When you walk into a pharmacy to pick up your prescription, you might not realize you have the legal right to say no. Pharmacists in many states are allowed to swap your brand-name medication for a cheaper generic version - even if your doctor didn’t ask for it. But you don’t have to accept that swap. You can refuse. And in some cases, you should.
What Is Generic Substitution?
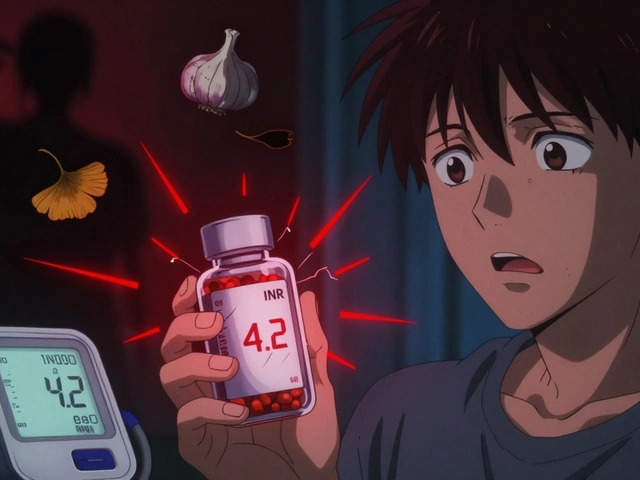
Generic substitution means a pharmacist gives you a drug with the same active ingredient as your prescription, but made by a different company. These generics are usually 80-85% cheaper than brand-name drugs. For many people, that’s a huge savings. But not all drugs are created equal.The FDA says generics must work the same way as brand-name drugs. And for most medications - like blood pressure pills or antibiotics - that’s true. But for drugs with a narrow therapeutic index (NTI), even tiny differences in how the body absorbs the drug can cause serious problems. Think levothyroxine for thyroid disease, seizure medications like phenytoin, or insulin. A small change in dosage can throw your whole system off.
That’s why some patients - especially those with chronic conditions - need to stick with the brand they know works. And the law lets them.
Your Legal Right to Say No
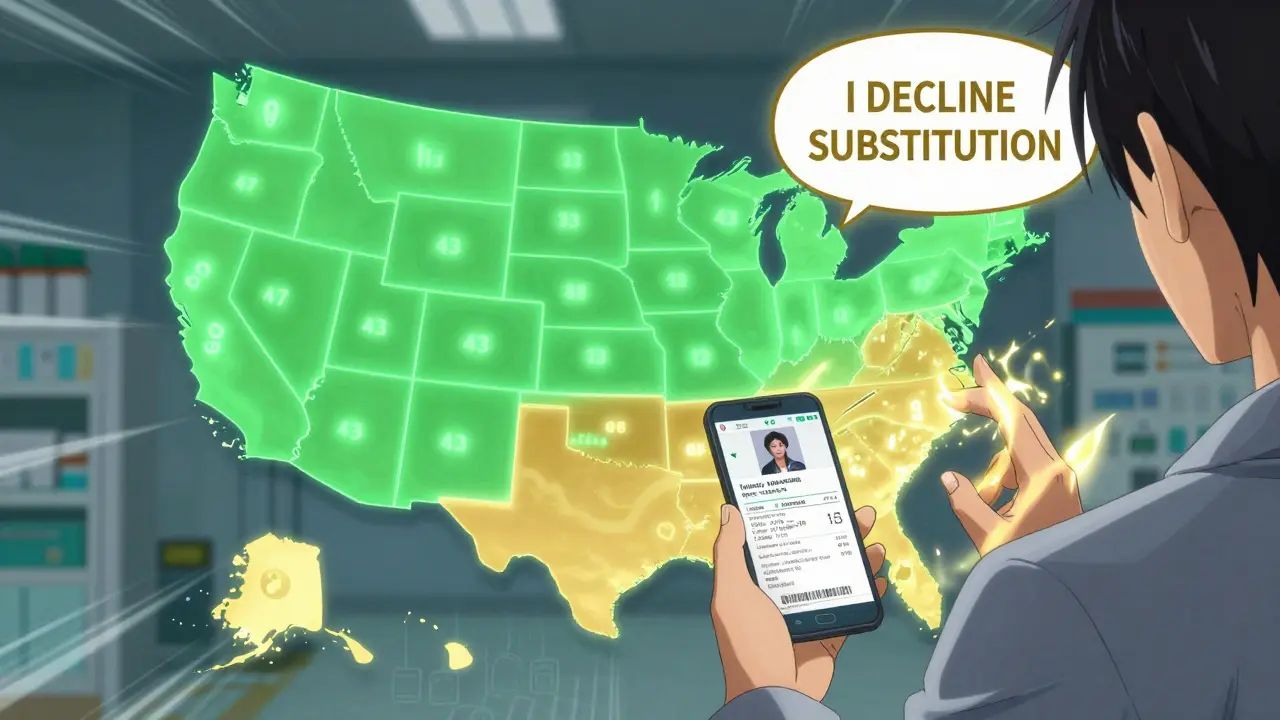
In 43 U.S. states, you can simply tell the pharmacist: “I decline substitution.” That’s it. No explanation needed. No paperwork. Just say it clearly at the counter.Some states go further. In seven states - Alaska, Connecticut, Hawaii, Maine, Massachusetts, New Hampshire, and Vermont - plus Washington, D.C., pharmacists must get your explicit permission before switching your medication. That means they can’t just hand you a generic unless you say yes.
And in 19 states, including California, Texas, and New York, pharmacists are required to substitute generics unless the doctor says otherwise. Even then, you still have the right to refuse. The law doesn’t take that away from you.
Here’s the catch: Not every pharmacist knows the rules. Some will tell you, “We have to switch it,” or “It’s cheaper for your insurance.” That’s not always true. If you’re told you can’t refuse, ask to speak to the manager. Cite your state’s law. Most pharmacies have a copy of their state’s substitution rules posted or available online.
When Brand-Name Drugs Are Medically Necessary
