Splitting or crushing pills might seem like a simple fix-maybe you’re trying to save money, make it easier to swallow, or adjust a dose. But if you do it wrong, you could be exposing yourself or someone you care for to serious health risks. Cross-contamination, uneven doses, and toxic dust aren’t just theoretical problems. They happen. And they can be deadly.
Why Contamination Matters More Than You Think
When you split a pill with a knife, crush it in a plastic bag, or reuse the same splitter for different medications, you’re not just handling medicine-you’re handling potential hazards. Some pills contain powerful drugs like chemotherapy agents, blood thinners, or opioids. Even tiny amounts left behind on a splitter or in a crusher can cause harm.Take warfarin, for example. A 2023 incident at Oakwood Care Center showed how shared pill splitters led to cross-contamination. Fourteen residents ended up with dangerous blood-thinning levels-not because they were overdosed intentionally, but because residue from previous splits stayed on the equipment. That’s not rare. The Agency for Healthcare Research and Quality found that improper pill splitting contributes to 8.3% of medication errors in care homes.
And it’s not just about pills you can see. Hazardous drugs like cyclophosphamide can become airborne when crushed. Studies have measured toxic particles on healthcare workers’ gloves after open crushing-levels high enough to pose a cancer risk over time. This isn’t a problem for hospitals alone. Home caregivers, nursing staff, and even family members helping with daily meds are at risk if they don’t follow clean protocols.
What Pills Should Never Be Split or Crushed
Not all pills are created equal. Some are designed to release medicine slowly, protect the stomach, or stay stable until they reach the right part of the gut. Crushing or splitting these can destroy that design-and turn a safe dose into a dangerous one.- Extended-release or sustained-release tablets (like Metformin XR, OxyContin): Crushing them releases the full dose at once. This can cause overdose, rapid heart rate, or even death.
- Enteric-coated pills (like aspirin EC, omeprazole): These have a special coating to prevent stomach irritation. Break that coating, and the drug can irritate your stomach or break down before it’s absorbed.
- Capsules with beads (like Adderall XR): These contain tiny pellets that release medicine over time. Opening them ruins the timing and can cause spikes in drug levels.
- Hazardous drugs (like cyclophosphamide, methotrexate): These are used in cancer treatment. Crushing them without a closed system can expose you to carcinogens.
According to the FDA, 97.8% of these types of medications should never be split or crushed. If you’re unsure, check the label. Look for phrases like “do not crush,” “swallow whole,” or “extended release.” If it’s not clear, call your pharmacist. Don’t guess.
The Right Tools for the Job
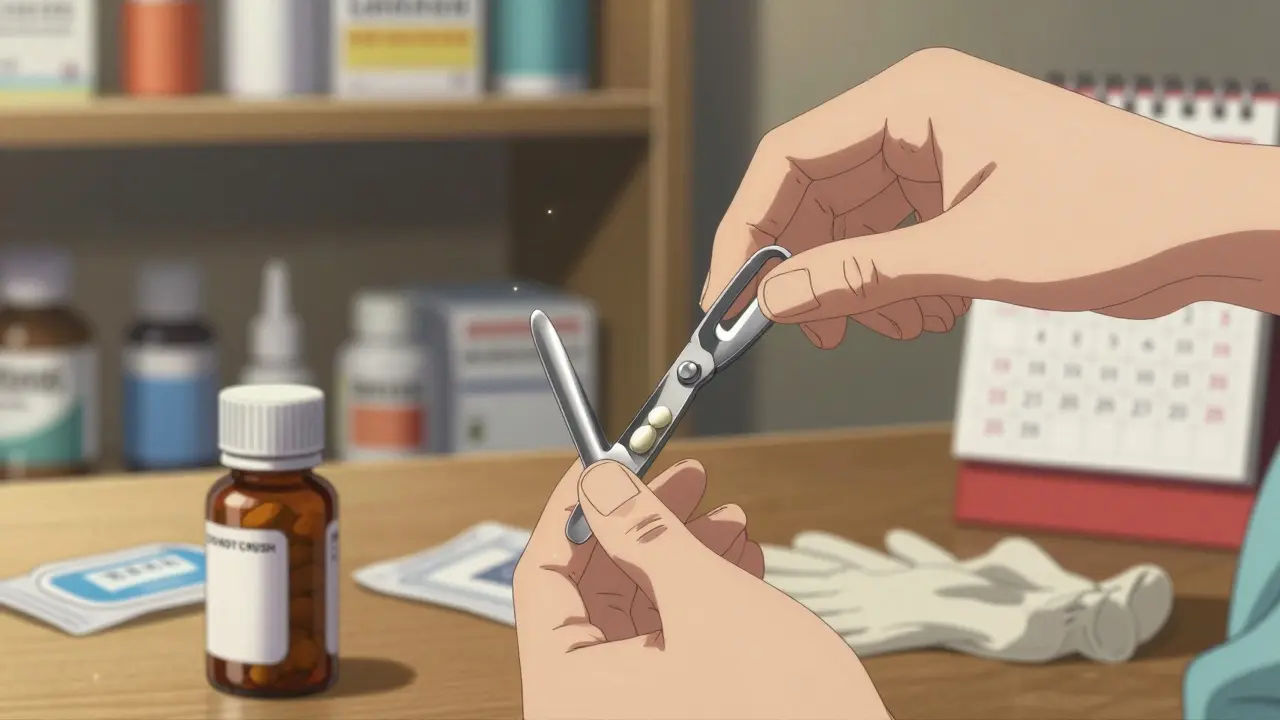
Using the wrong tool is one of the biggest causes of contamination and inaccurate dosing. Scissors, knives, or your fingers? Don’t do it.For splitting, use a dedicated pill splitter with a stainless steel blade and a v-shaped holder. These are designed to cut along the score line evenly. Models like the Med-Plus Pro (2024) include visual guides to help align the pill correctly-something 43.8% of staff struggle with using basic splitters.
