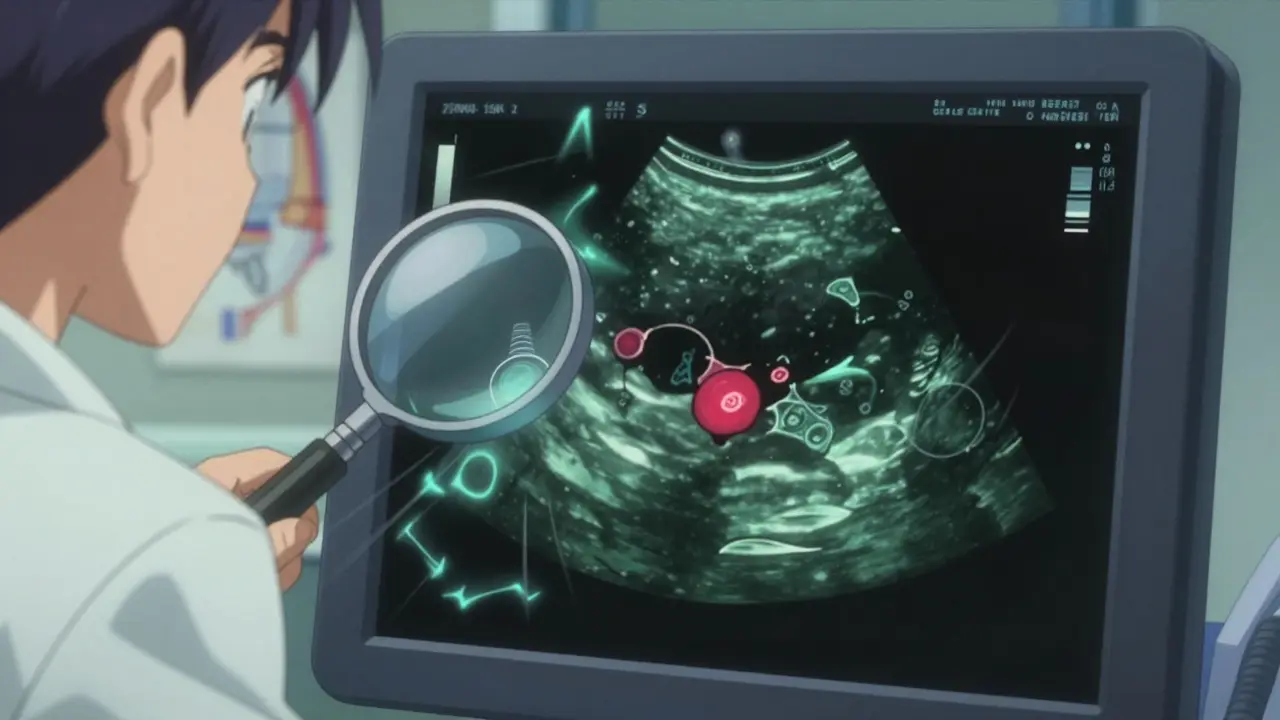
One in two adults over 60 has a thyroid nodule. Most won’t ever know it. And the vast majority? They’re harmless. But when a nodule shows up on an ultrasound, the fear kicks in: Is it cancer? And do I need a biopsy right away?
The truth is, thyroid nodules are incredibly common. Ultrasound scans find them in up to 67% of adults. Yet only 5-10% turn out to be cancerous. The real challenge isn’t finding them-it’s knowing which ones need action and which ones can be watched. Getting this wrong can mean unnecessary surgery or missed cancer. So how do you tell the difference?
What Makes a Thyroid Nodule Suspicious?
Not all nodules are created equal. Size matters, but it’s not the whole story. A 1.5 cm nodule with smooth edges and fluid inside is far less concerning than a 0.8 cm nodule with tiny calcium spots and jagged borders.
Ultrasound features are the first red flags. The most worrying signs include:
- Microcalcifications-tiny white specks inside the nodule. Found in over half of papillary thyroid cancers.
- Irregular or spiculated margins-edges that look jagged, not smooth.
- Hypoechogenicity-the nodule looks darker than the surrounding thyroid tissue.
- Taller-than-wide shape-if the nodule is taller vertically than it is wide, it’s more likely cancerous.
Benign nodules often look different: they’re mostly fluid-filled (cysts), have a spongy or honeycomb texture, or show large, coarse calcifications. These are rarely cancer.
Size alone isn’t enough. The American Thyroid Association says you should consider a biopsy if:
- The nodule is 1 cm or larger and has suspicious ultrasound features.