If you’ve had bad reactions to generics before - or if your doctor believes you need the brand - you can ask for a “dispense as written” or “brand medically necessary” note on your prescription.Forty-eight states legally recognize this notation. Your doctor writes it in the prescription, and the pharmacy must honor it. You don’t need to prove anything. You don’t need to file paperwork. Just ask your doctor to add it.
This is especially important for:
- Thyroid meds like Synthroid or Levoxyl
- Anti-seizure drugs like Lamictal or Dilantin
- Insulin products like Lantus or Humalog
- Immunosuppressants like cyclosporine
- Biosimilars (which aren’t true generics - more on that below)
A 2021 survey by Consumer Reports found that 28% of patients who tried to refuse substitution ran into pushback. Some pharmacists claimed they “had no choice.” That’s false. Others said refusing would cost you more. That’s often untrue too - especially after the 2018 Know the Lowest Price Act banned “gag clauses” that hid cash prices from patients.
Why Biosimilars Are Different
Biosimilars aren’t generics. They’re not even close.Generics are exact copies of small-molecule drugs. Biosimilars are copies of complex biological drugs - like those used for rheumatoid arthritis, cancer, or psoriasis. These drugs are made from living cells, not chemicals. Even tiny changes in manufacturing can affect how they work.
Forty-seven states now require pharmacists to notify your doctor if they switch you to a biosimilar. Only 38 states require them to tell you, the patient. That’s a gap. If you’re on a biologic, always ask: “Is this the brand or a biosimilar?”
The World Medical Association warns: Once you’re stable on a biologic, don’t switch without your doctor’s approval. There are documented cases of patients going from stable blood sugar levels to dangerous highs and lows after being switched to a biosimilar insulin without warning.
How to Protect Yourself
You don’t need to be a legal expert to protect your health. Here’s what to do:- Know your state’s law. If you live in Massachusetts, you can refuse without giving a reason. In Texas, you still can - but pharmacists may not tell you that.
- Say it clearly. At the counter: “I decline substitution.” Don’t say “I’d prefer” or “Can I get the brand?” Say “I decline.” That’s the legal phrase.
- Ask for the prescription label. Check the name on the bottle. If it’s not what your doctor prescribed, ask why.
