Beta-Blocker & CCB Combination Risk Calculator
Assess Your Risk of Heart Complications
This tool helps you understand the risk of dangerous heart rhythm problems when taking beta-blockers with calcium channel blockers. Based on data from medical studies, it identifies whether your combination is likely safe or carries significant risk.
Risk Assessment Summary
Recommendations
When doctors prescribe beta-blockers and calcium channel blockers together, it’s not just adding two pills to the mix. It’s a careful balancing act-one that can save lives or, if mismanaged, trigger serious heart problems. This combination isn’t used lightly. It’s reserved for specific cases where one drug alone isn’t enough, and even then, the type of calcium channel blocker matters more than most patients realize.
Why Doctors Combine These Two Drugs
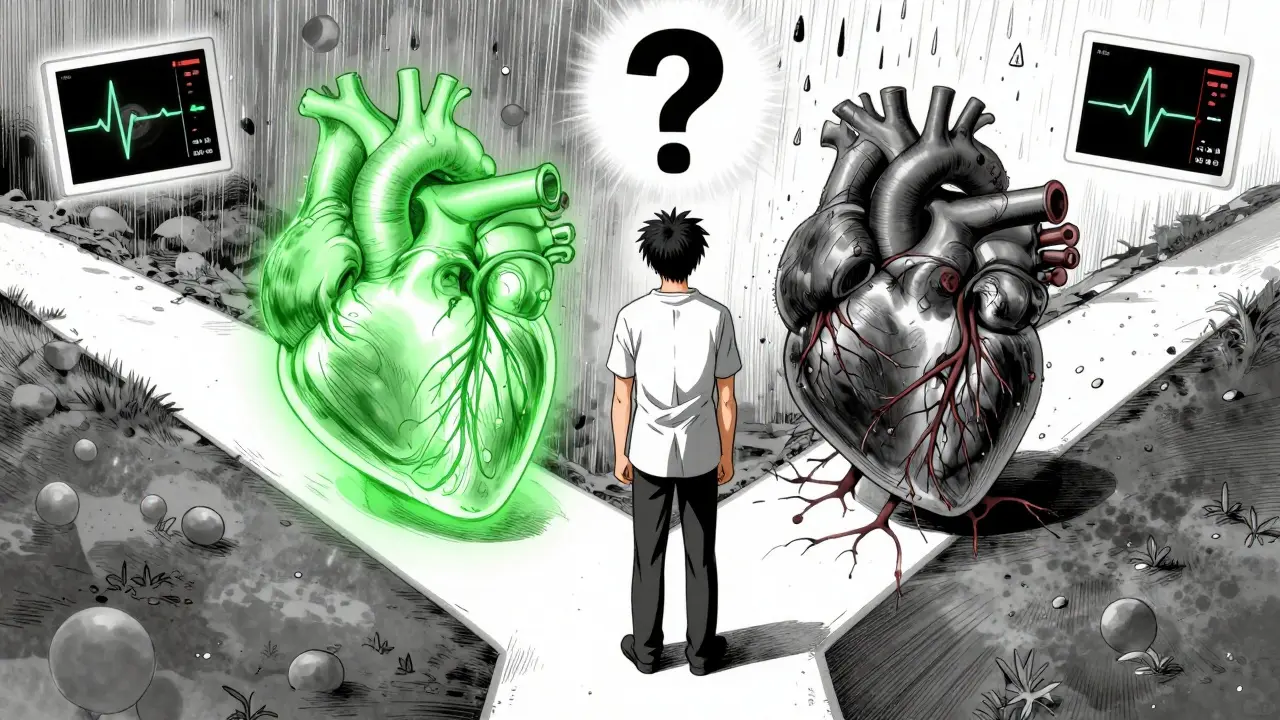
Beta-blockers like metoprolol, atenolol, and carvedilol work by slowing down your heart’s response to stress hormones. They lower heart rate, reduce blood pressure, and decrease the heart’s demand for oxygen. Calcium channel blockers, on the other hand, relax blood vessels by blocking calcium from entering heart and artery cells. This also lowers blood pressure and can ease chest pain (angina). When used together, these drugs can work better than either alone-especially for people with high blood pressure who also have angina. The American College of Cardiology and the European Society of Cardiology both list this combo as a first-line option for those two conditions. But here’s the catch: not all calcium channel blockers are created equal.The Critical Difference Between Dihydropyridines and Non-Dihydropyridines
