After a kidney transplant, the body doesn’t know the new organ isn’t an invader. It sees it as foreign-and tries to attack it. That’s where tacrolimus, mycophenolate, and steroids come in. Together, they form the most common immunosuppression regimen used worldwide. This isn’t just a random combo. It’s the result of decades of research, trial, and refinement. Since the mid-1990s, this triple-drug approach has become the gold standard for preventing rejection in kidney transplant patients. But it’s not perfect. Side effects are real. Dosing is tricky. And long-term outcomes still leave room for improvement.
Why This Combo Works
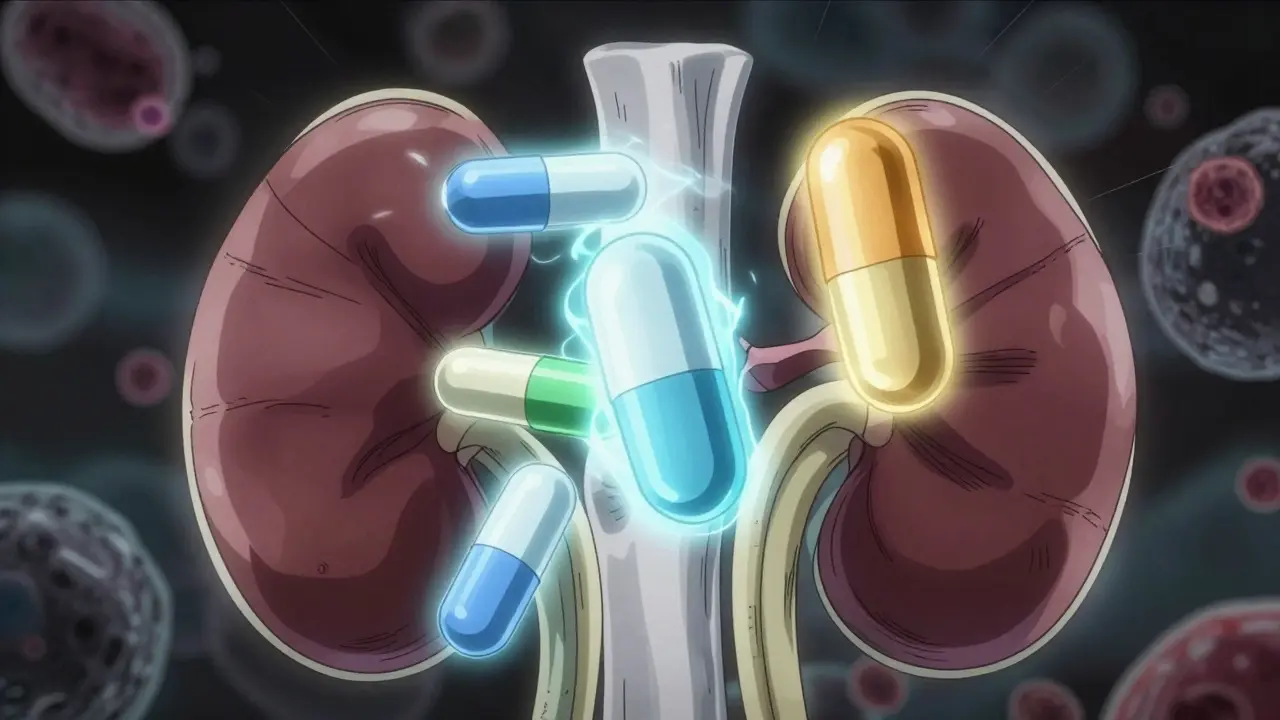
Before tacrolimus and mycophenolate, transplant patients relied on cyclosporine. It worked, but rejection rates were high-around 21% in the first year. Then came the game-changer: combining tacrolimus (a calcineurin inhibitor), mycophenolate mofetil (an anti-proliferative agent), and corticosteroids (broad anti-inflammatory drugs). The result? A drop in biopsy-proven acute rejection from 21% to just 8.2%. That’s a 61% reduction. Why? Because each drug hits the immune system differently.
Tacrolimus blocks the signal that tells T-cells to attack. Mycophenolate stops immune cells from multiplying. Steroids calm down the whole system. Together, they cover more ground than any single drug ever could. A 1998 study published in PubMed showed this combo was clearly better than using tacrolimus and steroids alone. The evidence was so strong it changed practice overnight.
How Each Drug Works
Tacrolimus is absorbed within 4 hours, peaks in the blood between 1.5 and 3 hours, and lasts about 8 to 12 hours. Doctors aim for a blood level between 5 and 10 ng/mL in the first year. Too low, and rejection kicks in. Too high, and you risk kidney damage, tremors, or even diabetes. It’s a tight balance. That’s why blood tests are routine-often weekly at first, then monthly. Newer methods now look at the total drug exposure over time (AUC), not just the trough level, to get a clearer picture of what’s happening in your body.
