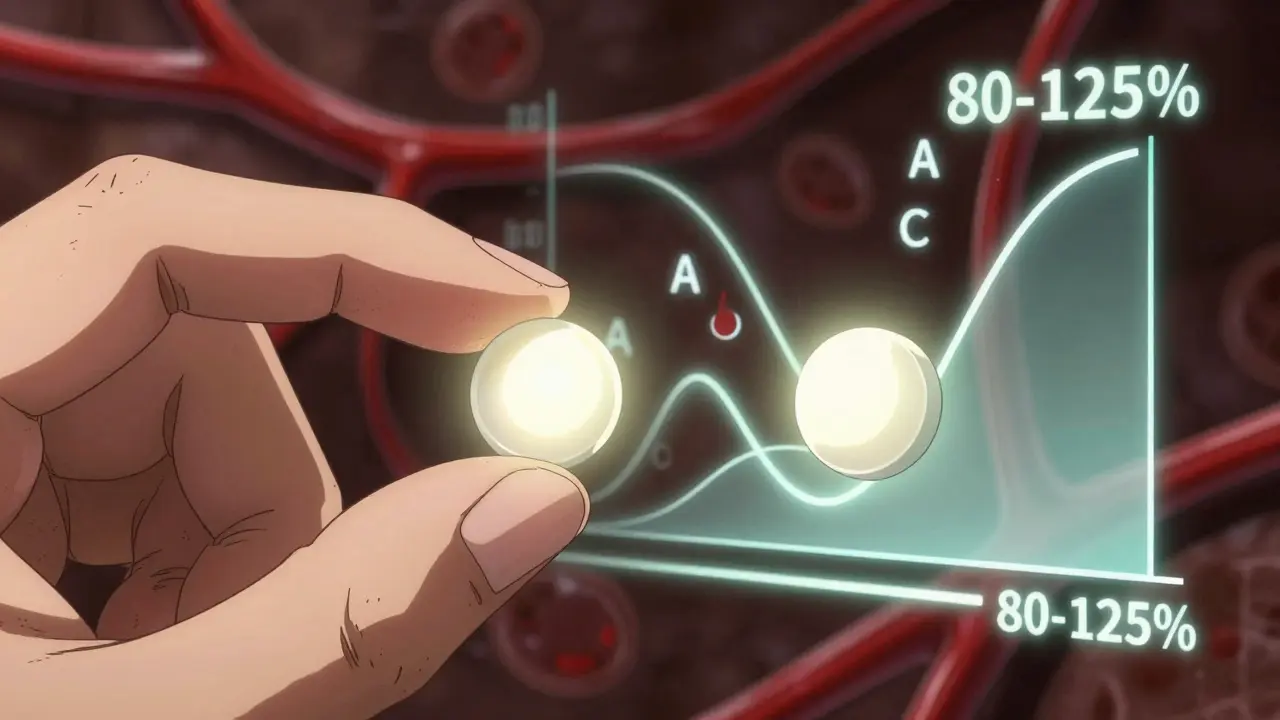
When you pick up a generic prescription, you might wonder: is this really the same as the brand-name drug you’ve been taking? A lot of people hear the 80-125% rule and think it means generics can be 25% weaker or 25% stronger. That’s not true. And that misunderstanding is costing people confidence in medicines that are just as safe and effective - and often save them hundreds of dollars a year.
What the 80-125% Rule Actually Measures
The 80-125% range doesn’t refer to how much active ingredient is in the pill. It’s not about the amount of drug you swallow. It’s about how much of that drug actually gets into your bloodstream - and how fast.
This rule is called bioequivalence. It’s a standard set by the U.S. Food and Drug Administration (FDA) to prove that a generic drug behaves the same way in your body as the brand-name version. To pass, the generic must deliver the same amount of medicine at roughly the same speed. The 80-125% range is the acceptable window for two key measurements: the total exposure over time (called AUC) and the peak concentration in your blood (called Cmax).
Here’s the catch: these numbers aren’t simple percentages. They’re calculated using logarithms because drug absorption in the body doesn’t follow a straight line - it’s a curve. That’s why 80% and 125% aren’t symmetrical around 100%. The math behind it means that if a generic’s average absorption is 90% of the brand, its 90% confidence interval (a statistical range that accounts for natural variation) must still fall entirely between 80% and 125%. In practice, most approved generics fall between 90% and 110% of the brand’s absorption.
