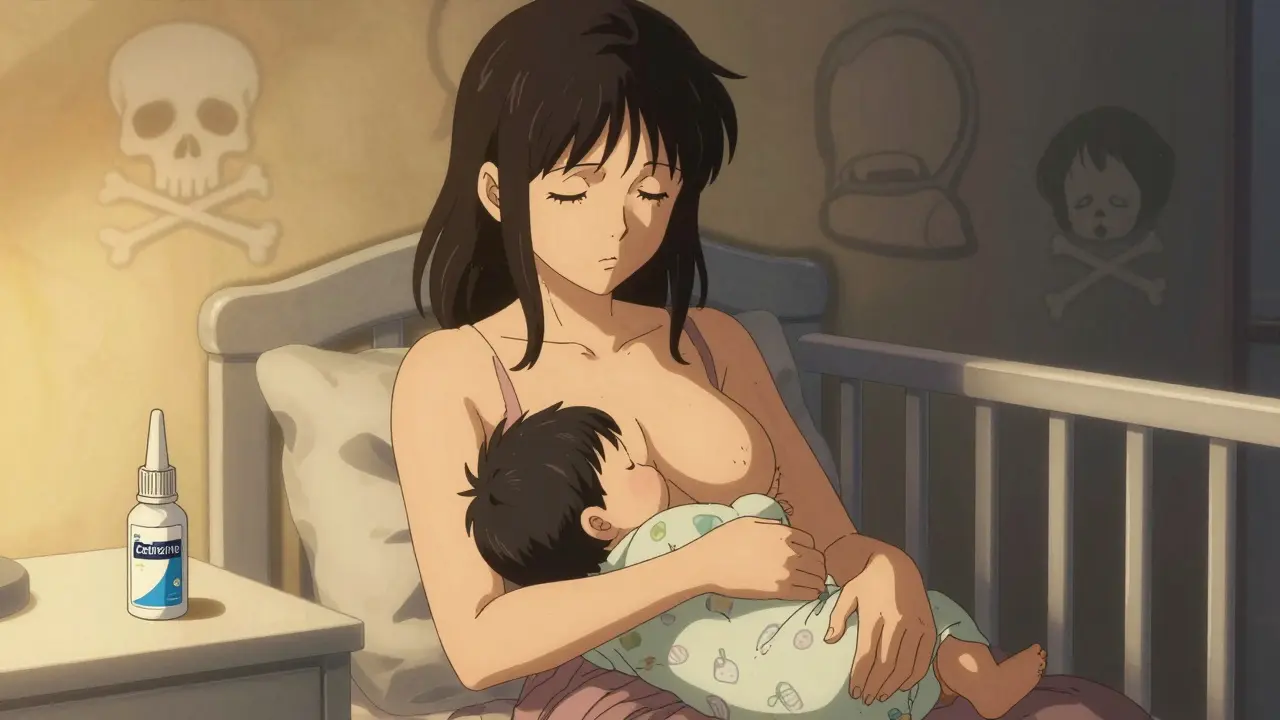
When you're breastfeeding and hit with a bad cold or seasonal allergies, the last thing you want is to choose between feeling better and keeping your baby safe. But many common cough and allergy meds carry hidden risks-especially when it comes to infant sedation. The truth is, not all medications are created equal when they pass into breast milk. Some are harmless. Others can make your baby dangerously sleepy, slow their breathing, or even stop them from feeding properly.