- The nodule is 1.5 cm or larger even if it looks normal on ultrasound.
- The nodule is 2 cm or larger-no matter how it looks.
But here’s the catch: some small nodules need attention anyway. If a nodule grows fast, size doesn’t matter as much.
How Fast Do Cancerous Nodules Grow?
Benign nodules grow slowly-about 1 mm per year on average. Cancerous ones? They grow faster. A 2017 study in the Journal of Clinical Endocrinology & Metabolism found that if a nodule grows more than 2 mm per year in at least two directions, the chance of it being cancer jumps sharply.
That’s why doctors now track growth over time. If your nodule was 1.2 cm last year and 1.5 cm this year, that’s a 3 mm increase. That’s a red flag-even if it’s still under 1.5 cm. Growth rate is now part of the official guidelines. If a nodule grows more than 2 mm/year, biopsy is recommended, regardless of initial appearance.
And it’s not just speed. Malignant nodules often grow unevenly. One part might balloon while another stays still. That’s why measurements need to be taken in three directions-length, width, and depth-at every ultrasound.
What Does a Thyroid Biopsy Actually Tell You?
The biopsy-fine-needle aspiration (FNA)-is the gold standard. A thin needle pulls out a few cells. A pathologist looks at them under a microscope. But it’s not perfect. About 15-30% of biopsies come back as “nondiagnostic.” That means not enough cells were collected. The fix? Repeat the biopsy with ultrasound guidance. Success rates jump to 85-90% the second time.
The results are grouped using the Bethesda System. Here’s what each category means:
- Category 1 (Nondiagnostic) - 1-4% cancer risk. Needs repeat FNA.
- Category 2 (Benign) - 0-3% cancer risk. Usually just monitoring.
- Category 3 (Atypia of Undetermined Significance) - 5-15% cancer risk. Often needs molecular testing.
- Category 4 (Follicular Neoplasm) - 15-30% cancer risk. Often leads to surgery or molecular testing.
- Category 5 (Suspicious for Malignancy) - 60-75% cancer risk. Surgery is usually recommended.
- Category 6 (Malignant) - 97-99% cancer risk. Surgery is confirmed.
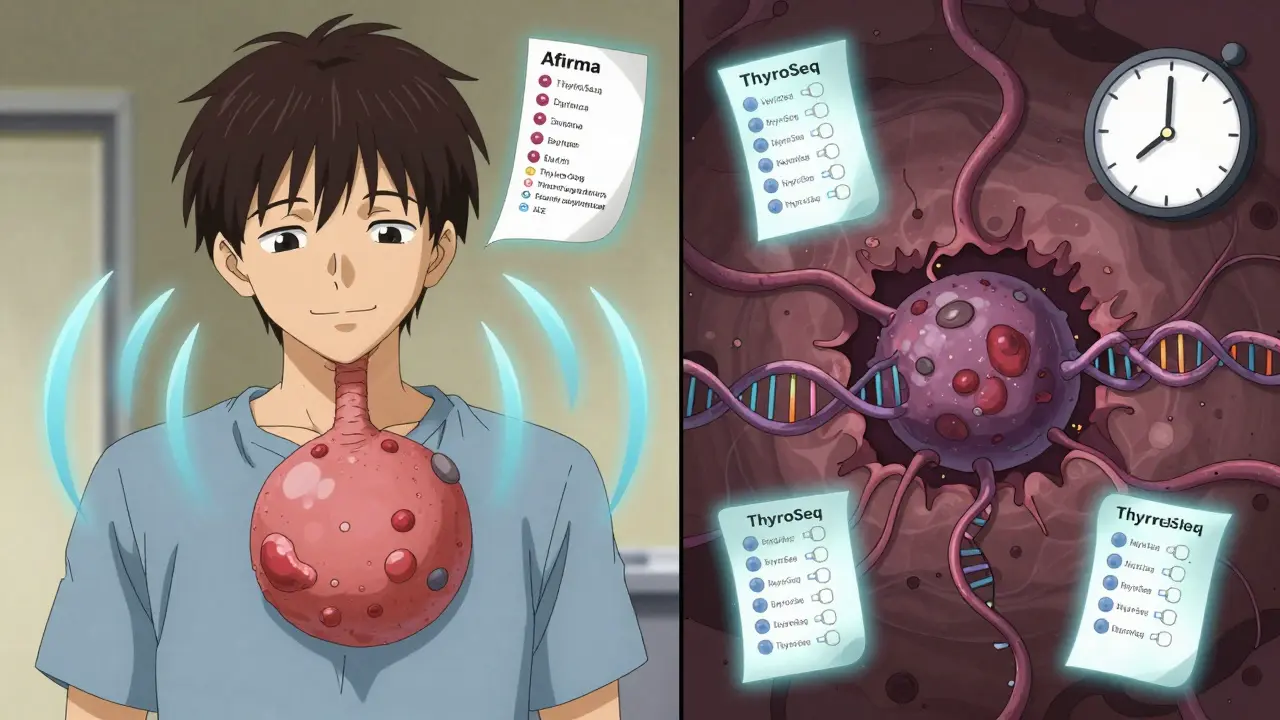
Categories 3 and 4 are the gray zone. That’s where molecular tests like Afirma GSC or ThyroSeq v3 come in. These tests look at the DNA inside the cells. If the test says “low risk,” you can avoid surgery. Studies show this reduces unnecessary operations by 35%. That’s thousands of people spared a scar and lifelong hormone pills.

