For years, taking a daily low-dose aspirin was seen as a simple, cheap way to prevent a first heart attack or stroke. Many people over 50 did it without thinking twice. But the science has changed. Aspirin is no longer recommended for most healthy adults as a routine preventive measure. In fact, for many, continuing daily aspirin could be doing more harm than good.
Why the Big Shift?
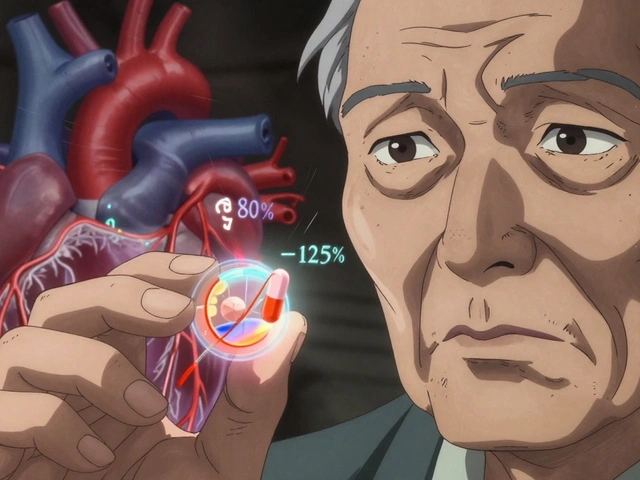
Back in the 1980s and 90s, studies showed aspirin reduced heart attacks in men and strokes in women. It seemed like a no-brainer: pop a pill, lower your risk. By 2016, nearly 25% of U.S. adults aged 40-79 were taking aspirin daily for primary prevention-meaning they had no history of heart disease or stroke. But newer, larger studies revealed something troubling. While aspirin did slightly lower the chance of a first heart attack, it also raised the risk of serious bleeding. And that risk didn’t stay small-it grew with age. For people over 60, the bleeding risk started to clearly outweigh the benefits. In 2022, the U.S. Preventive Services Task Force (USPSTF) reversed its earlier advice. Now, they say: don’t start aspirin for primary prevention if you’re 60 or older. The American College of Cardiology and American Heart Association followed suit. Their 2019 guidelines already warned against routine use. By 2024, prescriptions for aspirin in healthy adults had dropped by more than half compared to 2018. This isn’t just a guideline change-it’s a cultural shift in how doctors think about prevention.Who Should Definitely Skip Aspirin
You should avoid daily aspirin if you fall into any of these groups:- Age 60 or older-This is the clearest cutoff. The USPSTF gives a Grade D recommendation: do not start. For every 1,000 people over 60 taking aspirin for 10 years, about 1.6 will have a major bleeding event, while only 0.9 will avoid a heart attack. The math doesn’t work.
- History of stomach ulcers or GI bleeding-About 4% of U.S. adults have had a peptic ulcer. If you’ve had one, aspirin can bring it back-and fast. Even if it was years ago, your risk remains higher.
- Taking blood thinners like warfarin, apixaban, or rivaroxaban-Combining these with aspirin multiplies bleeding risk. It’s not a 1+1 situation-it’s more like 1+3.
- Using NSAIDs regularly-Ibuprofen, naproxen, even over-the-counter doses taken several times a week, raise bleeding risk. If you’re popping Advil for arthritis or back pain, aspirin is not a safe add-on.
- High risk of falls or bleeding disorders-If you’re prone to bruising easily, have low platelets, or are at risk for head injuries (like older adults with balance issues), aspirin increases the danger of intracranial bleeding.
What About People in Their 40s and 50s?
This is where things get messy. For people aged 40-59, the picture isn’t black and white. The USPSTF says you might consider aspirin if:- Your 10-year risk of heart attack or stroke is 10% or higher
- You have no increased bleeding risk
- You’re willing to take it for at least 10 years

What About Diabetes?
People with diabetes are often told they’re at higher risk for heart disease. That’s true. But does that mean they need aspirin? Not automatically. The 2025 AHA/ACC guideline for diabetes says aspirin might be considered only if:- You’re 40-70 years old
- Your 10-year ASCVD risk is 15% or higher
- You have no bleeding risk factors
Why Do So Many People Still Take It?
Despite the guidelines, nearly 1 in 6 adults over 60 still take aspirin daily. Why?- Fear-Many believe “if it was good before, it must still be good.” They don’t want to stop something that might protect them.