Mycophenolate mofetil (MMF) is taken as two pills a day-usually 1 gram each time. It turns into mycophenolic acid in the body, which shuts down the production of DNA in immune cells. Simple. Effective. But it’s hard on the gut. About 25 to 30% of patients get diarrhea. One in five have to lower the dose or stop it because of nausea, vomiting, or low white blood cell counts. Some centers now use enteric-coated versions to reduce stomach upset. Others switch to mycophenolate sodium, which is dosed once daily and may be easier to tolerate.
Steroids (usually prednisone or methylprednisolone) are the first line of defense. You get a 1,000-mg IV dose right in the operating room. Then, over the next few weeks, the dose drops fast: down to 15 mg/day by 3 to 4 weeks, then 10 mg/day by 2 to 3 months. The goal? Keep rejection at bay while minimizing long-term damage. Steroids cause weight gain, acne, mood swings, and higher blood sugar. For many, these side effects are worse than the transplant itself.
Side Effects You Can’t Ignore
This regimen saves kidneys-but it doesn’t come cheap. About 18 to 21% of patients develop new-onset diabetes after transplant, mostly because of tacrolimus and steroids. That’s not just a number. It means lifelong monitoring, diet changes, and sometimes insulin. Leukopenia (low white blood cells) happens in about 15% of patients, mostly due to mycophenolate. That raises infection risk. And yes, you’ll still get colds. But now, a simple flu can turn dangerous.
Diarrhea is the #1 reason people stop mycophenolate. It’s not just inconvenient-it can lead to dehydration, weight loss, and missed doses. Missing even one dose increases rejection risk. That’s why many clinics now pair MMF with a proton pump inhibitor (PPI) like omeprazole. But here’s the catch: PPIs can reduce MMF absorption. So timing matters. Take your MMF 2 to 4 hours apart from your PPI. Small things like this make a big difference.
Long-term steroid use? It’s a double-edged sword. Bone thinning, cataracts, high cholesterol, and mood changes add up. That’s why many centers now try to get patients off steroids entirely by 3 to 6 months. A 2005 multicenter trial showed that using daclizumab (an induction drug) with tacrolimus and mycophenolate worked just as well as the full steroid combo. And patients felt better. No moon face. No weight gain. No mood swings. About 89% stayed steroid-free at 6 months.
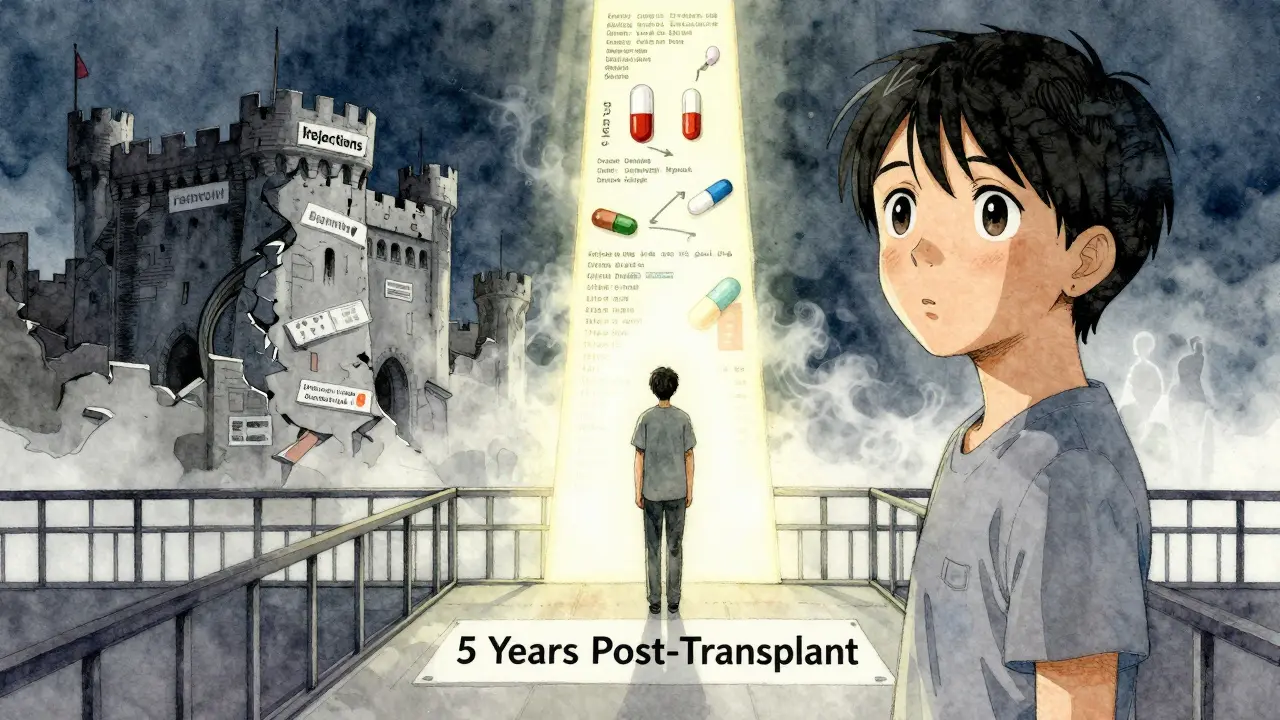
What Happens When It Doesn’t Work?
