork—it can change how your body responds to treatment.
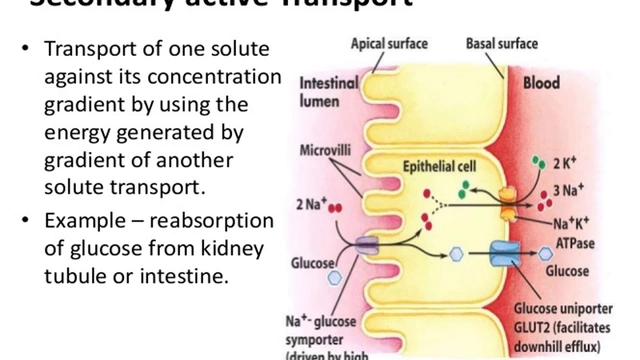
Not every drug plays nice when swapped. Therapeutic equivalence, the measure of whether two drugs produce the same clinical effect and safety profile is the gold standard. The FDA says most generics are fine, but for drugs with a narrow therapeutic index, a tiny difference in dose can cause serious harm or treatment failure, like digoxin or warfarin, switching between brands—even different generics—can throw your levels off. One pill might work fine. The next one, from a different maker, might not. That’s why some doctors write "do not substitute" on prescriptions.
Then there’s the legal side. Mandatory substitution, when state law requires pharmacists to swap brand for generic unless the doctor says no is common in many places. But permissive substitution, where the pharmacist can choose to swap but doesn’t have to, gives you more control—if you ask. Most people never know they got a different pill unless they check the label or notice side effects. And that’s the problem: if you’re on a tightrope with your meds, a silent switch can be dangerous.
It’s not just about cost. If you’ve had bad reactions to a generic before, or if your condition is unstable—like epilepsy, heart rhythm issues, or thyroid disease—you need to speak up. Pharmacists aren’t mind readers. They’ll swap unless you tell them not to. Keep a list of what works and what doesn’t. Bring it to every visit. Ask: "Is this the same as what I got last time?" That simple question can stop a chain reaction of side effects or treatment failures.
The posts below dive into real cases where substitution went wrong—like patients switching between digoxin generics and ending up in the ER, or people getting different versions of blood thinners and bleeding for no clear reason. You’ll also find how state laws vary, what to look for on the pill label, and how to protect yourself even when the system is designed to push you toward cheaper options. This isn’t theoretical. It’s about the pills you take every day—and whether they’re truly the same as the ones your doctor ordered.