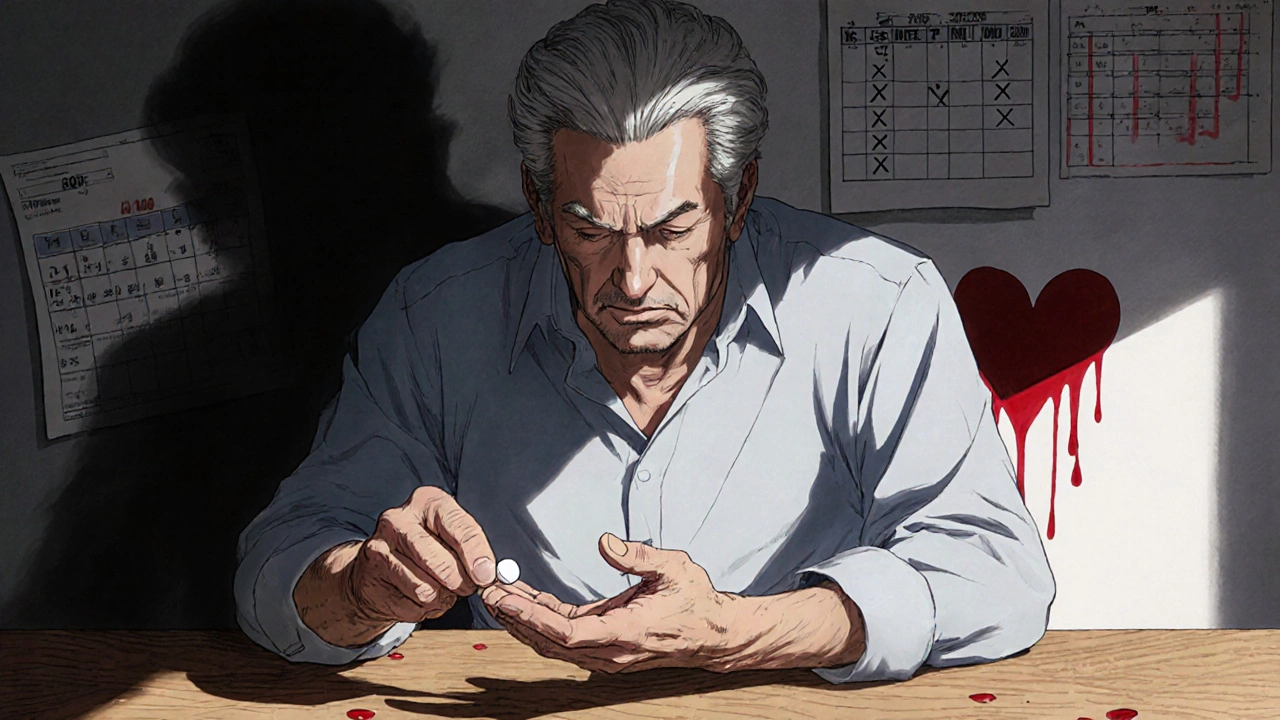
Who Should Not Take Aspirin: Risks, Alternatives, and Who’s at Danger
When you think of aspirin, a common over-the-counter pain reliever and blood thinner used for headaches, fever, and heart attack prevention. Also known as acetylsalicylic acid, it’s one of the most widely used drugs in the world—but it’s not safe for everyone. Many people pop it without thinking, but for some, even a single pill can trigger serious health problems.
If you have a history of stomach ulcers, open sores in the stomach or intestines that can bleed or perforate, aspirin can make them worse. It blocks protective stomach lining chemicals, leaving you vulnerable to internal bleeding. People with bleeding disorders, conditions like hemophilia or von Willebrand disease where blood doesn’t clot properly should avoid it too. Even if you’ve never had a problem before, taking aspirin with blood thinners like warfarin or clopidogrel raises your risk of dangerous bleeding—sometimes without warning.
Children and teens recovering from chickenpox or flu-like symptoms should never take aspirin. It’s linked to Reye’s syndrome, a rare but life-threatening condition that causes swelling in the liver and brain. Pregnant women, especially in the third trimester, should skip it too—it can delay labor, cause heart problems in the baby, or increase bleeding during delivery. People with severe kidney disease, where the kidneys can’t filter drugs properly or uncontrolled high blood pressure, where aspirin can interfere with blood pressure meds also need to be cautious.
And it’s not just about what’s in the pill—it’s about what else you’re taking. Aspirin interacts with many common drugs, from ibuprofen to certain antidepressants. If you’re on multiple medications, especially for chronic conditions like diabetes or heart disease, you might not realize how aspirin could be making things worse. That’s why a simple question to your doctor—"Is aspirin safe for me?"—can prevent a hospital visit.
There are safer alternatives for pain and inflammation, like acetaminophen for pain or naproxen for longer-lasting relief, depending on your health profile. But you can’t assume one size fits all. What works for your neighbor might be dangerous for you. The posts below dig into real cases where people got hurt by skipping this step—like someone who took aspirin for a headache and ended up in the ER with internal bleeding, or a senior who didn’t know their arthritis meds were making aspirin riskier. You’ll also find guides on how to talk to your doctor about drug safety, how to spot hidden risks in your medicine cabinet, and what to use instead when aspirin isn’t an option. This isn’t about fear—it’s about knowing your limits before you take that next pill.