What Kind of Cancer Are We Talking About?
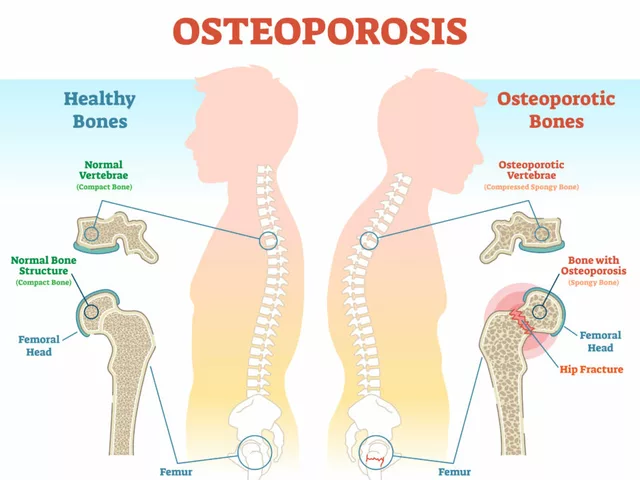
Most thyroid cancers are papillary-about 80%. They grow slowly, often spread to nearby lymph nodes, but rarely kill. Follicular cancer makes up 10-15%. It doesn’t usually go to lymph nodes but can spread to lungs or bones. Then there’s medullary, anaplastic, and lymphoma-rare, but more aggressive.
Here’s what most people don’t realize: Many thyroid cancers never cause symptoms. Unlike a large benign nodule that can push on your windpipe and make you cough or swallow hard, cancerous nodules are quiet until they’re big. That’s why ultrasound and biopsy are so important. You can’t feel cancer in your thyroid.
Benign nodules, on the other hand, can cause problems when they get big-over 4 cm. At that size, they might press on your throat, cause a lump you can see, make swallowing hard, or create a feeling of something stuck in your throat (called globus sensation). But even then, it’s not cancer-it’s just size.
When Can You Skip the Biopsy?
Not every nodule needs a needle. If you’re over 60 and have a small, solid nodule with no suspicious features, your doctor might just watch it. Same if you have a purely cystic nodule-fluid-filled with no solid parts. Those are almost always benign.
Also, if your nodule is under 1 cm and has no high-risk features, and you’re healthy with no family history of thyroid cancer, you may never need a biopsy. The risk is so low, the downsides of the procedure (bruising, minor pain, rare nerve injury) outweigh the benefit.
And here’s a big shift in thinking: Not every cancer needs surgery. A 2021 study in JAMA Surgery followed 500 people with tiny papillary cancers (under 1 cm) for five years. 87% showed no growth. Many patients now choose active surveillance-regular ultrasounds every 6-12 months-instead of immediate surgery. This is becoming standard for low-risk cases.
What Happens After a Biopsy?
If your biopsy says benign and the nodule isn’t growing, you’ll likely get an ultrasound every 12-24 months. If it grows or changes, you’ll get another biopsy.
If it’s indeterminate (Category 3 or 4), molecular testing is next. If the test says “low risk,” you can wait. If it’s “high risk,” surgery is usually recommended.
If it’s malignant or suspicious, you’ll be referred to a thyroid surgeon. Most thyroid cancers are treated with removal of half the gland (lobectomy). If cancer is confirmed, the other half may be removed later. You’ll likely need lifelong thyroid hormone replacement, but survival rates are over 98% for papillary and follicular types.
For large benign nodules causing symptoms, options now include radiofrequency ablation. It uses heat to shrink the nodule. A 2023 trial showed a 78% volume reduction in 12 months-with far fewer complications than surgery.