Why Some Medications Are Risky for Nursing Babies
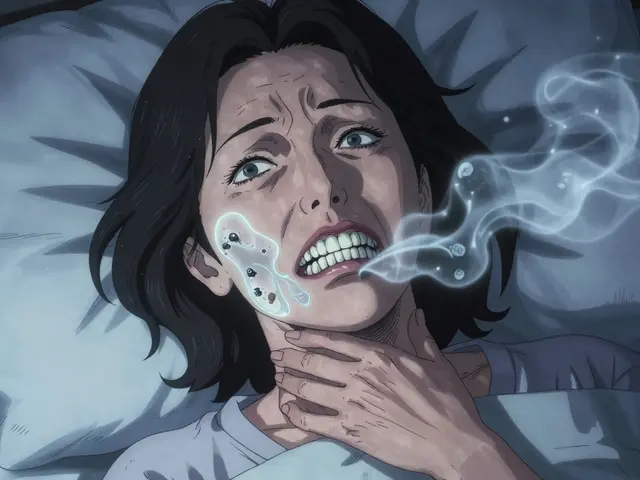
Your baby’s body is still learning how to process drugs. Their liver and kidneys aren’t fully developed, especially in the first two months. That means even small amounts of certain medications can build up in their system. Sedating drugs like first-generation antihistamines and codeine are the biggest culprits. These aren’t just "maybe" risks-they’ve been linked to real, documented cases of infant respiratory depression and even death.Take codeine, for example. Once thought to be safe, it’s now flagged by the FDA with a black box warning. Why? Because some people are "ultra-rapid metabolizers"-about 1 in 100 Caucasians-and their bodies turn codeine into morphine way too fast. That morphine ends up in breast milk. A 2012 study found infants exposed to codeine through breast milk had serum levels as high as 30 ng/mL. For a newborn, that’s enough to shut down breathing. There are reports of 13-day-old babies dying after their mothers took codeine for postpartum pain.
First-Generation Antihistamines: The Silent Sleepers
Diphenhydramine (Benadryl), chlorpheniramine, and hydroxyzine are common in over-the-counter allergy and cold meds. They work well for runny noses and sneezing-but they also cross into breast milk easily. Studies show milk-to-plasma ratios of 0.2 to 1.0, meaning your baby gets a significant dose relative to your weight.A Motherisk study found 1.6% of nursing infants showed noticeable drowsiness after their moms took diphenhydramine. That might sound low, but when you consider how many moms use it, the numbers add up. Reddit threads and breastfeeding forums are full of stories: "My 6-week-old wouldn’t wake up to feed after one Benadryl," or "She slept for 5 hours straight and missed three feedings." One survey found 68% of mothers who used codeine or diphenhydramine noticed changes in their baby’s alertness. Only 12% saw changes with ibuprofen.
The Royal Women’s Hospital in Australia and the American Academy of Pediatrics both warn: these meds aren’t recommended. Even a single dose can cause issues in newborns. And if you’re using it daily? The risk grows.
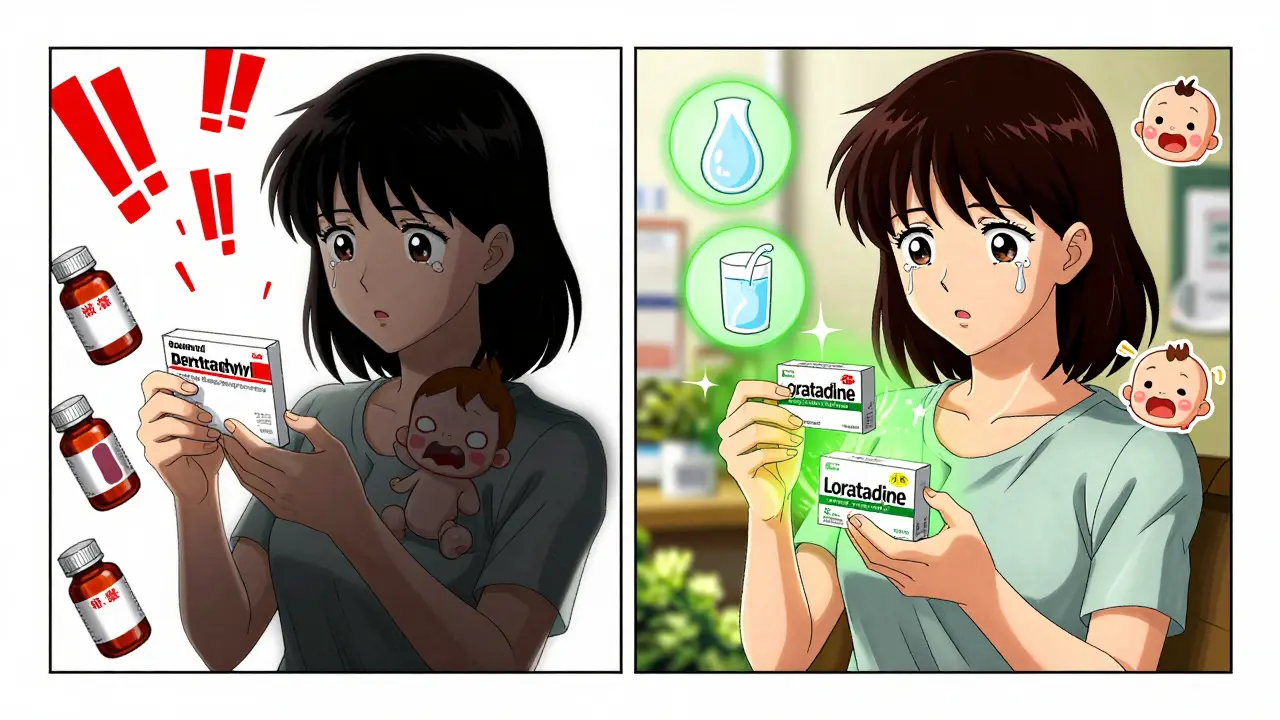
The Safer Alternatives: Second-Generation Antihistamines
