When you’re managing a chronic condition like rheumatoid arthritis, Crohn’s disease, or cancer, the cost of treatment can be just as stressful as the illness itself. Biologic drugs - powerful, targeted therapies made from living cells - have changed lives. But they’re expensive. That’s where biosimilars come in. They’re not generics. They’re not copies. They’re highly similar versions of these complex drugs, designed to work the same way with no meaningful difference in safety or effectiveness. The big question on everyone’s mind: Do they really work as well? The answer isn’t speculation. It’s data.
What Exactly Is a Biosimilar?
Think of a biologic drug like a handmade watch. It’s not assembled from simple parts. It’s built using living cells, grown in controlled environments, and shaped by complex biological processes. Even small changes in temperature, pH, or nutrients can alter the final product. That’s why you can’t just copy it like a pill.
A biosimilar is made to match the original biologic - called the reference product - as closely as possible. It’s not identical, because biological products can’t be perfectly replicated. But it’s close enough that any differences don’t affect how it works in your body. Regulatory agencies like the FDA and EMA require over 200 analytical tests to prove this. They look at structure, function, purity, and stability. Then they run tests in animals and humans to confirm safety and effectiveness.
It’s not a shortcut. It’s a science-heavy path. The first biosimilar approved in the U.S. was Zarxio in 2015, a version of Neupogen used to boost white blood cells after chemotherapy. Since then, 37 biosimilars are available in the U.S., and over 100 in Europe.
Do Biosimilars Work as Well in Real Patients?
Let’s cut through the noise. Do patients get the same results? Yes. Multiple large studies confirm it.
In a 2016 randomized trial called NOR-SWITCH, 480 patients with cancer, rheumatoid arthritis, or inflammatory bowel disease were switched from the original rituximab to its biosimilar. After 52 weeks, there was no difference in disease control. The response rate was nearly identical: 72.9% for the original, 69.3% for the biosimilar. The difference? Statistically meaningless.
A 2022 meta-analysis looked at 1,711 patients across six cancer types. For every biosimilar tested - bevacizumab, trastuzumab, rituximab - the overall response rates were within 1% of the reference drug. Confidence intervals? All crossed 1.0. That means no real difference.
In inflammatory bowel disease, a Canadian study tracked 1,200 patients for two years. Those on the infliximab biosimilar (CT-P13) had the same rates of remission, hospitalization, and treatment persistence as those on the original. No spikes in side effects. No drop in effectiveness.
Even in rheumatoid arthritis, where patients are sensitive to changes in treatment, a real-world study of 3,450 patients across Europe found no difference in drug survival at 12 months. Eighty-two percent of people stayed on the biosimilar. So did 81.7% on the original. The difference? Not significant.
What About Safety? Are Biosimilars Riskier?
The biggest fear? Immunogenicity - your body developing antibodies against the drug. That could make it less effective or cause allergic reactions. It’s a valid concern. Biologics are complex, and tiny structural changes could trigger an immune response.
But real-world evidence doesn’t support that fear. A 2023 report from NHS England followed 12,000 patients switched from rituximab to its biosimilar for non-Hodgkin’s lymphoma. No increase in infusion reactions. No rise in serious infections. No unexpected side effects.
On PatientsLikeMe, 1,245 people using the adalimumab biosimilar Amjevita reported symptom control identical to those on Humira. Adverse events? Exactly the same rate: 23%. In a survey by the Arthritis Foundation, 92% of patients switched from infliximab to Inflectra said their disease control didn’t change. Six percent even felt better. Only 2% felt worse - and their doctors couldn’t confirm it was the biosimilar’s fault.
Experts agree. Dr. G. Caleb Alexander from Johns Hopkins said, “The totality of evidence from over 100 biosimilars approved globally demonstrates no clinically meaningful differences.” The International Society for Pharmacoeconomics and Outcomes Research reviewed over 300 real-world studies involving half a million patients and concluded the same.
That said, long-term data beyond five years is still limited for some biosimilars. That’s why ongoing monitoring is required. But so far, no red flags.

Why Do Some Doctors Still Hesitate?
Despite the evidence, a 2021 survey found 38% of U.S. physicians still had concerns about biosimilar efficacy. Why? Misinformation. Lack of familiarity. Fear of liability.
Some think, “If it’s cheaper, it must be worse.” But cost doesn’t equal quality. Biosimilars are cheaper because they don’t need to repeat the original 10-year, $1 billion development process. They build on proven science.