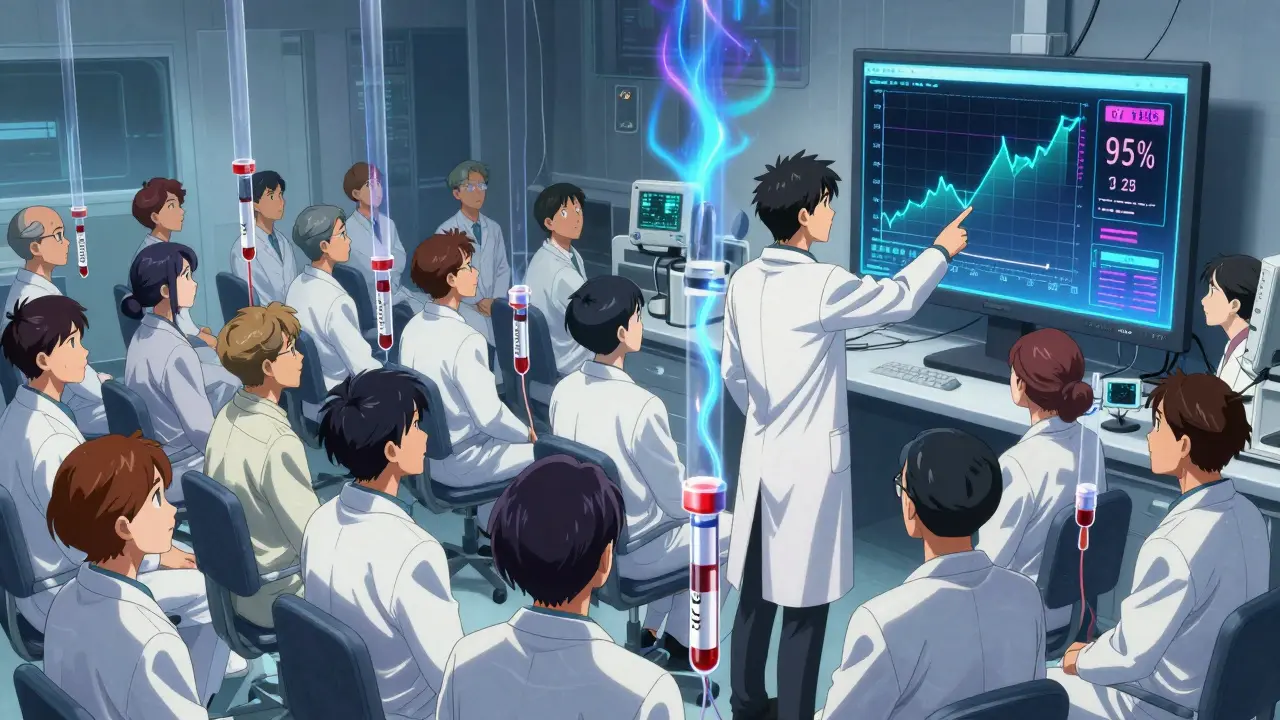
How the FDA Tests for Bioequivalence
Before a generic drug hits the shelf, it goes through a clinical study with 24 to 36 healthy volunteers. These people take both the brand-name drug and the generic, usually in a random order, with a washout period in between. Blood samples are taken every 30 to 60 minutes over 24 to 72 hours to map out how the drug moves through their system.
Scientists then calculate the AUC and Cmax for each drug. The ratio of the generic’s values to the brand’s is computed, and the 90% confidence interval is determined. If the entire interval sits between 80% and 125%, the drugs are considered bioequivalent. That’s it. No guesswork. No exceptions for most drugs.
But here’s what most people don’t realize: this isn’t a loose standard. A 2012 FDA analysis of over 2,000 bioequivalence studies found that 98% of generics had absorption levels within 95% to 105% of the brand. That’s tighter than many people assume. The 80-125% rule is designed to catch outliers - not to allow wide variation.