Good news: you don’t have to suffer through allergies without relief. Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) are the new gold standard for breastfeeding moms.Here’s why they’re safer:
- Cetirizine: Milk-to-plasma ratio of 0.25-0.75. Infant exposure is only about 0.14% of your weight-adjusted dose. No sedation reported in clinical studies.
- Loratadine: Minimal transfer-just 0.04-0.05% of your dose gets into milk. Even better, it’s not sedating for you or your baby.
- Fexofenadine: Almost no transfer into breast milk. Used safely by thousands of nursing mothers.
WebMD, Cleveland Clinic, and the Academy of Breastfeeding Medicine all list these as L1 (safest) category drugs. One mother on BabyCenter wrote: "I’ve taken Zyrtec daily since my baby was 3 months old. He’s 10 months now-never slept more than normal, never missed a feed. No issues."
What About Cough Suppressants?
Dextromethorphan, the active ingredient in most cough syrups like Robitussin DM, is another win. It transfers into breast milk at only 0.1% of your dose. That’s barely measurable. The InfantRisk Center classifies it as L1. It’s not sedating for babies and doesn’t affect feeding or breathing.But avoid combination products. Many cough syrups contain diphenhydramine or codeine under "extra strength" or "nighttime" labels. Always read the ingredients. If you see "PM," "Night," or "All-in-One," skip it. Stick to plain dextromethorphan-only formulas.
Nasal Sprays and Decongestants: What’s Safe?
For stuffy noses, nasal steroids like fluticasone (Flonase) and budesonide (Rhinocort) are ideal. Less than 0.1% of the dose enters your bloodstream-meaning almost nothing reaches your milk. The AAFP recommends them as first-line treatment for allergic rhinitis during breastfeeding.Saline nasal sprays are even safer-zero drugs, just salt water. Use them as often as needed. They work great for congestion without any risk.
Now, avoid oral decongestants like pseudoephedrine (Sudafed). They don’t make babies sleepy-but they can tank your milk supply. One 2003 study showed a 24% drop in milk production within 24 hours of a single dose. That’s not worth the trade-off. If you must use it, do it once, at the lowest dose, and monitor your supply closely.
Timing Matters: When to Take Your Meds
Even if you’re taking a safer med, timing can reduce exposure even further. Here’s what experts recommend:- Take your dose right after you breastfeed-not before.
