Digoxin Generics: What You Need to Know About Cost, Safety, and Alternatives
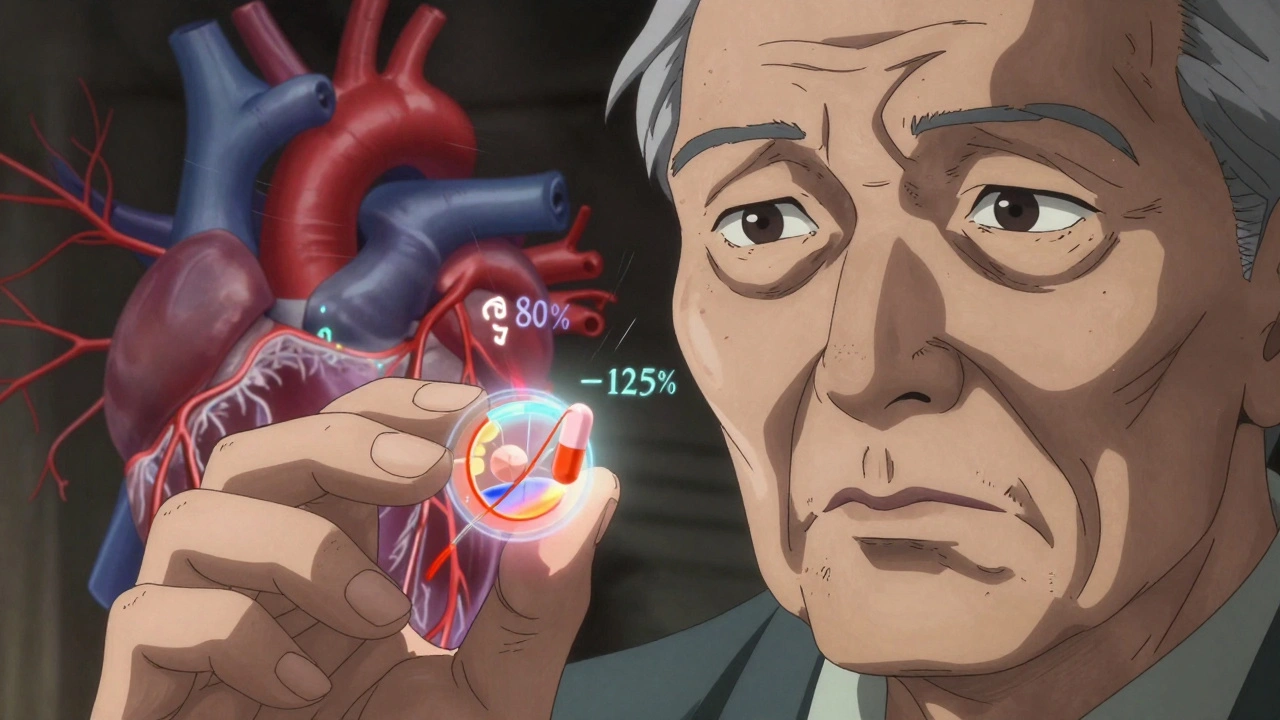
When you’re managing heart failure or an irregular heartbeat, digoxin, a cardiac glycoside used for over 200 years to strengthen heart contractions and slow heart rate. Also known as digitalis, it’s one of the oldest heart medications still in common use today. Most people get it as a generic version now—cheaper, widely available, and often just as effective as the brand-name Lanoxin. But here’s the catch: not all generic digoxin is created equal. Even small differences in how it’s absorbed can change how your heart responds, especially if you’re older, have kidney issues, or take other meds.
That’s why generic drug equivalence, the idea that a generic must perform the same as the brand in the body matters so much with digoxin. It has a narrow therapeutic window—meaning the difference between a helpful dose and a dangerous one is tiny. Too little and your heart keeps struggling. Too much and you risk nausea, confusion, or even life-threatening rhythms. That’s why switching between generic brands without your doctor’s input can be risky. Your body gets used to a specific formulation, and swapping it out might throw off your balance. This isn’t like switching between generic ibuprofen brands—digoxin needs careful monitoring.
And it’s not just about the pill. heart failure meds, a group of drugs including ACE inhibitors, beta-blockers, and diuretics that work together to manage symptoms and improve survival often overlap with digoxin. If you’re on multiple drugs, interactions matter. For example, antibiotics like clarithromycin or antifungals like ketoconazole can spike digoxin levels. Even over-the-counter antacids or fiber supplements can block absorption. That’s why keeping a full list of everything you take—prescription, OTC, supplements—isn’t optional. It’s a safety habit.
Cost is a big reason people choose generics. But if you’re paying less and feeling worse, the savings aren’t really savings. Some patients do better on one generic brand than another—not because one is "better," but because of how the body handles the filler ingredients or coating. If you notice new side effects after a refill, don’t assume it’s just your condition changing. Ask your pharmacist if the maker switched. And if your doctor hasn’t checked your digoxin blood level in over a year, it’s time to ask.
There’s no one-size-fits-all here. Some people stay on digoxin for decades with no issues. Others need to switch to newer drugs like ivabradine or sacubitril/valsartan because their condition changed or their body reacted poorly. What’s clear is this: digoxin isn’t going away, but how we use it is changing. You don’t need to be a medical expert to stay safe—just stay informed, stay consistent, and speak up when something feels off.
Below, you’ll find real-world posts that break down how digoxin fits into the bigger picture of heart care, what to watch for with generics, how it interacts with other drugs, and why some people need to avoid it altogether. These aren’t theory pieces—they’re from people who’ve lived it, and the doctors who’ve helped them through it.