Pharmaceutical Manufacturing: How Drugs Are Made and Why It Matters
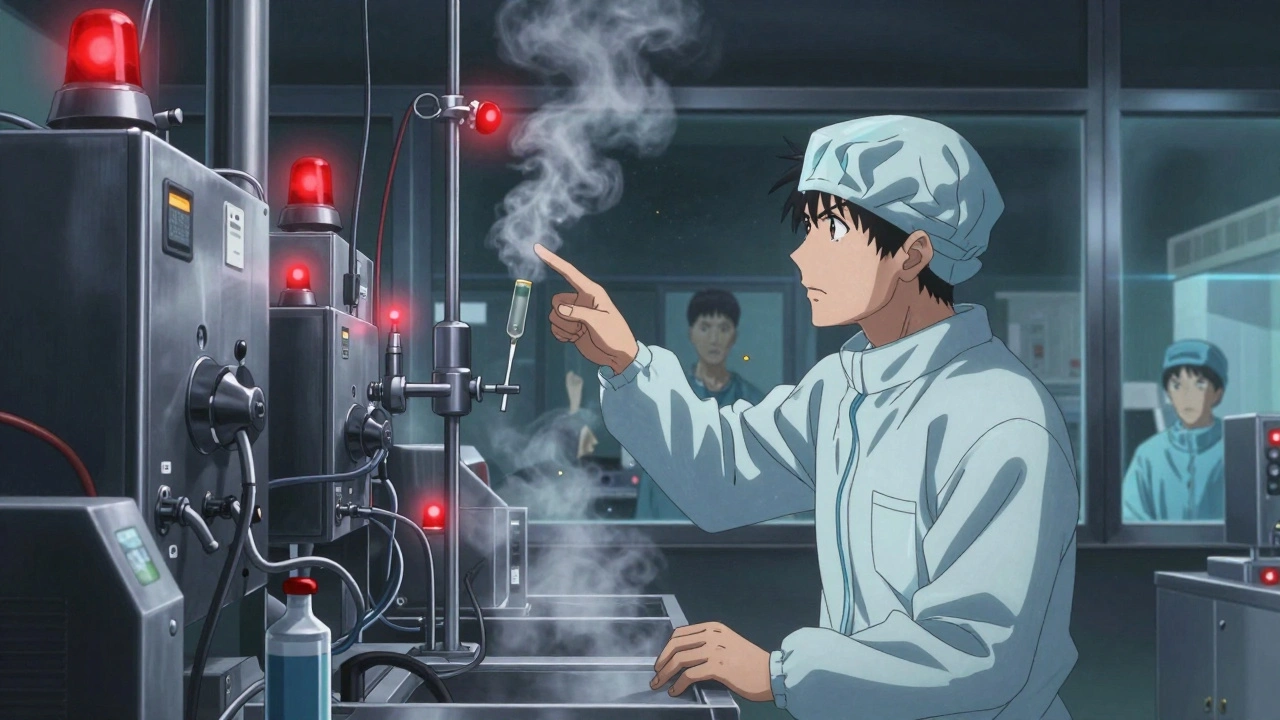
When you take a pill, you’re trusting a complex process called pharmaceutical manufacturing, the end-to-end process of producing medications from raw ingredients to finished dosage forms under strict regulatory standards. Also known as drug production, it’s not just about mixing powders—it’s about control, consistency, and safety at every step. This process determines whether your medicine works the same way every time, whether it’s safe to switch brands, and even if you’re getting what you paid for.
Generic drugs, lower-cost versions of brand-name medications approved by the FDA as therapeutically equivalent, rely entirely on how well they’re made. Two pills may have the same active ingredient, but if the manufacturing process changes the way the drug dissolves in your body—known as bioavailability, the rate and extent to which the active drug enters circulation—your treatment can fail. That’s why drugs like digoxin, with a narrow therapeutic index, demand extreme precision. A small change in manufacturing can mean the difference between healing and poisoning.
Therapeutic equivalence, the legal and clinical standard that ensures generics perform the same as brand-name drugs isn’t just a label—it’s the result of hundreds of tests on dissolution rates, particle size, and excipients. But not all manufacturers follow the same standards. Some cut corners to save money, leading to pills that don’t break down properly or contain inconsistent doses. This is why switching between different generic brands can cause problems, especially with blood thinners, seizure meds, or thyroid drugs.
Pharmaceutical manufacturing also affects safety. Counterfeit pills sold online often come from unregulated factories with no quality checks. They might contain fentanyl, too much or too little of the real drug, or even toxic chemicals. The same risks exist in legal supply chains when oversight slips. That’s why the FDA inspects factories globally—and why you should only buy from licensed pharmacies.
It’s not just about the science. The way drugs are made affects cost, access, and even your doctor’s prescribing choices. If a generic is cheaper but unreliable, your doctor might stick with the brand—even if it’s out of reach for you. And when manufacturing shifts overseas, supply chains get fragile. Shortages happen not because of demand, but because one factory had a contamination issue or failed an inspection.
What you’ll find below are real stories from people who’ve been affected by these invisible differences in drug quality. From pharmacists who catch dangerous substitutions, to patients who got sick after switching generics, to experts explaining why your insulin or blood pressure med might not work the same way after a refill. These aren’t theoretical concerns—they’re everyday risks hidden in plain sight.