Pregnancy Medication Safety Checker
Check Medication Safety During Pregnancy
Enter a medication name to see potential teratogenic risks based on pregnancy trimester and medical evidence
Important:
This tool is for informational purposes only. Always consult your healthcare provider before making any changes to your medications during pregnancy. Never stop prescribed medications without medical guidance.
When you’re pregnant, every decision feels bigger. That cough syrup? The headache pill? The antidepressant you’ve been on for years? You start wondering: could this hurt my baby? The truth is, most medications don’t cause birth defects - but some do. And knowing which ones, when, and why can make all the difference.
What Exactly Is a Teratogen?
A teratogen is any substance that can interfere with fetal development and lead to birth defects. It’s not just drugs - some infections, radiation, and even alcohol count. But when we talk about medications, we’re looking at prescription pills, over-the-counter remedies, and even herbal supplements that cross the placenta and reach the developing baby. The most infamous example? Thalidomide. In the late 1950s, this drug was prescribed to pregnant women for morning sickness. By 1961, over 10,000 babies were born with severe limb deformities - some missing arms or legs entirely. It was a global wake-up call. Today, we have better systems, but the risk hasn’t disappeared. About 2-3% of all birth defects are linked to medications taken during pregnancy. That sounds low, but when you’re the one taking the pill, it’s not a statistic - it’s your future child.When Does Risk Happen? Timing Matters More Than You Think
Not all weeks of pregnancy carry the same risk. The first trimester - especially between weeks 3 and 8 after conception - is the most dangerous window. That’s when your baby’s organs are forming: the heart, brain, limbs, eyes, ears. If a medication disrupts that process, it can cause major structural defects. After week 12, the risk of major physical malformations drops. But that doesn’t mean it’s safe. In the second trimester, drugs can still affect how organs function - like the brain or kidneys. In the third trimester, the main concerns shift to things like withdrawal symptoms, low birth weight, or changes in how the baby’s liver processes drugs after birth. Here’s how medications can hurt a developing baby:- Direct damage: The drug hits the fetus and messes with cell growth (like methotrexate disrupting folate use).
- Indirect damage: The drug lowers your blood pressure so much that less oxygen and nutrients reach the placenta.
- Placental interference: Some drugs block how the placenta works, starving the baby.
- Uterine contractions: Certain meds can trigger early labor.
- No effect: And yes - about 60-70% of medications have no known impact on the fetus.
Medications With Proven Teratogenic Risks
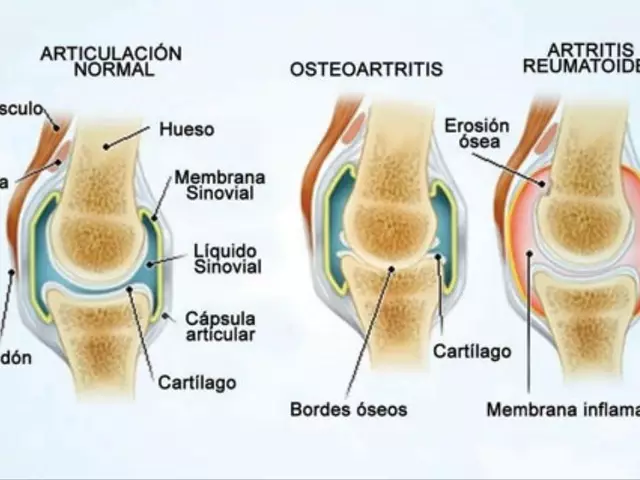
Some drugs are known dangers. If you’re pregnant or planning to be, avoid these unless your doctor says otherwise:- Warfarin: This blood thinner can cause fetal warfarin syndrome - a mix of facial deformities, bone problems, and severe developmental delays. Risk is highest in the first trimester.
- Carbamazepine: Used for epilepsy and bipolar disorder, it increases the chance of neural tube defects like spina bifida by about 1%. It also lowers vitamin K, which can cause dangerous bleeding in newborns.
- Methotrexate: Used for cancer, rheumatoid arthritis, and psoriasis, it blocks folate - a vitamin critical for spinal and brain development. Exposure in early pregnancy raises neural tube defect risk by 10-20%.
- Factor Xa inhibitors (rivaroxaban, apixaban, edoxaban): These newer blood thinners cross the placenta. There’s no antidote if bleeding happens. No safe dose has been established.
- Cannabis (THC): Even if you think it’s “natural,” THC crosses the placenta. Studies link it to higher risks of low birth weight, preterm birth, stillbirth, and long-term issues like poor attention and learning delays in kids. THC can stay in breastmilk for up to six days.