For crushing, use a closed-system pill crusher like the Silent Knight. These devices trap all dust and powder inside a sealed chamber. Open crushing-like using a mortar and pestle or crushing in a ziplock bag-releases particles into the air. NIOSH testing shows closed-system crushers contain 99.8% of hazardous particles. Standard crushers? Only 72.1%.
And here’s the catch: never share equipment between patients or medications. Even if you wipe it down, residue stays. A 2022 study found that shared splitters increase contamination risk by 17.8%. Each person should have their own splitter-or it must be cleaned properly between uses.

How to Clean Equipment Between Uses
Cleaning isn’t optional. It’s mandatory.Here’s the step-by-step for cleaning a pill splitter or crusher after each use:
- Wear disposable gloves. Don’t skip this-even if you think your hands are clean.
- Remove any visible pill fragments with a dry, lint-free cloth.
- Wipe all surfaces with a 70% isopropyl alcohol wipe. Pay attention to the blade, holder, and any crevices where powder can hide.
- Let it air dry completely. Don’t use a towel-it can leave fibers or reintroduce germs.
- Store it in a clean, covered container. Don’t leave it on the counter next to toothpaste or cleaning supplies.
And yes-this applies even if you’re splitting pills for the same person. Different medications can interact chemically. Warfarin residue on a splitter used for levothyroxine? That’s a recipe for unstable thyroid levels or dangerous bleeding.
When to Split vs. When to Ask for Help
Splitting pills can save money-up to $1.2 billion annually in the U.S. when done right. But it’s not always the best choice.Ask your pharmacist these questions before you split anything:
- Is this pill specifically approved for splitting?
- Does it have a clear score line?
- Is it immediate-release, or does it have special coatings or time-release features?
- Can you get the exact dose in a different form? (Like a liquid or smaller tablet)
Many pharmacies now offer pre-split pills or lower-dose versions. For example, instead of splitting a 10mg tablet of lisinopril, you can often get a 5mg tablet for the same price. Some insurance plans even cover these lower doses to avoid splitting altogether.
If you’re a caregiver or work in a care home, push for centralized pharmacy splitting. Hospitals do it-87.3% of them have pharmacists split pills under controlled conditions. Only 42.6% of long-term care facilities do. That gap puts residents at risk.
What to Do If You’ve Already Split or Crushed Pills Improperly
If you’ve been using scissors, reusing splitters, or crushing pills without a closed system-stop. Don’t panic, but don’t ignore it either.Here’s what to do next:
- Stop using the equipment immediately.
- Dispose of any split or crushed pills you’ve already made. Don’t store them. Split pills lose potency faster and can absorb moisture or contaminants.
- Wash your hands thoroughly with soap and water. If you touched a hazardous drug, change your clothes.
- Call your pharmacist. Tell them what you’ve done. They can advise if you need to monitor for side effects or get a new prescription.
- Replace your splitter or crusher with a proper, dedicated one.
There’s no shame in making a mistake. But continuing the same unsafe practice? That’s where the danger grows.

How to Prevent Mistakes Before They Happen
Prevention is easier than cleanup. Here’s a simple checklist you can print or save on your phone:- Check the label for “do not crush” or “do not split.”
- Ask your pharmacist if the pill can be safely split or crushed.
- Use a dedicated splitter with a stainless steel blade and v-holder.
- Use a closed-system crusher for hazardous or fine powders.
- Clean equipment with 70% alcohol after every use.
- Never store pre-split pills-split them right before taking.
- Never share equipment between people or medications.
- Dispose of used wipes and gloves in a sealed bag.
And if you’re helping someone with dementia or limited mobility, consider a pill dispenser with pre-filled doses. Many pharmacies offer this service for free or low cost. It’s safer, simpler, and removes the need to split or crush at all.
