
Every year, millions of people take supplements-vitamins, herbs, probiotics, fish oil-thinking they’re harmless because they’re "natural." But here’s the truth: supplements and food can interfere with your prescription meds in ways that are dangerous, even deadly. You might be taking St. John’s wort for low mood, grapefruit juice for heart health, or calcium pills for bones, but if you’re also on blood thinners, antidepressants, or cholesterol drugs, you could be risking serious side effects. And most people never tell their pharmacist.
Why Your Pharmacist Is the Best Person to Ask
Pharmacists are the most accessible healthcare professionals in your community. In Australia, 93% of people live within five kilometers of a pharmacy. Unlike doctors who see you for 10 minutes once a year, your pharmacist sees you every time you pick up a script. They know your full medication list. They’ve seen what happens when people mix supplements with prescriptions. The problem? Most patients don’t bring it up. A 2025 study found that only 6.7% of pharmacists were ever asked about supplement interactions by their patients. That means the vast majority of risks go unnoticed-until something goes wrong. Your pharmacist doesn’t just fill prescriptions. They’re trained to spot hidden dangers. They know that goldenseal can make your blood pressure meds stop working. That St. John’s wort can trigger serotonin syndrome when mixed with antidepressants. That grapefruit can turn your statin into a toxic dose. These aren’t myths. These are documented, life-threatening interactions.What Supplements Are Most Likely to Cause Problems
Not all supplements are risky. But some carry serious interaction potential. Here are the big ones:- St. John’s wort: Used for mild depression, but it can cut the effectiveness of birth control, blood thinners, HIV meds, and antidepressants. It’s one of the most dangerous supplements out there. It can cause serotonin syndrome-a rare but fatal condition.
- Goldenseal: Often taken for colds or digestion, but it interferes with how your liver processes over 50 medications, including blood pressure drugs, antidepressants, and diabetes pills.
- Ginkgo biloba: Popular for memory, but it can increase bleeding risk when taken with aspirin, warfarin, or clopidogrel. Even a minor cut could become serious.
- Milk thistle: Commonly used for liver support, but it can affect how your body metabolizes statins, antipsychotics, and some cancer drugs.
- Cranberry: Often thought to help prevent UTIs, but it can boost the effect of warfarin, raising your risk of internal bleeding.
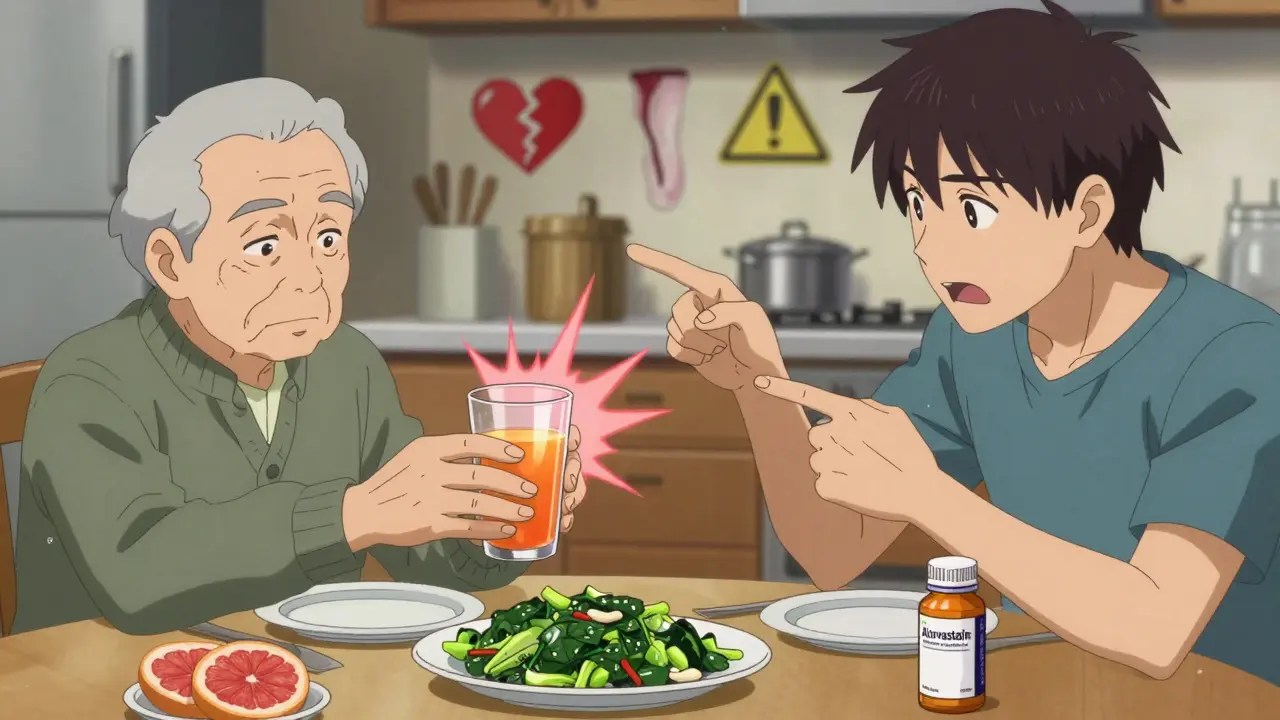
Food Interactions You Can’t Ignore
It’s not just pills. What you eat matters too.- Grapefruit and citrus fruits: One grapefruit can change how your body handles more than 85 medications. Statins (like atorvastatin), blood pressure drugs (like felodipine), and some anti-anxiety meds (like buspirone) can become dangerously potent. The effect lasts up to 72 hours. No amount of timing fixes it-just avoid it entirely.