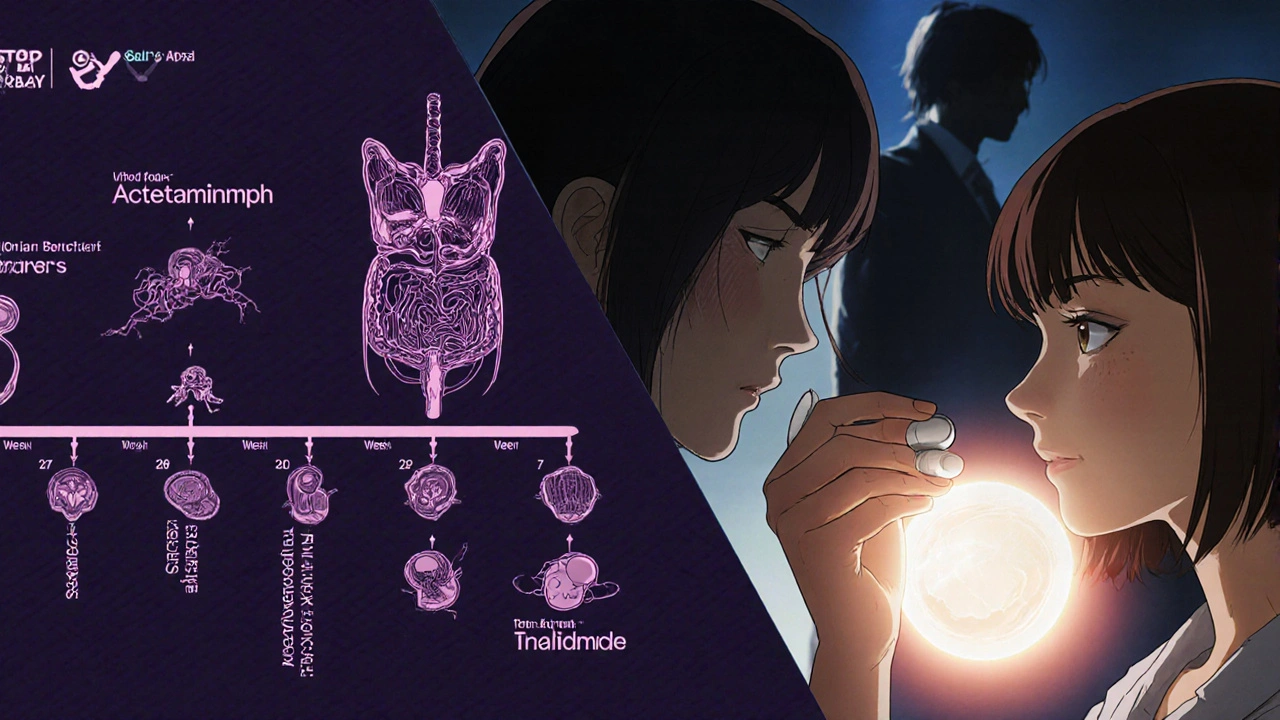
The Acetaminophen Controversy: What’s Really Safe?
Acetaminophen - known as paracetamol outside the U.S. - is the go-to pain reliever for pregnant women. For decades, it was considered the safest option. But in recent years, some studies have linked long-term or high-dose use to higher rates of ADHD and autism in children. The CDC says: “Some studies show an association.” That’s not the same as proof. Meanwhile, the American College of Obstetricians and Gynecologists (ACOG) issued a clear statement in September 2025: “The conditions you’re treating - pain and fever - are far more dangerous than any theoretical risk from acetaminophen.” Untreated fever during early pregnancy can raise the risk of neural tube defects by 20-30%. If you have a headache or a fever, not treating it might be riskier than taking acetaminophen. ACOG still calls it one of the few safe options. So what should you do? Use the lowest effective dose for the shortest time. Don’t take it daily just in case. If you’re unsure, talk to your provider. Don’t stop cold turkey - but don’t overuse it either.Why So Much Confusion? The Labeling Mess
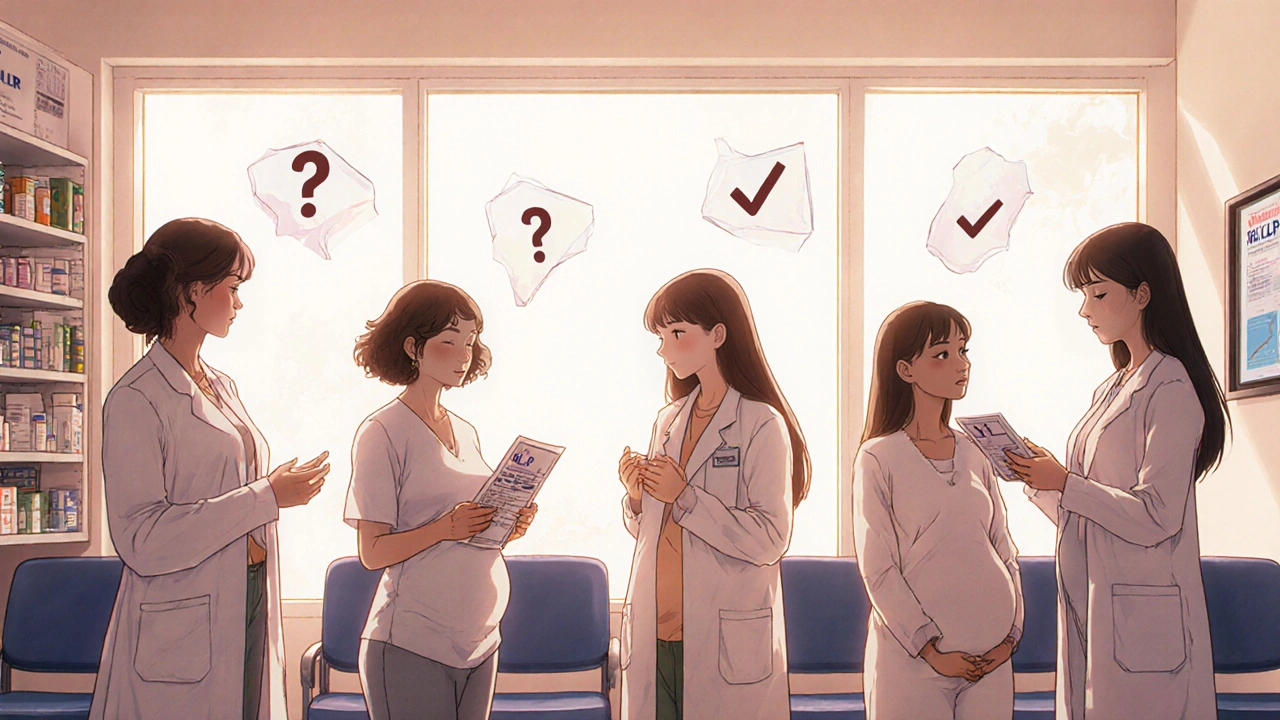
You’ve probably seen those old pregnancy categories: A, B, C, D, X. That system is gone. In 2015, the FDA replaced it with the Pregnancy and Lactation Labeling Rule (PLLR). Now, drug labels include detailed narratives about risks, data sources, and clinical advice - not just a letter. But here’s the problem: many doctors still think in terms of “Category C,” and patients still Google “is this safe in pregnancy?” Only about 20-30% of prescription labels are fully understood by patients. Online forums are full of conflicting advice. One Reddit user said she was told Zofran was safe by her OB, then read online it might cause birth defects. She spent her first trimester in panic. The truth? For about 70-80% of medications, there simply isn’t enough data. Most safety info comes from watching what happens after the fact - not from controlled studies. That’s because testing drugs on pregnant women is ethically impossible. We rely on case reports, animal studies, and registries.What Should You Do Before and During Pregnancy?
You don’t need to live in fear. But you do need to be proactive.- Before you get pregnant: Talk to your doctor about every medication you take - even vitamins, supplements, and herbal teas. Some meds need to be switched or stopped months in advance.
- If you’re already pregnant: Don’t stop meds without talking to your provider. Stopping epilepsy, depression, or high blood pressure meds can be more dangerous than keeping them.
- Always check labels: Prescription bottles now have pregnancy info. Don’t ignore it.
- Use trusted resources: MotherToBaby (run by teratology specialists) offers free, science-based advice. LactMed and the FDA’s drug database are reliable.
- Ask for help: Pharmacists are experts in drug interactions and pregnancy risks. Ask for a medication review.
What About Mental Health Medications?