There are two main types of calcium channel blockers. The first group-dihydropyridines like amlodipine and nifedipine-mainly target blood vessels. They don’t slow the heart much, which makes them safer to pair with beta-blockers. The second group-non-dihydropyridines like verapamil and diltiazem-hit both the heart and blood vessels. They slow the heart’s electrical signals and reduce its pumping strength. Combining a beta-blocker with verapamil or diltiazem is like stepping on the brake and the gas pedal at the same time. Both drugs suppress heart rate and contractility. The result? A higher risk of dangerously slow heartbeats (bradycardia), heart block, or even heart failure in people with weak hearts. A 2023 study of nearly 19,000 patients found that those taking beta-blockers with verapamil had a 10-15% chance of developing high-grade heart block-enough to require a pacemaker. In contrast, beta-blockers with amlodipine showed no such spike in heart rhythm problems.Who Should Avoid This Combo
This combination isn’t for everyone. If you have:- A slow heart rate (below 50 bpm at rest)
- A prolonged PR interval on ECG (over 200 milliseconds)
- Second- or third-degree heart block
- Sinus node dysfunction
- Heart failure with reduced ejection fraction (HFrEF)
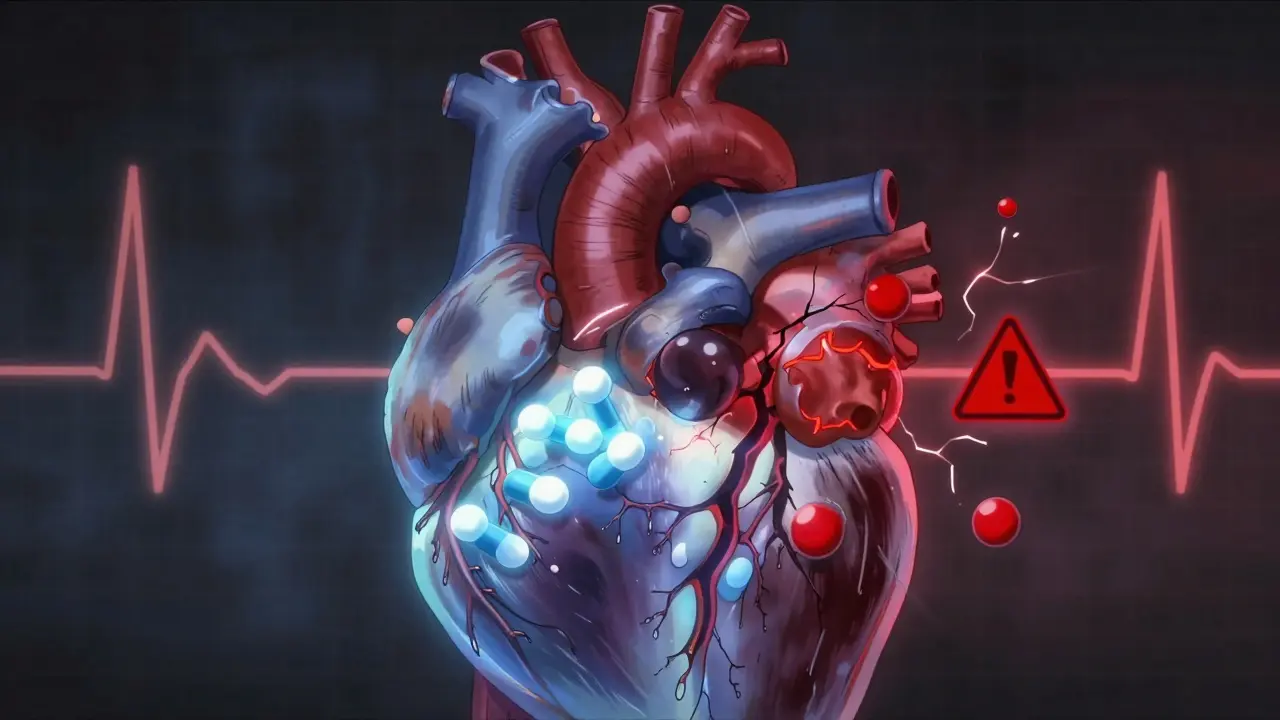
What Happens to Your Heart When You Take Both
The cardiac effects of this combination are measurable and sometimes alarming:- Resting heart rate can drop by 25-35 beats per minute-far more than with either drug alone.
- The PR interval (the time it takes for an electrical signal to travel through the upper chambers of the heart) can stretch by 40-80 milliseconds, increasing the risk of heart block.
- In people with existing heart weakness, left ventricular ejection fraction (a measure of how well the heart pumps) can drop by 15-25% with verapamil plus beta-blocker, compared to just 5-8% with one drug.
- Left ventricular end-diastolic pressure (a sign of heart strain) can rise by 8-12 mmHg, especially with nifedipine combinations.