Others worry about switching. “What if my patient does fine on Humira - why risk changing?” But studies show switching back and forth between biosimilars and reference products doesn’t harm outcomes. A 2023 study even showed patients who switched between two different adalimumab biosimilars had the same retention rate as those who stayed on one.
And here’s something surprising: 84% of biosimilar trials were double-blinded. That means neither patients nor doctors knew who got what. Meanwhile, only 17% of original biologic trials were. So the evidence for biosimilars is actually more rigorously tested.
How Are Biosimilars Being Used in Practice?
Implementation matters. A biosimilar won’t help if no one uses it.
In Europe, biosimilar adoption is high. For filgrastim, over 80% of prescriptions are for biosimilars. In the U.S., uptake varies by specialty. Rheumatology leads at 78%. Gastroenterology is at 65%. Oncology lags at 31% - partly because oncologists are cautious, and partly because drug manufacturers use tactics like “product hopping” to delay competition.
Successful programs follow clear steps:
- Provider education - 100% of health systems that adopted biosimilars trained their staff.
- Patient counseling - 93% used clear, simple materials to explain the switch.
- Electronic alerts - 87% set up EHR prompts to remind doctors and pharmacists.
Kaiser Permanente reduced patient refusal from 22% to just 5% by using standardized talking points. Pharmacies now have state-specific rules on whether they can switch a prescription automatically - 48 states have laws, with 53 different rules. Pharmacists need training. Prescribers need to know the FDA’s Purple Book, which lists all approved biosimilars and their reference products.

How Much Do They Save?
Cost is the biggest driver. In the U.S., biosimilars are priced 15-30% lower than the original. In Europe, savings are even bigger - 25% to 85% depending on the drug and market competition.
The Congressional Budget Office estimates biosimilars will save the U.S. healthcare system $169 billion over the next decade. Medicare Part B alone saved $1.3 billion in one year just from biosimilar competition.
That’s not just money. It’s access. A patient who couldn’t afford Humira might now get Amjevita. A family might not have to choose between rent and treatment. A hospital might fund more cancer screenings because they’re spending less on biologics.
What’s Next for Biosimilars?
The future is moving fast. The FDA is proposing to eliminate the requirement for clinical trials if analytical and pharmacokinetic data prove similarity. That’s a big shift - and it’s backed by evidence from eight completed studies showing no meaningful differences without additional human trials.
Companies are also developing biosimilars of biosimilars. Switching between two different adalimumab biosimilars? No problem. A 2023 study showed retention rates were nearly identical - 84.2% for those who switched multiple times, 85.7% for those who didn’t.
Patent thickets and legal delays still slow things down. But the trend is clear: biosimilars are here to stay. And the data says they work.
Bottom Line: Do Biosimilars Work as Well?
Yes. Not maybe. Not sometimes. They work as well.
The evidence isn’t just from labs. It’s from real people - thousands of them - living with chronic illness. It’s from hospitals saving millions. It’s from doctors who’ve switched their patients and seen no drop in outcomes.
Biosimilars aren’t a compromise. They’re a breakthrough. They bring the power of biologic therapy within reach for more people, without sacrificing safety or effectiveness. If your doctor suggests switching, ask for the data. You’ll find it’s solid.


Crystel Ann
January 16, 2026The data is overwhelming, and it’s reassuring to see real patients doing just as well on biosimilars. I’ve seen friends switch from Humira to Amjevita and not miss a beat. No drama, no flare-ups, just lower bills and same relief. It’s not magic-it’s science working the way it should.
Nat Young
January 18, 2026Let’s be real-this whole ‘no meaningful difference’ narrative is corporate propaganda. The FDA approves biosimilars based on statistical noise, not biological truth. You can’t replicate a living molecule with perfect fidelity, and pretending otherwise is dangerous. I’ve seen patients crash after switching-silent immunogenicity doesn’t show up in 52-week trials.
Niki Van den Bossche
January 19, 2026Oh, the poetry of biologics-tiny, trembling proteins born in bioreactors like celestial symphonies, each glycosylation pattern a whispered secret from the gods of cellular alchemy. And now we dare to clone them? To reduce the sacred to a spreadsheet of equivalence metrics? Biosimilars are not mere substitutes-they are echoes in a cathedral of complexity, and to treat them as interchangeable is to misunderstand the very essence of life’s fragility.
Iona Jane
January 21, 2026They’re testing this on us because Big Pharma wants to kill the original drugs. You think they care about savings? No. They’re running a slow genocide on chronic patients by replacing proven treatments with cheaper knockoffs. The FDA is compromised. The studies? Funded by the same companies that profit from biosimilars. Wake up.