- Confusion-They don’t understand the difference between primary and secondary prevention. If they had a stent or bypass surgery, aspirin is still essential. But if they’ve never had a heart event, it’s a different story.
- Doctor disagreement-A 2023 JAMA study found 57% of patients got conflicting advice. Cardiologists are more likely to keep prescribing than primary care doctors. One patient on Reddit wrote: “My cardiologist says keep taking it. My PCP says stop. Who do I trust?”
What If You’re Already Taking It?
If you’re on daily aspirin and you’re over 60-or have any of the bleeding risk factors listed above-don’t stop cold turkey. Talk to your doctor. Stopping aspirin suddenly can cause a rebound effect, slightly increasing your short-term risk of clotting. But that risk is tiny compared to the long-term bleeding danger. Your doctor can help you taper off safely if needed. If you’re under 60 and unsure, ask for a risk calculation. Use the ACC’s free online tool or ask your provider to run your numbers. If your risk is below 10%, you’re better off without it.
What Should You Do Instead?
Aspirin was never the best tool for prevention-it was the easiest. The real game-changers are things that don’t cost a dime and have no bleeding risk:- Don’t smoke-This is the single biggest thing you can do to cut heart disease risk.
- Move more-150 minutes of brisk walking a week cuts risk by 30%.
- Eat real food-More vegetables, whole grains, nuts, fish. Less processed meat, sugar, and fried food.
- Control blood pressure-Even if you’re not on meds, keeping it under 120/80 helps more than aspirin ever could.
- Manage cholesterol-Statins are far more effective than aspirin at preventing first events in high-risk people.
The Future: Personalized Prevention
The next wave of prevention isn’t about age or one-size-fits-all pills. It’s about precision. Researchers are now studying:- Coronary calcium scores-A CT scan that shows plaque buildup. If your score is over 100, you might still benefit from aspirin-even if you’re over 60.
- Genetic testing-Some people metabolize aspirin poorly. Others have genes that make them more prone to bleeding. Future guidelines may require genetic screening before prescribing.
- Lp(a) testing-A blood test that identifies a hidden genetic risk for heart disease. If your Lp(a) is high, aspirin might still help.
Final Takeaway
Aspirin isn’t evil. It’s not useless. But for most healthy people, it’s not the right tool anymore. The days of popping a baby aspirin every morning as a default are over. If you’re under 40: skip it. You’re not at risk. If you’re 40-59: get your 10-year risk calculated. If it’s below 10%, don’t take it. If it’s above 10%, talk to your doctor about bleeding risk. If you’re 60+: unless you have a very specific, high-risk profile (like a calcium score over 300 and no bleeding history), you should stop. The harms outweigh the benefits. And if you’re unsure? Ask your doctor: “Based on my numbers, does aspirin still make sense for me?” Don’t accept vague answers. Push for the numbers. Your heart-and your stomach-will thank you.Should I stop taking aspirin if I’m over 60?
If you’re over 60 and have never had a heart attack, stroke, or stent, the answer is usually yes. The U.S. Preventive Services Task Force recommends against starting aspirin for primary prevention in this group because bleeding risk-like stomach or brain bleeding-outweighs the small chance of preventing a first heart event. If you’ve been taking it for years, don’t quit cold turkey. Talk to your doctor about a safe plan to stop.
Is aspirin still good for people with diabetes?
Only in specific cases. The 2025 guidelines say low-dose aspirin might be considered for adults with diabetes aged 40-70 who have a 10-year heart disease risk of 15% or higher and no bleeding risks. But if your Lp(a) level is normal, aspirin likely won’t help. Most people with diabetes don’t need it. Ask your doctor to check your risk score and Lp(a) before deciding.
What if my doctor still prescribes aspirin for me?
You have the right to ask why. Request your 10-year cardiovascular risk score and your bleeding risk assessment. If your risk is below 10% or you have a history of ulcers, NSAID use, or are over 60, the current guidelines say not to take it. Some doctors still follow older habits, especially cardiologists. If your doctor insists, ask for the evidence behind their choice. You can also get a second opinion.
Can I take aspirin occasionally for headaches instead of daily?