When the Combo Actually Works Well
Despite the risks, this combination can be life-changing-for the right people. The same 2023 study found that patients on beta-blockers plus amlodipine had:- 17% lower risk of major heart events
- 22% lower risk of stroke
- 28% lower risk of developing chronic heart failure
- Hypertensive patients with resting heart rate above 80 bpm
- People with angina who can’t tolerate nitrates
- Patients who need both blood pressure control and heart rate reduction
Side Effects and Why People Stop Taking It
Even the safer combinations come with side effects. The most common:- Swelling in the ankles and legs (peripheral edema)-reported by 32% of prescribers
- Unexplained fatigue or dizziness
- Slow heart rate that feels uncomfortable
How Doctors Decide If It’s Right for You
Before starting this combo, a good doctor won’t just write a prescription. They’ll do a few key things:- Order an ECG to check your PR interval and heart rhythm
- Perform an echocardiogram to measure your ejection fraction
- Review all your other medications-especially if you’re on other heart drugs
- Start with low doses and increase slowly
- Check your heart rate and blood pressure weekly for the first month
What’s Changing in 2026
Guidelines are shifting. The FDA added a boxed warning in 2021 for verapamil + beta-blocker combinations in patients with conduction problems. The European Medicines Agency now requires an echocardiogram before prescribing this combo. In the U.S., only 12% of dual therapy prescriptions for hypertension involve beta-blockers and calcium channel blockers. In China, it’s 22%-showing regional differences in how aggressively doctors use this tool. The trend is clear: beta-blocker + amlodipine is growing. Beta-blocker + verapamil is declining. Experts agree: if you need both drugs, choose the dihydropyridine. Avoid verapamil unless there’s no other option-and even then, only with strict monitoring.What You Should Ask Your Doctor
If you’re prescribed this combo, don’t just take it. Ask:- Is this a dihydropyridine (like amlodipine) or a non-dihydropyridine (like verapamil)?
- Have you checked my ECG and heart function before starting?
- What signs should I watch for-like dizziness, fainting, or swelling?
- What’s the plan if my heart rate drops below 50?
- Are there alternatives I could try first?
Can beta-blockers and calcium channel blockers be taken together safely?
Yes, but only under specific conditions. The combination is safest when using a dihydropyridine calcium channel blocker like amlodipine with a beta-blocker. Avoid combining beta-blockers with verapamil or diltiazem unless absolutely necessary and only with close monitoring. Patients with slow heart rates, heart block, or heart failure should not take this combo.
What are the biggest risks of combining beta-blockers and calcium channel blockers?
The biggest risks are dangerously slow heart rate (bradycardia), heart block (which can require a pacemaker), and worsening heart failure-especially with non-dihydropyridine CCBs like verapamil. Studies show up to 15% of patients on beta-blocker + verapamil develop high-grade heart block. Peripheral swelling is also common with amlodipine, though usually mild.
Why is amlodipine safer than verapamil with beta-blockers?
Amlodipine is a dihydropyridine calcium channel blocker, meaning it mainly relaxes blood vessels and has little direct effect on the heart’s electrical system or pumping strength. Verapamil, a non-dihydropyridine, slows heart rate and reduces contractility-so when paired with a beta-blocker, the effects multiply dangerously. Think of it like two brakes on the same car: amlodipine is a gentle brake on the wheels; verapamil is a brake on the engine too.
Should I get an ECG before starting this combination?
Absolutely. A baseline ECG is essential to check your PR interval and rule out hidden conduction problems. If your PR interval is over 200 milliseconds, this combo should be avoided. The European Society of Cardiology recommends this step for every patient before starting beta-blocker + non-dihydropyridine CCB therapy.
What should I do if I feel dizzy or my heart feels too slow?
If you feel faint, dizzy, unusually tired, or notice your pulse is below 50 beats per minute, stop taking the medication and contact your doctor immediately. Do not wait. These could be early signs of heart block or severe bradycardia. Keep a home heart rate monitor if possible, and record your readings for your doctor.
Are there alternatives to this combination for high blood pressure and angina?
Yes. For high blood pressure, ACE inhibitors or ARBs combined with a diuretic or calcium channel blocker are often preferred. For angina, nitrates or ranolazine may be used instead. If you need both blood pressure and heart rate control, a beta-blocker with amlodipine is still the safest combo. Avoid verapamil or diltiazem unless your doctor has ruled out all other options.



Priscilla Kraft
January 11, 2026Just got prescribed amlodipine + metoprolol last week 😊 My heart rate dropped from 92 to 68 and my ankles are puffy but manageable. My doc said this combo is the gold standard if you're not a walking ECG disaster. So glad I didn't get verapamil 🙌
Vincent Clarizio
January 12, 2026Let me tell you something profound-this whole medical-industrial complex is built on the illusion of control. You think you're managing hypertension with pills, but really you're just outsourcing your body’s wisdom to a pharmacopeia that profits from your fear. Beta-blockers? They’re emotional suppressants disguised as cardiovascular tools. Calcium channel blockers? They’re chemical handcuffs on your arteries. And yet, we’re told to trust the algorithm, the guideline, the ‘evidence-based’ protocol-when the truth is, every human heart is a unique symphony, not a lab rat in a randomized trial. The real question isn’t whether amlodipine is safer than verapamil-it’s whether we should be poisoning our hearts at all. Maybe we should just… breathe. Or walk. Or eat a damn leafy green. But no, we need a pill for the pill that fixes the pill that was supposed to fix the problem we created by sitting on our couches eating processed carbs. I’m not mad. I’m just disappointed.