- Get a “dispense as written” note. If you’re on a sensitive medication, ask your doctor to write it on the prescription.
- Keep records. Save your receipts. Take a photo of the label. If you have a bad reaction, you’ll need proof of what you were given.
- Call your state pharmacy board. If a pharmacist refuses to honor your right, file a complaint. All 50 states have a process for this.
Costs and Savings - What You Really Pay
Yes, generics save money. On average, you save $27.50 per prescription. But here’s the twist: Sometimes, paying cash for the brand is cheaper than using your insurance for the generic.Before the 2018 Know the Lowest Price Act, pharmacists couldn’t tell you that. Now they can. Always ask: “If I pay cash, how much would the brand cost?” You might be surprised.
Medicare Part D plans push generics harder than private insurers - 95% of their prescriptions are generic. But if you’re on a drug like Synthroid, that doesn’t mean you have to take the generic. Your plan still has to honor your refusal.
And remember: Non-medical switching - changing someone’s stable medication just to cut costs - costs the system $2.1 billion a year in extra doctor visits, ER trips, and hospitalizations. Your refusal isn’t just about you. It’s about preventing harm.
What to Do If You’re Switched Without Consent
If you find out you were switched to a generic or biosimilar without your knowledge - and you had a bad reaction - act fast.- Call your doctor. Tell them what happened.
- Call the pharmacy. Ask for the name of the drug you received. Request a copy of the dispensing record.
- File a report with the FDA’s MedWatch program. This helps track unsafe substitutions.
- Contact your state pharmacy board. They can investigate and fine the pharmacy.
In 2019, a Michigan patient suffered seizures after being switched to a different antiepileptic drug without consent. They sued the pharmacy and won. Your rights matter.
Final Advice: Be Your Own Advocate
You’re not being difficult. You’re being smart.Generic substitution saves billions. But it shouldn’t come at the cost of your health. If you’ve found a medication that works for you - especially for a chronic condition - you have the right to keep it.
Don’t wait until something goes wrong. Before your next refill, check your state’s substitution law. Talk to your doctor. Know your options. And when you go to the pharmacy, say it clearly: “I decline substitution.”
It’s your medicine. It’s your body. And the law is on your side.


Rachel Cericola
December 24, 2025I’ve been managing hypothyroidism for 12 years, and switching from Synthroid to a generic levothyroxine nearly sent me into cardiac arrest. My TSH went from 2.1 to 8.9 in three weeks. No one warned me. No one asked. I just got a different bottle with a different label. When I called the pharmacy, they said, ‘It’s the same thing.’ It’s not. Not when your body’s been stable on one formulation for over a decade. I now carry a printed copy of my state’s substitution law in my wallet. I say ‘I decline substitution’ every single time. No exceptions. If you’re on a narrow therapeutic index drug, don’t trust the system. Trust your body and your doctor. And if they push back? File a complaint. It’s not just about cost-it’s about survival.
Also, if you’re on insulin or antiseizure meds? Same rules. Don’t let anyone tell you it’s ‘just a generic.’ Your life isn’t a spreadsheet.
And yes, I’ve called my state pharmacy board three times. They’ve retrained three pharmacists because of me. You’re not being difficult. You’re being responsible.
And if your doctor won’t write ‘dispense as written’? Find a new doctor. Your health isn’t negotiable.
I’ve seen too many people get hurt because they didn’t know their rights. This post? Lifesaving. Thank you.
Also-always check the label. Always. Even if you’ve been getting the same pill for years. I once got a different generic because the bottle looked the same. It wasn’t. I had to go to the ER. Don’t be me.
And if you’re on Medicare Part D? They’ll try to force you. Don’t let them. You have rights. Use them.
I’m not mad. I’m just done being a guinea pig.
And yes, I’ve written to my congressman. They don’t respond. But I keep trying.
You’re not alone. I’ve started a support group for people who’ve been switched without consent. DM me if you want to join.
And if you’re reading this and you’re on Synthroid? Don’t wait until you feel weird. Say it now. ‘I decline substitution.’ Say it like you mean it.