Yes. Occasional use for pain or fever-like once or twice a week-is not the same as daily preventive use. The bleeding risk from occasional aspirin is very low. The danger comes from taking it every single day over years. If you only take it when you need it, you’re not at increased risk for major bleeding.
What are safer alternatives to aspirin for heart health?
The best alternatives are lifestyle changes: not smoking, walking 30 minutes a day, eating more vegetables and whole grains, managing blood pressure, and controlling cholesterol. For people at high risk, statins are far more effective than aspirin at preventing first heart events. If you’re at very high risk, your doctor might recommend a statin instead-or in addition to aspirin, if you’re still a candidate.
How do I know my 10-year heart disease risk?
Ask your doctor to run your numbers using the Pooled Cohort Equations. They’ll need your age, sex, race, total and HDL cholesterol, blood pressure, diabetes status, and whether you smoke. Many clinics have free online calculators you can use too, like the one from the American Heart Association. If your score is under 10%, aspirin won’t help you. If it’s over 10%, you’ll need to weigh bleeding risk before deciding.



David Cunningham
November 23, 2025Man I used to pop one every morning like it was cereal. Then my doc showed me the bleeding stats and I was like... wait, I'm not trying to become a human blood bag.
Latonya Elarms-Radford
November 25, 2025Let’s be real - aspirin was never medicine, it was a placebo for the anxious middle class who needed to feel like they were doing *something* to outrun mortality. We’ve been sold a myth wrapped in a Bayer logo, and now the myth’s unraveling like a cheap sweater. The real tragedy isn’t the bleeding - it’s that we trusted a pill to do the work of discipline, diet, and self-awareness. We wanted a shortcut to immortality, and aspirin was the pharmaceutical equivalent of a fidget spinner.
New Yorkers
November 27, 2025Oh wow so now we’re telling old people to stop taking aspirin because they might bleed? What’s next? Telling them to stop breathing? The real killer here is the medical establishment’s need to flip-flop on everything so they can sell new guidelines like NFTs. I’ve seen 80-year-olds on aspirin who run marathons - and you want to take that away because of some abstract risk calculus? Give me a break.
Jessica Correa
November 27, 2025i read this and thought about my dad hesitated to stop even though he had ulcers and takes ibuprofen daily and now i get why so many people are confused its not just the science its the emotional weight of being told youve been doing something wrong for decades and now youre supposed to just... stop
Mark Williams
November 27, 2025From a clinical epidemiology standpoint, the shift is entirely evidence-based. The NNT for primary prevention in low-risk cohorts is astronomical - like 1000+ to prevent one MACE event - while the NNH for major GI bleed is under 200 in those over 60. The risk-benefit ratio inverted around 2018, and guidelines followed the data. What’s surprising is how slow the cultural adoption has been. We’re still clinging to 1990s heuristics in a 2024 risk stratification world.
Robin Johnson
November 28, 2025Hey if you're over 60 and still taking aspirin - don't panic. But do schedule a chat with your doc. Bring your cholesterol numbers, your BP logs, and ask: "Is this helping me or just giving me a false sense of security?" You're not weak for asking. You're smart for checking.
Miruna Alexandru
November 29, 2025The hypocrisy is staggering. We’re told to avoid pharmaceuticals for primary prevention - unless it’s statins, which are prescribed to 40% of Americans over 50, often without proper lipid profiling or Lp(a) screening. Aspirin gets demonized, but statins? No questions asked. The real issue isn’t aspirin - it’s the medical-industrial complex’s selective risk aversion. One pill is "dangerous," the other is "essential," despite both having similar bleeding profiles. The narrative is manufactured.
Daniel Jean-Baptiste
November 29, 2025my grandpa took aspirin every day for 30 years and he just turned 92 and still fixes his own fence. maybe the stats dont account for people who walk 5 miles a day and eat homegrown tomatoes. dont forget the human variable
Rahul Kanakarajan
November 29, 2025Why are we even debating this? Just test everyone’s Lp(a) and coronary calcium score and then decide. Stop pretending age is the only factor. This is 2024 not 1994. If your doctor doesn’t offer these tests, find a new one. Stop trusting guidelines that don’t know your name.
luke young
November 30, 2025My PCP told me to stop. My cardiologist said keep going. So I did what any sane person would do - I started walking 30 mins a day, eating more greens, and stopped stressing about it. Turns out, the best medicine wasn’t in a bottle at all.