Why Do Some Doctors Over-Treat?
Thyroid cancer diagnoses have jumped 15-fold since the 1970s. But deaths haven’t changed. That’s because we’re finding tiny, harmless cancers that would’ve never caused a problem. This is called overdiagnosis.
Before molecular testing, about 30% of biopsies labeled “follicular neoplasm” turned out to be benign after surgery. That meant 30% of people had their thyroid removed for nothing. Now, with better tests, that number is dropping.
Still, practice varies. In academic centers, 89% of doctors follow biopsy guidelines strictly. In community clinics? Only 76% do. Some still biopsy every nodule over 1 cm, even if it looks perfectly normal. That’s why getting a second opinion or asking about molecular testing matters.
Don’t let fear drive decisions. Ask: What’s the risk? What’s the next step if it’s benign? What if I wait? You have options. You’re not just a nodule on a screen-you’re a person with choices.
What Should You Do Next?
If you’ve been told you have a thyroid nodule:
- Get a thyroid ultrasound from a certified radiologist. Make sure they measure all three dimensions.
- Ask: Does it have any suspicious features? Don’t just get the size-get the details.
- If it’s over 1 cm with suspicious features, or over 1.5 cm without, ask about FNA.
- If the biopsy is indeterminate (Category 3 or 4), ask for molecular testing. It can save you from surgery.
- If it’s benign and stable, ask how often you need follow-up ultrasounds.
- If you’re unsure, get a second opinion from an endocrinologist.
Thyroid nodules are common. Cancer is rare. But knowing the signs, asking the right questions, and using modern tools like molecular testing can make all the difference between unnecessary surgery and peace of mind.



Layla Anna
January 2, 2026i had a nodule and just ignored it for years lol my doctor was like uh you should prob get that checked and now im fine 🙃
Heather Josey
January 3, 2026This is an exceptionally well-researched and clearly presented overview. Many patients are terrified by the word 'biopsy' without understanding the nuanced risk stratification that modern guidelines provide. Thank you for emphasizing evidence-based approaches.
Donna Peplinskie
January 5, 2026I just want to say... thank you... for writing this... because so many people are scared... and they don't know what to ask... and honestly... this gives me hope... that we're getting better at not overtreating... 🌱
jaspreet sandhu
January 5, 2026You say cancer is rare but you also say 67 percent of people have nodules. So if 10 percent of those are cancer then that means 6.7 percent of adults have thyroid cancer. That is not rare. You are lying to people to make them feel better. The truth is the system is broken and they are cutting out thyroids like they are apples.
Alex Warden
January 7, 2026This is why America is falling apart. People are getting biopsied for everything. Back in my day we just ate more salt and didn't worry. Now we got doctors poking needles into people for no reason. Thyroid cancer? Nah. Just let it be.
Andy Heinlein
January 9, 2026so i got my nodule checked last year and it was benign and still the same size and honestly i feel so much better now that i know its not gonna kill me like i thought it would 🤗
gerard najera
January 10, 2026Fear drives medicine. Knowledge frees patients.
Olukayode Oguntulu
January 10, 2026The entire paradigm of thyroid nodule management is a neo-liberal bio-political apparatus designed to extract value from the corporeal substrate of the anxious subject. Molecular testing? Merely a techno-capitalist re-inscription of diagnostic hegemony. The real pathology is the epistemic violence of the ultrasound machine.
Lee M
January 12, 2026They say 5-10% are cancerous but they don't tell you that 90% of those 'benign' nodules are later found to be papillary microcarcinomas after surgery. The system is gaslighting us. Don't trust the Bethesda system. It's a lie.
Kristen Russell
January 13, 2026I'm so glad this info is out there. Too many people panic and rush into surgery. You deserve to know your options - and your body.
Bryan Anderson
January 14, 2026Thank you for including the growth rate criteria - this is something many primary care providers overlook. Tracking changes over time is far more valuable than a single snapshot. Well done.
Matthew Hekmatniaz
January 15, 2026I'm a nurse and I've seen patients cry because they think they're going to die. This post helps. Really helps. The fact that you included active surveillance as a real option? That's the kind of care we need more of.
Liam George
January 16, 2026They're hiding the truth. The FDA and big pharma are pushing molecular tests because they make billions from them. The real cancer risk is lower than they say. And the thyroid hormone pills? That's lifelong dependency. Wake up. They want you on meds forever. Look into iodine. It's been proven. But they don't want you to know.