Michael Patterson
January 12, 2026yo u guys rly think verapamil is that bad? i had it with metoprolol for 3 yrs and my bp is perfect. sure i got a lil dizzy once but i just sat down. also my doc said if ur pr interval is under 200 its fine. also u dont need an echo if ur young and dont have symptoms. this article is fearmongering. i saw a guy on reddit who took 4 heart meds and still ran marathons. so chill.
Alfred Schmidt
January 12, 2026Ugh. Another ‘guideline’ piece written by someone who’s never met a patient with actual heart failure. I’ve seen 3 patients on verapamil + beta-blocker drop dead in the ER because some ‘study’ said it was ‘safe.’ One was 78, had a PR of 210, and was told ‘it’s fine.’ No echo. No follow-up. Just a script. Now he’s on a pacemaker and his wife blames me. I’m not blaming the drugs-I’m blaming the lazy docs who don’t check ECGs before prescribing. And don’t even get me started on how amlodipine causes ankle swelling like it’s a damn feature. This isn’t medicine. It’s guesswork with a DEA license.
Sean Feng
January 14, 2026So basically dont take verapamil with beta blockers. got it. thanks for the 2000 word essay on something that couldve been a bullet point.
Jason Shriner
January 14, 2026Wow. So the medical establishment finally figured out that combining two drugs that slow your heart isn’t a great idea? Took ‘em long enough. I bet the FDA had to be dragged kicking and screaming into this revelation after a few patients turned into human metronomes. Next up: ‘Surprise! Drinking bleach is bad for your stomach.’
Priya Patel
January 15, 2026Just shared this with my dad in India-he’s on verapamil + atenolol and didn’t know the risks. He’s gonna ask his doc to switch to amlodipine. So glad I found this! ❤️ I’m no doctor but even I could tell this combo sounded sketchy. Thanks for breaking it down so clearly!!
Jennifer Littler
January 15, 2026From a clinical pharmacology standpoint, the pharmacodynamic synergy between non-dihydropyridine CCBs and beta-blockers at the AV node is well-documented in the literature-particularly via L-type calcium channel inhibition and beta-adrenergic receptor blockade converging on reduced conduction velocity and myocardial contractility. The 2023 cohort study referenced demonstrates a statistically significant hazard ratio for high-grade AV block (HR 1.42, 95% CI 1.28–1.58) when verapamil is co-administered with beta-blockers, even after adjusting for age, renal function, and baseline QTc. This is not theoretical-it’s a Class IIa recommendation in ESC 2023 guidelines. The key is risk stratification: PR interval >200ms, ejection fraction <40%, and age >65 are red flags. Amlodipine, as a dihydropyridine, lacks significant nodal effects, making it the only CCB with a Class I safety profile in this context. Still, monitor HR weekly for the first 30 days.
Sam Davies
January 16, 2026Oh, so now we’re treating hypertension like it’s a Shakespearean tragedy? ‘To block or not to block-that is the question.’ Honestly, if you need a calculator to decide whether your patient can handle two pills, maybe you shouldn’t be prescribing them. Also, ‘89% accurate’? That’s not a calculator, that’s a fortune cookie with a medical license.
Christian Basel
January 17, 2026PR interval >200ms = avoid combo. EF <40% = avoid combo. Age >65 = avoid combo. So… who’s left? The 22-year-old athlete with borderline HTN? The combo’s basically a death sentence for anyone over 30. Why not just prescribe aspirin and hope?
Alex Smith
January 19, 2026Hey, I’m a nurse in a rural clinic and I’ve seen this play out a dozen times. A patient comes in with BP 180/100 and angina. Doc says ‘Let’s try metoprolol + amlodipine.’ They come back in 2 weeks with swollen ankles and say, ‘I feel like a zombie.’ We lower the amlodipine to 5mg, add a leg elevation tip, and boom-they’re fine. No pacemaker. No ER visits. But if they’d gotten verapamil? We’d be talking about a 78-year-old with a new pacemaker and a family who thinks the doctor ‘killed’ him. This isn’t rocket science. It’s common sense with a stethoscope. And yes-ask your doc which type of CCB they’re prescribing. If they don’t know, find a new one.