Because your thyroid doesn’t care about corporate profits.
And neither should you.
claire davies
December 25, 2025As someone who moved from the UK to the US and had to navigate this mess, I can say with absolute certainty: this is a global issue dressed in American bureaucracy. In the NHS, generics are the default, but pharmacists are trained to flag NTI drugs automatically. Here? You’re expected to be your own pharmacist, lawyer, and advocate-all while juggling insurance forms and copays.
I once had to argue with a pharmacist in Ohio who swore ‘all thyroxine is the same.’ I showed him the FDA’s own guidelines on bioequivalence thresholds for levothyroxine. He looked at me like I’d spoken Latin. Then he called the manager. The manager knew the law. But the pharmacist? He didn’t. That’s the problem.
And biosimilars? Oh, honey. In the UK, we call them ‘biological medicines’ and treat them like heart transplants-no swapping unless you’ve got a full clinical review. Here? You get a label change and a shrug.
I’ve started handing out laminated cards at my local pharmacy: ‘I decline substitution. My doctor wrote DAW 1. Thank you.’ It’s polite. It’s firm. It works.
Also-never trust the ‘cash price’ spiel. I paid $12 cash for my brand-name insulin last month. My insurance copay for the ‘generic’ was $47. Because of tiering. Because of formularies. Because the system is designed to confuse you.
Keep saying no. Keep asking. Keep documenting. You’re not just protecting yourself-you’re pushing the system to be better.
Katie Taylor
December 26, 2025My mom got switched to a generic seizure med and had a grand mal in her kitchen. She’s fine now, but she had to be airlifted. The pharmacy didn’t even tell her it was a different brand. They just handed her the bottle. I’m so pissed I could scream. This isn’t about money. It’s about people dying because someone thought ‘close enough’ was good enough.
Stop letting them do this. Say ‘I decline substitution.’ Say it like you mean it. And if they give you grief? Tell them you’ll report them to the state board. Then do it. I did. They got fined. It felt good.
Also-your doctor needs to write ‘dispense as written’ on the prescription. Don’t let them say ‘oh, it’s not necessary.’ It is. It’s life or death.
And if you’re on insulin? Don’t even joke about switching. I’ve seen the numbers. People go into DKA because they got a different batch. It’s not a myth. It’s a pattern.
Be loud. Be angry. Be unapologetic. Your life matters more than a 27-dollar savings.
Isaac Bonillo Alcaina
December 28, 2025Let’s be clear: this post is dangerously oversimplified. The FDA’s bioequivalence standards for generics are not arbitrary-they’re statistically validated. The notion that ‘small differences’ in absorption cause catastrophic outcomes is largely anecdotal and rarely supported by controlled trials. Yes, there are outliers. But conflating those with systemic failure is fearmongering.
And let’s not forget: 95% of patients do just fine on generics. The fact that you’re one of the 5% who react poorly doesn’t mean the system is broken-it means you’re an outlier. And outliers don’t dictate policy.
Also, the claim that pharmacists are ‘ignorant’ of the law? Most are trained on state-specific substitution rules. If they’re not, it’s a training failure, not a conspiracy.
And ‘dispense as written’? That’s a legitimate tool-but it’s meant for documented clinical intolerance, not preference. If your doctor writes it for ‘brand loyalty,’ that’s not medical-it’s consumerism.
Don’t confuse your personal experience with universal truth. The system works for millions. Don’t let your anxiety dismantle it for everyone else.
And while we’re at it: the ‘cash price cheaper than insurance’ thing? That’s a loophole, not a right. You’re gaming a broken pricing system. That’s not advocacy. That’s exploitation.
And biosimilars? They’re not ‘different.’ They’re just more complex. And yes, they’re regulated. The FDA doesn’t approve them on a whim.
Stop treating every pharmacy visit like a life-or-death courtroom drama. Most people don’t need this level of paranoia. Most people just need their meds.
And if you’re keeping photos of labels and filing complaints for every switch? You’re not a patient. You’re a litigant.