- If you’re on a 4-6 hour medication like cetirizine, wait 3-4 hours before the next feed.
- Use your baby’s longest sleep stretch (usually overnight) as your dosing window.
Don’t pump and dump unless you’re on something truly dangerous like codeine. Pumping doesn’t speed up drug clearance from your body-it just removes milk you could’ve fed your baby. It also signals your body to make less milk. That’s a double loss.
What to Watch For in Your Baby
Even with "safe" meds, keep an eye out for these signs:- Excessive sleepiness-you can’t wake your baby for a feed
- Shallow or irregular breathing
- Decreased feeding frequency or weak suck
- Unusual fussiness or lethargy
If you notice any of these, call your pediatrician. Don’t wait. In newborns, even mild sedation can lead to poor weight gain or dehydration.

What’s Changed in the Last 5 Years
The landscape has shifted dramatically. Five years ago, codeine was still listed as "probably safe" in many parenting guides. Now? It’s banned for breastfeeding mothers by the Academy of Breastfeeding Medicine. The LactMed database from the NIH now flags 17 medications with sedation risks-up from just 9 in 2018.Over-the-counter brands have caught up too. In 2015, only 42% of allergy meds had "non-drowsy" labels. Now, 68% do. You can find loratadine, cetirizine, and fexofenadine in almost every pharmacy aisle. Look for "non-drowsy," "24-hour," or "daytime" on the box.
Real-Life Decisions: What Should You Do?
You’re not alone in this. Every year, 23% of calls to the InfantRisk Center are about sedation risks from medications. Here’s how to make the right call:- For allergies: Use loratadine or cetirizine daily. Safe, effective, no trade-offs.
- For cough: Use plain dextromethorphan. Skip anything with "PM" or "night."
- For congestion: Try saline spray first. If you need more, use Flonase or Rhinocort.
- Avoid: Codeine, diphenhydramine, hydroxyzine, pseudoephedrine.
If you’re unsure, call the InfantRisk Center or your IBCLC. Don’t guess. There’s no need to suffer-but there’s also no need to risk your baby’s safety.
Final Thought: You’re Not Alone
Breastfeeding while sick is hard. You feel guilty for taking meds. You worry you’re letting your baby down. But choosing the right medicine isn’t selfish-it’s responsible. You’re not just protecting your baby from sedation. You’re protecting your ability to keep feeding them. And that’s the biggest win of all.Is it safe to take Benadryl while breastfeeding?
Benadryl (diphenhydramine) is not recommended while breastfeeding. It can cause drowsiness in infants, especially newborns. Even a single dose has been linked to babies being too sleepy to feed properly. There are safer, non-sedating alternatives like loratadine and cetirizine that work just as well for allergies without the risk.
Can codeine cause death in breastfed babies?
Yes. Codeine has been linked to infant deaths due to respiratory depression. The FDA issued a black box warning in 2017 after multiple cases, including a 13-day-old baby who died after maternal codeine use. This happens because some mothers are ultra-rapid metabolizers, converting codeine into morphine at dangerous levels that pass into breast milk. Codeine is now classified as contraindicated during breastfeeding by major health organizations.
What’s the safest cough medicine for a nursing mom?
Dextromethorphan is the safest cough suppressant for breastfeeding mothers. It transfers into breast milk at only 0.1% of the maternal dose and has no known sedative effects on infants. Avoid combination products that include diphenhydramine, codeine, or pseudoephedrine. Always check the ingredient list.
Do nasal sprays affect breast milk supply?
Nasal steroid sprays like Flonase and Rhinocort have minimal systemic absorption-less than 0.1% of the dose enters your bloodstream-so they don’t affect milk supply. Oral decongestants like pseudoephedrine, however, can reduce milk production by up to 24% within 24 hours. Stick to nasal sprays or saline rinses instead.
Should I pump and dump after taking allergy meds?