Why the Range Isn’t 80-120%
You might wonder why it’s 80-125% instead of 80-120%. The answer lies in statistics. If you use a linear scale, the difference between 80 and 120 is 40 percentage points. But drug absorption data is log-normally distributed - meaning it’s skewed. Using a log scale makes the math work properly. The natural log of 0.80 is -0.223, and the natural log of 1.25 is +0.223. That’s a perfectly symmetrical spread around 100% (which is log 1 = 0). So 80-125% isn’t arbitrary - it’s mathematically precise.
Using a fixed ±20% linear range would be misleading. A drug with 80% absorption might be fine, but if the variation between people is high, the confidence interval could dip below 80%, even if the average looks okay. The 90% CI requirement forces manufacturers to control variability - not just hit a target.
What About Drugs That Need Precision?
Not all drugs are created equal. Some - like warfarin, levothyroxine, and certain anti-seizure medications - have a narrow therapeutic index. That means even small changes in blood levels can cause serious side effects or make the drug stop working.
For these, the FDA uses a tighter standard: 90-111%. That’s not a typo. It’s a deliberate restriction. If a generic warfarin product’s 90% confidence interval for AUC or Cmax goes outside 90-111%, it gets rejected. The same goes for levothyroxine. In 2019, the FDA issued specific guidance for these drugs, requiring more rigorous testing and even stricter bioequivalence criteria.
And even then, real-world data backs this up. A 2016 study in JAMA Internal Medicine tracked over 2 million patients taking generic versions of cardiovascular drugs. The results? No difference in heart attacks, strokes, or hospitalizations compared to the brand-name versions.
Why Do People Still Doubt Generics?
Despite the science, myths persist. Online forums like Reddit and Student Doctor Network are full of posts where people claim generics are “only 80% as strong.” Pharmacists report being asked this question weekly. One 2020 survey found that 78% of pharmacists explain the bioequivalence rule to patients at least once a week.
The confusion often comes from a simple misunderstanding: people think the percentage refers to the amount of active ingredient in the pill. But the active ingredient is identical. The difference lies in the fillers, coatings, and manufacturing processes - which affect how quickly the drug dissolves and gets absorbed. The 80-125% rule is designed to make sure those differences don’t matter clinically.
And the data proves it. The FDA’s Sentinel Initiative, which monitors 200 million patient records, found no significant rise in adverse events for generic drugs across 94% of tested products between 2015 and 2020. That’s not luck. That’s regulation working as intended.
What Happens When a Generic Fails?
If a generic doesn’t meet the 80-125% standard, it doesn’t get approved. That’s not a suggestion - it’s a hard requirement. In 2022, 32% of incomplete generic applications were rejected because of bioequivalence issues. That’s more than any other reason.
Some companies try to cut corners. They might use cheaper excipients (inactive ingredients) or change the tablet’s coating. But if that changes absorption, the FDA catches it. One manufacturer in India had to recall a generic version of a blood pressure drug in 2021 after bioequivalence testing showed its Cmax was outside the acceptable range - even though the active ingredient was correct.
That’s why the FDA doesn’t just rely on lab tests. They inspect manufacturing sites. They require detailed documentation. And they monitor real-world use after approval.
Global Standards and Consistency
The U.S. isn’t alone. The European Medicines Agency (EMA), Health Canada, and Australia’s TGA all use the same 80-125% bioequivalence standard. The International Council for Harmonisation (ICH) has made this the global norm for over 50 countries.
Some emerging markets like Brazil and India have slightly different rules for certain complex drugs, but for standard oral tablets and capsules, the 80-125% rule is universal. That’s because the science is solid. It’s not a U.S. quirk - it’s the best method we have.
Real Impact: Savings and Access
Thanks to this rule, generics now make up 90% of all prescriptions filled in the U.S. - but only 23% of total drug spending. In 2021 alone, generics saved the healthcare system $373 billion. That’s money that goes back into hospitals, research, and patient care.
And it’s not just about cost. For people without insurance, or those on fixed incomes, generics are the only way they can afford their meds. A 2022 survey by the National Community Pharmacists Association found that once patients understood the bioequivalence rule, 63% said their concerns about generic effectiveness disappeared.
Pharmacists are trained to explain this. Many offer free consultations. You don’t need a PhD to understand it - just a clear explanation.
What’s Next for Bioequivalence?
The FDA is working on new tools. By 2025, they plan to use computer modeling - called “model-informed drug development” - to predict how a generic will behave without always needing human trials. This is especially helpful for complex drugs like inhalers, topical creams, or injectables where blood levels don’t tell the whole story.