Sidra Khan
December 28, 2025I just got my generic thyroid med and didn’t even notice. 🤷♀️
Ademola Madehin
December 29, 2025Bro, I got switched to a generic insulin and my sugar went to 480. I called the pharmacy and they said ‘it’s the same chemical.’ I said ‘then why did I almost die?’ They hung up.
Then I called my doctor. He said ‘I didn’t write that.’ So I called the FDA. Then I called the state board. Then I called the governor’s office. Then I posted a TikTok. Now the pharmacy got shut down for 3 days.
They thought I was just some dude. I’m not. I’m the guy who made them scared to touch your meds again.
And now my whole block knows to say ‘I decline substitution.’
They think it’s a joke. It ain’t.
They think it’s about money. Nah. It’s about not waking up in the ER again.
And if you’re not screaming at your pharmacist? You’re not trying.
They don’t care until you make them care.
And I’m still waiting for my $5000 reimbursement. They haven’t paid. But I’m not done.
They think they can hide behind ‘policy.’ I’m the policy now.
Andrea Di Candia
December 30, 2025It’s interesting how this issue reveals so much about our healthcare system: we treat patients like customers, not people. We optimize for cost, not care. We assume compliance without understanding biology. We let pharmacists make clinical decisions without training them to recognize the nuances of NTI drugs.
But here’s the thing-this isn’t just about levothyroxine or insulin. It’s about trust. Do we trust the system to protect us? Or do we have to fight for every pill?
I used to think generics were a win. Now I see them as a symptom of a deeper problem: healthcare commodification.
And I get it-costs are insane. But if we keep sacrificing safety for savings, we’ll end up spending more on ER visits, hospitalizations, and lost productivity. The $2.1 billion stat? That’s not a cost of refusal. That’s a cost of indifference.
Maybe the real question isn’t ‘Can I refuse?’
It’s: ‘Why do I have to?’
And why is it on me, the patient, to be the expert on bioequivalence thresholds and state pharmacy laws?
Why isn’t it on the system to just… get it right?
I’m not angry. I’m just tired.
And I’m grateful for this post. Because it’s a small step toward making the invisible visible.
Maybe one day, ‘I decline substitution’ won’t be a battle cry.
Maybe it’ll just be standard practice.
CHETAN MANDLECHA
January 1, 2026From India, where generics are the norm and brand-name drugs are luxury items. We don’t have the luxury of refusing. My uncle took a generic antiepileptic and had a seizure during a family wedding. We didn’t know it was a switch. No one told us. No one asked.
Here, doctors write ‘dispense as written’-but pharmacists ignore it. Insurance? Doesn’t exist for most.
So I read this post and I’m torn. I’m glad you have rights. I’m sad that most of the world doesn’t.
Maybe the real fight isn’t just about substitution.
It’s about equity.
Because if you can afford to say ‘no,’ you’re already ahead of 90% of the world.
So thank you for speaking up.
And if you ever come to India, bring extra Synthroid. We’ll pay you in chai and gratitude.
Harsh Khandelwal
January 1, 2026They’re using this to push you into the biometric surveillance system. Did you know that every time you refuse a generic, the pharmacy logs your refusal and sends it to a health data broker? They’re building profiles on ‘medication non-compliance’ and selling them to insurers. Next thing you know, your premiums go up because you ‘refuse cost-saving measures.’
And the ‘dispense as written’ note? That’s just a backdoor for Big Pharma to lock you in. They pay doctors to write it. That’s why your doctor won’t refuse. They’re getting kickbacks.
And the FDA? They’re owned by the same people who make the generics. That’s why they say ‘bioequivalent.’ It’s not true. It’s a legal loophole.
They want you to think you have a choice. You don’t. You’re just being manipulated into thinking you’re fighting the system.
Meanwhile, the real villains? The pharmacy chains that profit from the switch. They get rebates from generic manufacturers. Every time you say ‘I decline,’ they lose money.
So they make you feel guilty. They call you ‘difficult.’
But you’re not. You’re awake.
And if you think this is about your thyroid? Think again.
This is about data. Control. Profit.
They don’t care if you live or die.
They care if you click ‘accept’ on the next screen.
So say ‘I decline substitution’ all you want.
But know this: you’re still being tracked.
And they’re still winning.