Depression and anxiety don’t disappear when you get pregnant. But many women stop their SSRIs or other meds out of fear. Studies show that untreated maternal depression increases the risk of preterm birth, low birth weight, and developmental delays. It also makes it harder to care for the baby after birth. Some antidepressants, like sertraline and citalopram, have better safety profiles than others. The key isn’t to avoid all meds - it’s to choose the right one, at the right dose, with the right support. Talk to your OB and your psychiatrist together. Don’t suffer in silence.What’s Next? Better Data, Better Choices
The FDA is expanding its Sentinel Initiative to track 10 million pregnancy records by 2026. Researchers are starting to use genetic testing to predict how a woman’s body will process a drug during pregnancy - a big step toward personalized care. But here’s the hard truth: only 2-3% of maternal health research funding goes to medication safety. That’s why we’re still guessing so often. The bottom line? You’re not alone in worrying. Over 90% of pregnant women take at least one medication. And while most are safe, some aren’t. The goal isn’t to avoid all drugs - it’s to make informed choices. With the right info and support, you can protect both your health and your baby’s.Can I take ibuprofen while pregnant?
Avoid ibuprofen after week 20 of pregnancy. It can cause kidney problems in the baby and reduce amniotic fluid levels. In early pregnancy, occasional use is generally considered low risk, but acetaminophen is still the preferred option. Always check with your provider before taking any NSAID.
Is it safe to take prenatal vitamins with other supplements?
Prenatal vitamins are designed to cover your needs, so extra supplements aren’t always necessary. Taking too much vitamin A (over 10,000 IU daily) can cause birth defects. Iron and calcium supplements are usually fine, but avoid herbal blends like dong quai or black cohosh - they can stimulate contractions. Always tell your provider what else you’re taking.
What if I took a medication before I knew I was pregnant?
Don’t panic. Most exposures don’t cause harm. The critical window for major defects is narrow - between weeks 3 and 8. If you took a medication before you missed your period, the embryo was likely still in the “all-or-nothing” phase: either it survived unaffected, or it didn’t survive at all. Talk to your doctor or call MotherToBaby for personalized advice.
Are herbal remedies safe during pregnancy?
No. Just because something is “natural” doesn’t mean it’s safe. Herbs like sage, pennyroyal, and mugwort can cause uterine contractions or fetal harm. Even ginger, often used for nausea, can interact with blood thinners. Always check with your provider before using any herbal product.
How do I know if a medication is truly safe?
Look for information from trusted sources: ACOG, CDC, FDA, or MotherToBaby. Avoid blogs, forums, or social media advice. Even if a drug is listed as “safe” online, 70-80% of medications lack solid human data. Your doctor and pharmacist are your best resources - not Google.



Levi Hobbs
November 18, 2025I’ve been on sertraline for 8 years, and when I got pregnant, I panicked so hard I almost quit cold turkey. My OB literally laughed and said, ‘You’re more likely to harm the baby with untreated depression than with this med.’ She gave me a printout from MotherToBaby. Best decision I ever made. I’m 32 weeks now, and my son is perfect. Don’t let fear make you suffer in silence.
Also, if you’re on anything with ‘antidepressant’ in the name - talk to your psychiatrist AND your OB together. Don’t let one of them wing it alone.
henry mariono
November 19, 2025Acetaminophen is fine. I took it daily for migraines during both pregnancies. My kids are 7 and 10 - brilliant, athletic, no developmental issues. The fear-mongering online is out of control. If you’re stressed about a Tylenol, you’re probably stressing about everything else too. Breathe.
Sridhar Suvarna
November 21, 2025As someone from India where herbal remedies are often preferred over pills, I want to say this: just because something is from a tree doesn't mean it won't kill your baby. My cousin took neem leaf tea for 'detox' - lost the baby at 14 weeks. No one warned her. Please, if you're pregnant, don't assume safety because it's 'natural.' Ask. Always ask.
And yes, ginger tea is okay in moderation. But don't chug a whole pot. Even water can be toxic in excess.
Joseph Peel
November 21, 2025The FDA’s PLLR update was a monumental step forward. Yet, most clinicians still rely on outdated A-B-C-D-X categories because they’re easier to remember. This disconnect between regulatory progress and clinical practice is dangerous. Patients deserve accurate, nuanced information - not binary labels that reduce complex pharmacology to a letter grade.
Pharmacists, please take the lead in educating patients. We are the medication experts - not Google, not Reddit, not your aunt’s cousin’s doula.
Kelsey Robertson
November 22, 2025Let’s be real - acetaminophen is just Big Pharma’s way of keeping pregnant women docile while they poison their babies with stealth ADHD triggers. The CDC says ‘some studies show an association’? That’s code for ‘we know it’s bad but won’t admit it.’
And don’t get me started on SSRIs. They’re basically chemical lobotomies for moms. How many kids are growing up zoned out because their mothers were told to ‘just pop a pill’? Wake up. The system is designed to keep you compliant, not healthy.