Jaspreet Kaur Chana
January 22, 2026Bro, in India we’ve been using biosimilars for over a decade-infliximab, rituximab, everything. My uncle had RA and switched to a biosimilar, saved 80% on meds, still plays cricket at 68. The doctors here don’t have time for drama-they see results. Why are Americans so scared of a cheaper option that works? We don’t have luxury of fear. If it helps, it’s good. End of story. No need to overthink biology like it’s a Netflix plot twist.
Haley Graves
January 23, 2026If your doctor suggests switching, don’t panic. Ask for the data. Read the NOR-SWITCH study. Look at the real-world outcomes. You’re not being traded in for a lesser product-you’re being given access to the same life-changing treatment without the financial prison. This isn’t a compromise. It’s liberation.
Gloria Montero Puertas
January 24, 2026Oh, please. 'No meaningful difference'? That’s the exact phrase used by pharmaceutical lobbyists to pacify the masses. And now you’re parroting it like a TED Talk zombie? The EMA’s approval process is a joke-200 analytical tests? That’s like measuring the color of a sunset with a ruler. Where’s the long-term immunogenicity data? Where’s the post-market surveillance across diverse populations? You’re ignoring the elephant in the room: this is a profit-driven illusion.
Frank Geurts
January 26, 2026It is with the utmost scientific rigor and institutional integrity that I must affirm, based upon the totality of peer-reviewed evidence, regulatory determinations, and longitudinal pharmacovigilance reports, that biosimilars, as currently approved and monitored by the FDA and EMA, demonstrate non-inferiority in clinical efficacy and safety profiles relative to their reference biologics. Furthermore, the economic implications of their adoption are not merely favorable-they are transformative for public health infrastructure.
Ayush Pareek
January 27, 2026It’s beautiful to see how science and compassion can meet here. I’ve worked with patients in rural clinics who couldn’t afford treatment-now, with biosimilars, they’re back on their feet. No need for grand speeches. Just quiet, steady healing. That’s what matters. Keep pushing for access. This isn’t just medicine-it’s dignity.
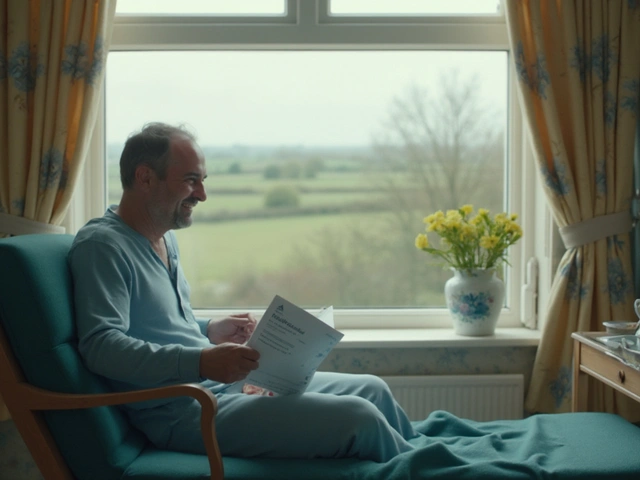
Sarah Mailloux
January 27, 2026My mom switched to an infliximab biosimilar last year. She was terrified. We sat down with her rheumatologist, read the studies together, and she’s been fine. No side effects. No flare. Just way less stress about the bill. Honestly? If you’re scared, talk to your doctor. But don’t let fear make you choose suffering over savings.
Nilesh Khedekar
January 29, 2026Of course they work-because the system demands it. The FDA doesn’t approve junk. But let’s not pretend this isn’t a corporate power play. Biosimilars are the Trojan horse for eroding patent protections. And now? They’re pushing biosimilars of biosimilars. Next thing you know, we’ll be on version 4.3 of the same molecule. Who’s really winning here? Not the patient. Not the doctor. The shareholders.
Jami Reynolds
January 31, 2026There is no long-term data beyond five years for most biosimilars. This is a massive, uncontrolled experiment on millions of immunocompromised patients. The FDA is cutting corners. The drug companies are lobbying aggressively. The media is parroting PR. And you’re just accepting it? Wake up. This is how people die quietly.
Amy Ehinger
February 2, 2026I’ve been on Humira for 8 years. My doc suggested switching to Inflectra last spring. I was nervous, but I did it. Felt the same. Same energy, same joint pain relief. My co-pay dropped from $450 to $85. I cried in the pharmacy parking lot-not from sadness, but from relief. I didn’t lose anything. I gained freedom. If you’re scared, talk to someone who’s done it. Real people, not studies. They’re out there.