- Dairy products: Calcium in milk, yogurt, and cheese can block absorption of antibiotics like ciprofloxacin and doxycycline. It also interferes with thyroid meds like levothyroxine. The fix? Wait at least 2-4 hours between taking these meds and eating dairy.
- Leafy greens: Spinach, kale, broccoli-packed with vitamin K. If you’re on warfarin, your vitamin K intake needs to stay consistent. One week eating tons of greens, then switching to salads? Your INR can swing wildly. Your pharmacist will help you find a balance.
- Alcohol: It doesn’t just interact with painkillers. It can worsen liver damage from acetaminophen, increase drowsiness from benzodiazepines, and spike blood pressure when mixed with certain antidepressants.

How to Prepare Before Your Visit
Going in unprepared is the biggest mistake people make. Here’s how to get it right:- Write down everything. Not just your prescriptions. Include every supplement, herb, vitamin, protein powder, and even over-the-counter products like melatonin or laxatives. Include brand names, doses, and how often you take them.
- Track your diet. Do you drink grapefruit juice every morning? Eat a spinach smoothie daily? Have a glass of wine with dinner? Note it. Your pharmacist needs to know your routine.
- Bring the bottles. Pictures of labels aren’t enough. Bring the actual containers. Pharmacists check ingredients, fillers, and dosages. Many supplements don’t even contain what’s on the label.
- Ask specific questions. Don’t say, “Is this safe?” Say: “I’m on warfarin. Is this ginkgo supplement going to make me bleed?” Or: “I take metformin. Will magnesium supplements affect my B12 levels?”
What Your Pharmacist Will Do for You
A good pharmacist won’t just say “yes” or “no.” They’ll dig deeper. Here’s what to expect:- They’ll check your entire list against drug interaction databases. These systems flag over 1,000 known interactions between supplements and meds.
- They’ll tell you if timing matters. For example: take your thyroid med first thing in the morning on an empty stomach, then wait 3-4 hours before eating or taking calcium.
- They’ll warn you about nutrient depletion. Proton pump inhibitors (like omeprazole) drain your B12 and magnesium. Metformin lowers B12 and folate. Statins reduce CoQ10-linked to muscle pain. Your pharmacist can recommend safe replacements.
- They’ll suggest verified brands. The FDA doesn’t test supplements before they hit shelves. But third-party groups like USP, NSF, and ConsumerLab do. Your pharmacist knows which brands actually contain what they claim.
What to Do If You’ve Already Had a Bad Reaction
If you’ve felt dizzy after taking a supplement with your blood pressure pill. If you’ve had unexplained bruising after starting ginkgo. If your anxiety got worse after adding St. John’s wort-stop immediately. Don’t wait for your next appointment. Call your pharmacist. Or go to the nearest pharmacy. Bring your meds and the supplement. They can assess whether you need urgent care. Many pharmacies now have private consultation rooms where you can talk without embarrassment. And if you’ve been told by a friend, a YouTube video, or a wellness influencer that a supplement is “safe”-remember this: they’re not trained in pharmacology. Your pharmacist is.Why This Matters More Than Ever
The supplement market in Australia is growing fast. More people are using them, especially older adults. But regulation hasn’t kept up. In 2025, a major pharmacy chain in Melbourne started integrating supplement interaction alerts into their dispensing software. That’s progress. But it’s not enough. You have to be your own advocate. If your pharmacist doesn’t ask about supplements, ask them. Say: “I take a few supplements. Can we check if they’re safe with my meds?” The truth is, your pharmacist wants to help. They’re not judging you. They’ve seen it all-from people taking turmeric with blood thinners to those drinking green tea with antidepressants. They’ve helped fix mistakes. They can help you avoid them.Final Tip: Don’t Stop Anything Without Talking
Some people, once they learn a supplement interacts with their meds, just quit cold turkey. That’s risky too. Suddenly stopping a supplement-or a medication-can cause withdrawal, rebound symptoms, or worsening conditions. Always talk to your pharmacist first. They’ll help you taper safely, swap out risky products, or adjust doses. You don’t have to choose between feeling better and staying safe. You can do both.Can I take supplements with my prescription medications?