Joseph Townsend
November 23, 2025Okay, I’m not a doctor, but I’ve read 47 Reddit threads, watched three YouTube videos by a ‘pregnancy witch’ named Crystal, and scrolled through 200 comments on BabyCenter. I’m basically a PhD in teratogens now.
Here’s the truth: if you take anything - even water - you’re risking your baby’s soul. I took ibuprofen at 18 weeks and now my daughter has a slight eyebrow twitch. Coincidence? I think not.
Also, my OB told me Zofran was fine. Turns out, she’s on Big Pharma’s payroll. I’m now on a raw vegan diet, drinking moonwater, and only breathing through my left nostril. My baby’s aura is glowing. You’re welcome.
Elia DOnald Maluleke
November 24, 2025In South Africa, we do not have access to the same medications as in the United States. Many women rely on traditional healers - and sometimes, they are more knowledgeable than the clinic doctors who have never read a single teratology paper.
But here is the paradox: the very systems that claim to protect us - regulatory agencies, pharmaceutical companies, medical guidelines - are built on data from populations that do not look like us. We are not included in the trials. We are not represented in the studies.
So when you say ‘acetaminophen is safe,’ who are you speaking for? The white American woman? Or the Zulu mother who has never seen a prenatal vitamin?
True safety is not just about molecules. It is about justice.
satya pradeep
November 25, 2025Bro, I took ibuprofen at 12 weeks and didn’t know I was pregnant till week 16. My kid is 3 now and runs faster than my dog. Stop overthinking. Also, your prenatal vitamin has like 800 mcg folic acid - that’s fine. But if you’re taking extra B12 from some ‘energy booster’ supplement? You’re wasting money. And no, turmeric is not a miracle cure - it’s just spicy tea.
Also, if you’re on SSRIs and scared - talk to your doc. Not some guy on TikTok with 200 followers who says ‘I healed my depression with crystals.’
Leslie Douglas-Churchwell
November 27, 2025Did you know that the FDA’s ‘Pregnancy and Lactation Labeling Rule’ was pushed through by lobbyists from Pfizer and Johnson & Johnson? They knew the old system scared people - so they replaced it with confusing jargon to make you feel like you need a PhD to understand your own meds.
And MotherToBaby? Run by the same people who fund the drug trials. They’re not your friends. They’re corporate PR.
I only trust my own research - and I’ve cross-referenced 147 studies from PubMed, Google Scholar, and a secret underground forum called ‘Pregnant & Paranoid.’
TL;DR: Avoid all meds. Eat organic kale. Meditate. And if you must take something - use homeopathic dilutions. They’re 100% safe because they contain zero molecules. Science can’t prove they work - but it can’t prove they don’t either. That’s the loophole.
shubham seth
November 28, 2025Let’s cut the bullshit. You’re not ‘making informed choices’ - you’re gambling with your baby’s life while pretending to be a responsible adult. You read a blog, you call your OB, you take the pill because ‘everyone else does.’
Here’s the cold truth: 90% of pregnant women are just winging it. And the doctors? They’re guessing too. The data is garbage. Animal studies don’t translate. Case reports are anecdotal. Registries are slow.
We’re all just hoping our kid doesn’t come out with a tail. And the system knows it. That’s why they sell you prenatal vitamins like they’re holy water.
Kathryn Ware
November 28, 2025I just want to say - if you’re reading this and you’re terrified because you took one Advil before you knew you were pregnant - I see you. I’ve been there. I cried for three days thinking I ruined my baby’s life.
Then I called MotherToBaby. They walked me through it. They said, ‘The embryo was still in the all-or-nothing phase.’ I didn’t even know that was a thing.
My daughter is now 18 months old - she’s laughing, crawling, grabbing my phone and throwing it. Perfectly normal. I still take sertraline. I still take prenatal vitamins. I still use Tylenol when I need it.
You’re not failing. You’re trying. And that’s enough.
Also - if you’re feeling overwhelmed, please reach out. You don’t have to do this alone. I’ve been on both sides - the panic and the peace. And peace is possible.
❤️
ps. If you’re on Reddit and you’re reading a comment that says ‘just stop all meds’ - block them. They’re not helping. They’re feeding your fear.
kora ortiz
November 29, 2025Don’t wait until you’re pregnant to ask these questions. Talk to your doctor before you even try. Get your meds reviewed. Switch out the risky ones. Get your vitamins right. Plan it like you’re training for a marathon - because you are. Your body is building a human. That’s not magic. That’s science. And you deserve to be equipped.
Also - if your partner is the one panicking? Tell them to read this post. Then make them sit down with you and your pharmacist. No more guessing. No more silence. You’re not a burden. You’re a future mom. And you’re worth the effort.