What’s Changing in 2025 and Beyond
Regulations are catching up. Starting January 1, 2025, OSHA requires all hazardous drugs to be crushed only in closed-system devices. The FDA’s 2024 draft guidance now requires manufacturers to test and label whether a tablet can be safely split. By the end of 2026, every scored pill must come with a clear “split-safe” label.Pharmacies are also updating their systems. Electronic health records now show bold, highlighted warnings like “DO NOT CRUSH” directly on medication administration sheets. If you see a warning, don’t ignore it.
Emerging tech is helping too. Devices like Med-Engage’s FDA-cleared smart splitter can verify the split dose and alert users if the pill wasn’t cut properly. Early trials show a 47.2% drop in errors.
But none of this replaces your responsibility. Technology helps. But you’re still the one holding the pill, the splitter, the gloves. Make sure you’re doing it right.
Final Reminder: Your Safety Is Non-Negotiable
Splitting or crushing pills isn’t a minor household chore. It’s a medical procedure. And like any medical procedure, it needs care, precision, and respect.Don’t let convenience override safety. Don’t assume your pharmacist already checked the pill. Don’t reuse equipment because it’s “just one more time.”
One wrong split can lead to a hospital visit. One contaminated crusher can affect multiple people. One moment of carelessness can have lasting consequences.
Take the extra 30 seconds. Use the right tool. Clean it. Ask questions. Your health-or the health of someone you care for-depends on it.




Tony Du bled
December 21, 2025Been splitting my mom's blood pressure pills with a knife for years. Thought I was being smart. Now I'm gonna buy one of those Med-Plus Pro splitters and throw the knife in the trash. Don't need to be a hero with meds.
Just... don't.
Kathryn Weymouth
December 22, 2025The data cited here is compelling and rigorously sourced. The 8.3% medication error statistic from AHRQ, paired with the NIOSH findings on airborne particulates, underscores a systemic failure in home care protocols. It is not merely a matter of technique-it is a public health imperative to standardize equipment and enforce cleaning procedures. The FDA’s upcoming labeling requirements are a necessary step, but enforcement remains the critical gap.
Herman Rousseau
December 23, 2025Y’all need to stop treating meds like cereal. 😅
Just got my Silent Knight crusher last week-$45, but worth every penny. My grandma’s chemo pills used to make my whole kitchen smell like chemicals. Now? Zip. No dust. No panic. No mess.
And yeah, I clean it after every use. Even if it’s the same pill. Just... don’t be lazy. Your lungs and your aunt’s kidneys will thank you.
Candy Cotton
December 24, 2025It is regrettable that such basic medical hygiene has become a topic of public discourse. In civilized societies, pill manipulation is conducted under pharmaceutical supervision. The fact that laypersons are even permitted to crush medications reflects a catastrophic erosion of professional standards. One must wonder whether this is a consequence of deregulation, cultural decline, or both. The FDA’s 2026 labeling mandate is insufficient without mandatory certification for home caregivers.
Gabriella da Silva Mendes
December 24, 2025Okay but like… who even does this? I mean, I get splitting a 20mg pill in half for cost, but crushing chemo meds at home?? 😭
My cousin’s nurse just used a coffee grinder for her mom’s pills. I screamed. Like, literally screamed. And now I’m the family pill police. I’ve got a spreadsheet: ‘DO NOT CRUSH’ meds, who’s using what, and when the last cleaning was. I’m basically a pharmacist now. I didn’t sign up for this. But hey, at least my uncle didn’t bleed out. 🤷♀️
Also, I bought my own splitter and named it ‘Steve.’ He’s got a little sticker on him. I’m weird. Sue me.
Kiranjit Kaur
December 26, 2025This is so important! In India, many people crush pills because they can’t swallow them-no access to liquid forms, no money for smaller doses. But we don’t have these fancy tools. I learned from a nurse at the clinic to use a clean spoon and a plastic bag, then wipe with alcohol. Not perfect, but better than fingers or a knife.
Maybe someone should make cheap, reusable splitters for low-income homes. This isn’t just about safety-it’s about equity.
Sai Keerthan Reddy Proddatoori
December 26, 2025They say it’s about safety. But I bet the real reason is Big Pharma wants you to buy more pills. Why else would they make 20mg tablets but not sell 10mg ones? They profit off splitting. And now they’re pushing these expensive crushers? Fake safety. They want your money.
And why do I need to clean a splitter? I wash my hands. That’s enough. Government lies. Always lies.
Sam Black
December 28, 2025I used to think pill splitting was just a dumb home hack-until my neighbor’s dad ended up in the ER after a shared splitter got contaminated with a thyroid med. He went into atrial fibrillation. Didn’t even know why.
Now I carry a tiny alcohol wipe in my pocket when I help out with meds. And I always ask, ‘Is this one of the ones you don’t mess with?’
Turns out, most people don’t know. And that’s the real tragedy-not the lack of tools, but the lack of awareness. We need to talk about this more. Like, at dinner tables, at the pharmacy counter, in the waiting room. It’s not sexy. But it’s life-or-death.