Some can, but many can’t. Supplements like St. John’s wort, goldenseal, and ginkgo can interfere with blood thinners, antidepressants, and heart medications. Even common ones like calcium and vitamin K can affect how your drugs work. Always check with your pharmacist before starting any supplement.
Do I need to tell my pharmacist about vitamins and herbal teas?
Yes. Vitamins, herbal teas, and even protein powders can interact with medications. For example, green tea can reduce the effectiveness of some blood pressure drugs. Vitamin B6 can interfere with Parkinson’s meds. Your pharmacist needs the full picture-even if it seems minor.
Is it safe to take supplements at the same time as my pills?
Timing matters. Calcium and iron supplements should be taken at least 2-4 hours apart from antibiotics and thyroid meds. Grapefruit juice should be avoided entirely if you’re on statins or certain blood pressure drugs. Your pharmacist can give you a personalized schedule.
How do I know if a supplement brand is safe?
Look for third-party verification labels: USP, NSF, or ConsumerLab. These mean the product was tested for ingredients, potency, and contamination. The FDA doesn’t test supplements before they’re sold, so these labels are your best protection.
Can supplements replace my medication?
No. Supplements are not substitutes for prescribed medication. While some, like omega-3s or magnesium, may support health, they won’t treat conditions like high blood pressure, diabetes, or depression the way your meds do. Never stop your prescription without talking to your pharmacist or doctor.
What if my pharmacist says a supplement is fine, but my doctor says no?
That’s a red flag. Pharmacists and doctors should be on the same page. Ask both to talk to each other. Your pharmacist can contact your doctor directly to clarify. Don’t let conflicting advice leave you confused-get them to coordinate.
Are there supplements that are generally safe?
Some have low interaction risk when taken correctly, like vitamin D (if you’re not on high-dose steroids), vitamin C, and most B-complex vitamins. But even these can interfere if you’re on certain drugs. Always confirm with your pharmacist-even the "safe" ones.
Can food interactions be avoided just by timing?
Sometimes. For example, taking your thyroid pill on an empty stomach and waiting 4 hours before eating dairy helps. But with grapefruit, timing doesn’t help-it’s the compound in the fruit that stays in your system for days. Avoid it completely if you’re on a statin or certain blood pressure meds.
How often should I review my supplements with my pharmacist?
Every time you get a new prescription, or every 6 months if your meds haven’t changed. Supplement use changes often-people start and stop based on trends. Your pharmacist needs to know what’s in your cabinet right now.
Do pharmacists get paid to recommend certain supplements?
No. Pharmacists are not paid commissions to push specific brands. Their goal is your safety. They recommend verified products based on science, not profit. If they suggest a supplement, it’s because they’ve checked the interactions and know it’s appropriate for your situation.
Supplements aren’t the enemy. But treating them like harmless candy is. Your pharmacist is your best line of defense against dangerous interactions. Take the time to talk to them. Bring your bottles. Ask the hard questions. It’s not just about avoiding side effects-it’s about making sure your meds work the way they’re supposed to.



Angel Molano
January 14, 2026St. John’s wort with SSRIs? That’s not a risk-it’s a death sentence waiting to happen. People treat supplements like candy because they’re ‘natural.’ Natural doesn’t mean safe. It means unregulated, untested, and often lethal.
Kimberly Mitchell
January 15, 2026The pharmacological literature on herb-drug interactions is overwhelmingly consistent, yet public health messaging remains catastrophically inadequate. The FDA’s regulatory gap for dietary supplements constitutes a systemic failure of pharmacovigilance, and the onus is placed entirely on the layperson to navigate a minefield of documented CYP450-mediated metabolic interference.
Vinaypriy Wane
January 16, 2026I understand people want to feel better… but please, for the love of everything holy, stop self-prescribing like you’re on a wellness podcast. I’ve seen a 72-year-old man end up in ICU because he mixed turmeric with warfarin and thought ‘it’s just spice.’ It’s not. It’s pharmacology. Talk to your pharmacist. Please.