They’ve also created a database tracking 1,200 challenging generic drugs that need special testing. But the core rule? Still 80-125%. The FDA says it’s stood the test of time - and it still works.
In 2022, a Supreme Court case upheld the FDA’s bioequivalence standards. The ruling noted that after 30 years of real-world use, there’s no evidence of therapeutic failure due to properly approved generics.
Bottom Line
The 80-125% rule isn’t a loophole. It’s a safeguard. It ensures that a generic drug works just like the brand - not because we trust the company, but because we tested it, statistically, with real human data.
If your doctor prescribes a generic, you’re not getting a lesser version. You’re getting a drug that has passed the same rigorous test as the brand. The active ingredient is identical. The absorption is nearly identical. The safety profile is identical.
Don’t let a misleading number make you afraid. The science is clear. Generics work. And the rule behind them? It’s one of the most carefully designed, evidence-based standards in modern medicine.
Does the 80-125% rule mean generic drugs have less active ingredient?
No. The active ingredient in a generic drug is identical to the brand-name version. The 80-125% rule measures how much of that ingredient enters your bloodstream and how quickly - not how much is in the pill. All generics must contain the same amount of active ingredient as the brand.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generics to meet the same strict quality, safety, and effectiveness standards as brand-name drugs. Real-world data from over 200 million patient records shows no meaningful difference in adverse events between generics and brand-name drugs for 94% of medications.
Why do some people feel different on a generic?
Sometimes, it’s psychological - the belief that a brand is better can influence how you feel. Other times, switching between different generic manufacturers (each with slightly different inactive ingredients) can cause minor differences in how the drug dissolves. For most people, this has no clinical effect. But if you notice a change, talk to your pharmacist. They can help you stick with the same generic manufacturer or switch back to the brand if needed.
Do all generic drugs follow the 80-125% rule?
For standard oral tablets and capsules - yes. The 80-125% bioequivalence rule applies to nearly all immediate-release generics. For complex products like inhalers, patches, or injectables, different testing methods are used because blood levels don’t fully reflect how the drug works. The FDA has special guidelines for these.
Can a generic be rejected even if it looks similar to the brand?
Absolutely. A generic can look identical and still be rejected if its absorption profile doesn’t meet the 90% confidence interval within 80-125%. Manufacturing changes - like a different coating or filler - can affect how fast the drug dissolves. The FDA tests the biological performance, not just the appearance.
Is the 80-125% rule used worldwide?
Yes. The U.S., European Union, Canada, Australia, and over 50 other countries use the same 80-125% bioequivalence standard for most generic drugs. It’s the global gold standard because it’s based on solid science, not politics or cost.
Why does the FDA use a 90% confidence interval instead of just the average?
Because people vary. Some absorb drugs faster, some slower. The 90% confidence interval accounts for this natural variation. If the average looks good but the range is too wide, it means the drug’s performance isn’t consistent. The FDA wants every patient to get the same benefit - not just most.




Monte Pareek
December 18, 2025Let me cut through the noise here - the 80-125% rule isn't a loophole it's a lock. People think if it's not 100% it's broken but that's like saying your car gets 28 mpg so it's defective because the manual says 30. The FDA doesn't wing it. They test with real humans, real blood draws, real stats. And 98% of generics land between 90-105%. That's tighter than your iPhone battery percentage.
And yeah the math is log-based because biology isn't linear. You don't get to pick the rules because they're convenient. The system works. Stop letting fear sell you overpriced brand names when your insurance won't cover them.
holly Sinclair
December 19, 2025What fascinates me isn't just the statistical rigor but the philosophical underpinning - the idea that equivalence isn't identity. We're not saying the generic is the same molecule in the same environment. We're saying it produces the same biological outcome within an acceptable margin of error. That's a profound shift from Platonic ideals to pragmatic empiricism.
It's like two pianos tuned slightly differently - one might have a brighter tone, the other warmer - but if both play Beethoven with equal emotional resonance, does it matter which one you hear? The body doesn't care about the pill's color or the company logo. It only cares about the concentration curve. And the FDA's standard ensures that curve doesn't deviate into dangerous territory.