Even with this triple therapy, about 25% of adult kidney transplant recipients lose their graft within five years. Why? Because rejection isn’t the only problem. Chronic injury-the slow, silent damage from inflammation, high blood pressure, or recurring low-grade immune activity-still creeps in. These drugs prevent acute rejection. They don’t fix the long-term wear and tear.
Some patients develop drug resistance. Others have genetic differences that make them metabolize tacrolimus too fast or too slow. That’s why therapeutic drug monitoring is no longer just about trough levels. AUC (area under the curve) tracking is becoming standard. It tells you how much drug your body was exposed to over 12 hours-not just a single snapshot. This helps avoid under-dosing in fast metabolizers and over-dosing in slow ones.
And then there are interactions. Antibiotics, antifungals, even grapefruit juice can spike tacrolimus levels. Antacids can slash mycophenolate absorption. A patient on a new medication might not realize it’s sabotaging their transplant. That’s why pharmacists are now part of the transplant team-not just afterthoughts.
What’s Next?
The future isn’t about more drugs. It’s about smarter dosing. Researchers are testing biomarkers-tiny signals in the blood-that show if the immune system is about to attack. Imagine a test that says, “Your risk of rejection is rising,” instead of waiting for a biopsy. That’s the goal.
Pharmacogenomics is also changing the game. Some people have gene variants that make them process tacrolimus differently. A simple genetic test before transplant could tell doctors: “Start this patient at 30% lower dose.” That’s already happening in a few leading centers.
By 2030, experts predict 15 to 20% fewer patients will be on the standard triple therapy. Why? Because alternatives are emerging. Sirolimus, belatacept, and newer induction agents are offering steroid-free, calcineurin-sparing options. They’re not perfect yet-but they’re getting closer.
For now, though, tacrolimus, mycophenolate, and steroids remain the backbone. They’re not glamorous. They’re not easy. But they work. And for millions of people around the world, they mean a second chance at life without dialysis.
Why do I need all three drugs instead of just one?
Each drug targets a different part of the immune system. Tacrolimus blocks the signal that activates T-cells. Mycophenolate stops immune cells from multiplying. Steroids reduce overall inflammation. Using just one leaves gaps the immune system can exploit. Together, they cover more ground and lower rejection risk by over 60% compared to double therapy.
Can I stop taking steroids after a few months?
Yes, many patients do. Studies show that with proper induction therapy (like daclizumab), you can safely stop steroids by 3 to 6 months without increasing rejection risk. This reduces side effects like weight gain, diabetes, and bone loss. But it’s not for everyone. Your transplant team will monitor your immune activity and decide if you’re a candidate.
Why is my mycophenolate dose being lowered?
The standard dose is 1 gram twice daily, but about 20-30% of patients can’t tolerate it. Common reasons are diarrhea, nausea, or low white blood cell counts. Lowering the dose to 500 mg twice daily often helps while still keeping rejection risk low. If side effects persist, your team may switch you to mycophenolate sodium, which is easier on the stomach.
How often do I need blood tests for tacrolimus?
In the first month, you’ll likely have blood tests twice a week. As your levels stabilize, this drops to once a week, then every 2-4 weeks. After 6 months, most patients test monthly. Some centers now use AUC monitoring instead of just trough levels-it gives a better picture of how much drug your body actually used over time.
Can I drink grapefruit juice while on tacrolimus?
No. Grapefruit juice blocks an enzyme in your liver that breaks down tacrolimus. This causes levels to spike dangerously high-increasing the risk of kidney damage, tremors, or seizures. Even small amounts can do this. Avoid it completely. The same goes for Seville oranges, pomelos, and some herbal supplements like St. John’s Wort.
What You Should Do Next
If you’re on this regimen, keep your appointments. Don’t skip blood tests. Tell your doctor about every new medication-even over-the-counter ones. If you’re having side effects, speak up. There are options. Dose adjustments. Timing changes. Alternative drugs. You’re not stuck with discomfort.
And if you’re considering a transplant? Ask your team about steroid-free protocols. Ask about AUC monitoring. Ask about genetic testing. Knowledge is your best defense. This isn’t just about taking pills. It’s about staying alive-with a functioning kidney-for decades to come.