Diana Campos Ortiz
January 17, 2026My grandma started taking ginkgo after reading it ‘boosts memory’-then she started bruising like a grape. Took her to the pharmacy, they checked her meds, and boom-warfarin interaction. She’s fine now. But she didn’t know. Nobody tells you this stuff. Your pharmacist isn’t just a person who hands you pills-they’re your safety net.
Robin Williams
January 17, 2026Look. We’re all trying to fix ourselves with potions and powders because the system’s broken. But the truth? Your body isn’t a video game where you stack buffs. You can’t ‘supplement’ your way out of a broken healthcare system. But you *can* stop being lazy and ask your pharmacist. Just ask. It’s not hard.
Scottie Baker
January 18, 2026I used to take St. John’s wort for my anxiety. Thought it was ‘natural therapy.’ Then I got serotonin syndrome. Ended up in the ER. My pharmacist was the only one who knew what happened. The doctor? Didn’t even ask about supplements. Don’t be like me. Bring the bottles. Talk to them. They’ve seen worse.
Anny Kaettano
January 19, 2026Let’s normalize asking your pharmacist about supplements like it’s as routine as asking if your prescription has generics. They’re the unsung heroes of medication safety. They don’t get paid extra. They don’t get applause. But they’ve saved more lives than most doctors ever will-just by listening. So next time you pick up your meds, say: ‘Hey, I’m taking this too. Is it safe?’ It’s that simple.
Pankaj Singh
January 20, 2026‘Grapefruit interferes with 85 drugs’? That’s not a warning-that’s a corporate liability nightmare. The fact that this isn’t federally mandated on every supplement bottle says everything about how little we value public safety. And don’t get me started on ‘natural’ labels. If it’s not FDA-approved, it’s a gamble. And you’re the sucker.
Jesse Ibarra
January 21, 2026You people are so naive. You think your ‘organic’ ashwagandha is harmless? It’s not. It’s a chemical compound with pharmacokinetic properties that interact with your liver enzymes. And you’re reading about it on Instagram. Meanwhile, your pharmacist has access to Micromedex, Lexicomp, and clinical databases that track 10,000+ interactions. You’re not ‘wellness warriors.’ You’re walking drug interaction case studies.
laura Drever
January 22, 2026supplements r just expensive urine anyway lmao
Randall Little
January 24, 2026Interesting how the U.S. lets supplements fly under the radar while Europe and Canada regulate them as medicines. It’s not about safety-it’s about capitalism. The supplement industry spends more on lobbying than on research. Your ‘natural remedy’? It’s a profit center. Your pharmacist? The only one who’s not getting paid to sell you snake oil.
Rosalee Vanness
January 25, 2026When I first started taking metformin, I had no idea that magnesium could mess with my B12 absorption-or that my daily protein shake with added zinc might be making my neuropathy worse. I didn’t know to ask. I just thought ‘more vitamins = better.’ Then I sat down with my pharmacist, brought every bottle, and she spent 20 minutes going through each one. She didn’t judge me. She just said, ‘Here’s what’s actually helping you, and here’s what’s just empty calories.’ I cried. Not because I was scared-but because someone finally saw me as a person, not a prescription list. Don’t be afraid to do the same. They’re not here to scold you. They’re here to help you live.
Trevor Davis
January 27, 2026Look, I used to think pharmacists were just glorified cashiers. Then my dad had a stroke. His meds were a mess-blood thinners, statins, antihypertensives. We brought his supplement cabinet to the pharmacy. Turned out he was taking CoQ10 for his heart… which was neutralizing his statin. The pharmacist rewrote his entire regimen, flagged the interactions, and even called his cardiologist to sync up. That’s not a job. That’s a lifeline. And it’s free. Why don’t we treat it like one?
James Castner
January 28, 2026The philosophical underpinning of this entire issue lies in the epistemological dissonance between consumer autonomy and scientific epistemic authority. We live in an age where anecdotal evidence, amplified by social media algorithms, is granted equal epistemic weight as peer-reviewed pharmacokinetic data. This is not merely a public health crisis-it is a crisis of epistemic humility. The pharmacist, as the custodian of evidence-based pharmacological knowledge, occupies a uniquely accessible, non-hierarchical position within the healthcare ecosystem. To dismiss their expertise is not merely ignorance-it is a rejection of rationality itself. The burden of epistemic responsibility does not rest with the physician, the regulator, or the manufacturer. It rests with the individual who chooses to ingest substances without verifying their pharmacodynamic compatibility. We must reclaim the sacred space of informed consent-not as a legal formality, but as a moral imperative.