There's a deeper cultural anxiety here too - we distrust what's cheap. We equate cost with quality. But medicine isn't luxury. It's a public good. The 80-125% rule is one of the few places where capitalism is held accountable by science. That's worth defending.
And yet - I still wonder why we don't talk more about excipient variability. Some people report differences not because of absorption but because of lactose, dyes, or coating agents. That's not bioequivalence - that's individual sensitivity. The FDA doesn't regulate that. Maybe it should. Maybe we need a second tier of labeling for sensitive populations. Not to scare people but to empower them.
Also - the fact that this standard is global is quietly revolutionary. For once, the science didn't bend to national interests. The ICH didn't let politics dilute the data. That’s rare. We should celebrate that.
And yet - I still get asked by patients why their generic makes them sleepy when the brand didn't. And I have to say - maybe it's the filler. Maybe it's the timing. Maybe it's placebo. Maybe it's all three. The system works. But humans are messy. And maybe the rule needs to evolve to meet us where we are, not just where the data says we should be.
Kelly Mulder
December 19, 2025Oh please. The 80-125% rule is a corporate shill’s dream. Let me break this down for you with actual precision - logarithmic scales are used because the FDA knows that if they used linear, the range would be too narrow and manufacturers would have to spend more on quality control. So they rigged the math to allow for more variance under the guise of "scientific rigor."
And don’t get me started on "98% of generics fall within 90-105%" - that’s cherry-picked data. What about the 2% that don’t? The ones that caused elevated INRs in elderly patients? The ones that led to seizure breakthroughs? You think the FDA publishes those? Please. They bury them under "no clinical significance" - a phrase invented by pharmacists who can’t admit they were wrong.
And yes - I’ve seen patients switch from brand to generic and go from stable to unstable. And no - it’s not "psychological." It’s pharmacokinetic variability masked as statistical noise. The rule is a compromise. A dangerous one. And you’re all just repeating the PR script.
Emily P
December 19, 2025So if the active ingredient is identical, why do some generics feel different? Is it just the fillers? Or is there something else I’m missing?
Vicki Belcher
December 19, 2025YESSSS this is so important 😭 I used to be scared of generics too until my pharmacist sat me down and explained it like this: "It’s like buying the same brand of coffee but from a different store - same beans, same roast, just different packaging."
And guess what? My blood pressure hasn’t budged since I switched. Saved me $400/month 🙌
Stop letting fear pay your bills. Generics are legit. The science is solid. Trust the process 💪❤️
Jedidiah Massey
December 20, 2025Log-normal distribution of pharmacokinetic parameters is non-negotiable in bioequivalence assessment. The 90% CI for ln(AUC) and ln(Cmax) must lie within ln(0.80) to ln(1.25) - that’s the ICH E9 and E14 gold standard. Anything less is methodologically unsound.
And let’s not conflate excipient variability with bioequivalence failure - that’s a confounder, not a flaw in the model. The FDA’s Sentinel Initiative data is robust - 94% of products show no adverse event differential. The outliers? They’re either non-compliant manufacturers or patients with CYP polymorphisms.
Bottom line: if your generic isn’t working, it’s not the rule - it’s the batch. Or your liver.
Alex Curran
December 22, 2025Used to work in a lab that tested generics for TGA. The 80-125% rule is brutal. One batch failed because the coating was 0.5 microns thicker. That’s thinner than a human hair. But it slowed dissolution enough to push the Cmax outside the CI. Got rejected. No second chances.
And yeah - the math is logarithmic. I’ve seen people argue it’s arbitrary. It’s not. It’s the only way to handle skewed data. Linear would be nonsense.
Also - the global adoption is no accident. This isn’t US exceptionalism. It’s good science. Everyone else copied us because it works.
Lynsey Tyson
December 23, 2025I get why people are nervous. I used to be too. But after working in a community pharmacy for 12 years, I’ve seen so many people struggle to afford their meds - and then light up when they find out the generic is just as good.
It’s not about being perfect. It’s about being safe and accessible. And honestly? Most of the time, the difference people feel isn’t the drug - it’s the worry.
My advice? Stick with the same generic brand if you notice anything. Talk to your pharmacist. They’re the real heroes here.
And if you’re still unsure? Talk to your doctor. But don’t let fear cost you your health.