Pumping and dumping is rarely necessary. Most medications, even sedating ones, clear from your system naturally over time. Pumping doesn’t speed this up-it just reduces your supply. For safe meds like loratadine or cetirizine, no pumping is needed. For high-risk drugs like codeine, avoid them entirely instead of relying on pumping.
How do I know if my baby is reacting to my medication?
Watch for signs like excessive sleepiness, difficulty waking for feeds, shallow or irregular breathing, weak sucking, or fewer wet diapers. If your baby suddenly becomes unusually quiet or unresponsive, contact your pediatrician immediately. These symptoms can develop quickly, especially in newborns under two months old.


Jigar shah
December 16, 2025Interesting breakdown. I appreciate the clinical references to milk-to-plasma ratios and the FDA black box warning on codeine. This is the kind of evidence-based info I wish more parenting forums had.
BETH VON KAUFFMANN
December 17, 2025Let’s be real - most moms just grab whatever’s on the shelf because they’re sleep-deprived and desperate. The fact that we’re even having this conversation means Big Pharma hasn’t done enough to label OTC meds properly. L1 category? Sounds like marketing jargon to me.
Martin Spedding
December 18, 2025Benadryl is a trap. Saw a friend’s baby go limp after one dose. Never again.
Steven Lavoie
December 19, 2025As someone raised in India where ‘dadi ki dawa’ is still preferred over pills, it’s wild how much we’ve moved from traditional remedies to pharmacological risk assessments. Still - saline sprays and steam? Still the OG solution. No science needed.
Pawan Chaudhary
December 21, 2025Man, I took Zyrtec for 8 months while nursing my twins. No issues at all. My boys are now 2 and super active. You got this, mama!
Raven C
December 23, 2025It’s not just about sedation - it’s about the erosion of maternal autonomy. Why are we being policed for taking medicine? We’re not addicts. We’re caregivers. And yet, every time we try to feel better, someone’s got a black box warning and a spreadsheet.
Erik J
December 24, 2025Did any of the studies control for maternal BMI or infant weight? The 0.14% exposure metric seems arbitrary without context.
Nishant Desae
December 25, 2025Hey, I’m a dad and I read this whole thing because my wife was freaking out about her cold - and honestly? This is the most reassuring thing I’ve seen in weeks. I didn’t know codeine could be deadly for babies - I thought it was just a ‘be careful’ thing. Now I’m double-checking every OTC bottle in the house. Thank you for writing this like you actually care about people, not just data.
Sachin Bhorde
December 26, 2025Bro, I used cetirizine while nursing my girl and she slept like a champ - no weirdness. But I did notice that if I took it at 8pm, she’d wake up at 3am extra hungry. So I switched to morning doses. Simple fix. Also, saline spray FTW. No pills needed.
Anna Giakoumakatou
December 27, 2025Of course the ‘safe’ meds are the ones Big Pharma markets as ‘non-drowsy.’ Coincidence? Or just capitalism solving problems it created? I’ll take my grandma’s honey and lemon, thanks.
Michael Whitaker
December 27, 2025While I appreciate the clinical rigor, I must point out that the assumption that all mothers have access to these ‘L1’ medications is classist. Not everyone can afford Zyrtec over Benadryl. And not every pharmacy stocks fexofenadine in rural areas. This is helpful - but only if you live in a ZIP code with a Whole Foods.
Philippa Skiadopoulou
December 28, 2025Timing the dose post-feed is critical. I’ve seen mothers panic over a single dose of diphenhydramine when a 4-hour delay would have prevented any issue. Education > fear.
Joe Bartlett
December 30, 2025Just took loratadine. Baby’s wide awake. Milk’s fine. Problem solved. Don’t overthink it.
amanda s
December 30, 2025Why are we still talking about this? In America, we have the best medical resources on Earth. If you’re still using Benadryl in 2025, you’re not being careful - you’re being negligent. Get your act together.