Senior Medications: What Works, What to Avoid, and How to Stay Safe
When you’re over 65, taking multiple medications isn’t just common—it’s often necessary. But senior medications, drugs prescribed to older adults to manage chronic conditions like high blood pressure, diabetes, or arthritis. Also known as geriatric pharmacotherapy, it’s a high-stakes game where one wrong pill can lead to falls, confusion, or hospitalization. The average senior takes four to five prescriptions a day, and many more over-the-counter pills or supplements. That’s not just a number—it’s a ticking clock for dangerous interactions.
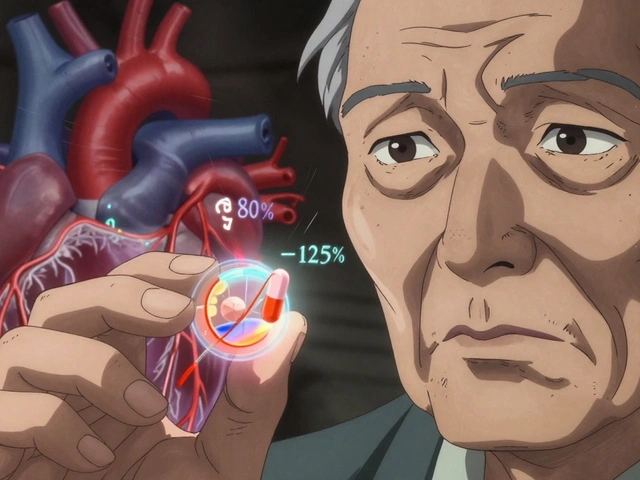
Here’s the problem: your body changes as you age. Your liver and kidneys don’t process drugs the way they did at 30. A dose that was fine years ago might now overload your system. drug interactions, when two or more medications react in harmful ways inside the body. Also known as pharmacodynamic conflicts, it happens more often than you think. Take linezolid, for example—it’s an antibiotic that can spike your blood pressure if you eat aged cheese or drink red wine. Or consider insulin stacking, where giving another dose too soon after the last one crashes your blood sugar. These aren’t rare cases—they’re daily risks for seniors managing multiple conditions.
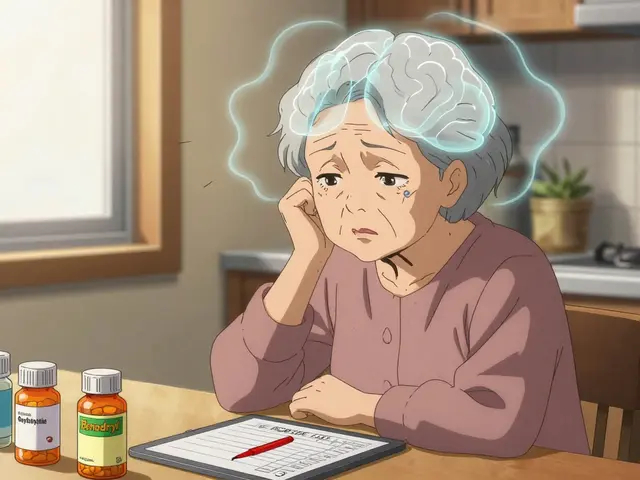
And then there’s polypharmacy, the use of five or more medications at once, often without clear coordination between providers. Also known as medication overload, it is the silent crisis in aging care. One doctor prescribes a blood pressure pill, another adds a sleep aid, a third throws in an anti-inflammatory—all without knowing what the others ordered. The result? Dizziness, memory lapses, fatigue, or worse. Studies show nearly 20% of hospital admissions in seniors are linked to medication errors. And most of those could’ve been avoided with better communication and simpler regimens.
You don’t need to stop taking your meds. You need to understand them. That means asking your pharmacist: "Which of these are absolutely necessary?" Checking with your doctor: "Can any of these be cut or lowered?" And watching for signs like confusion after a new prescription, or falling more often. It’s not about fear—it’s about control. The posts below show real cases: how vitamin deficiencies mess with your cycle, how generic drugs react differently based on your genes, how cost-blind prescribing leaves seniors skipping doses. They reveal the hidden gaps in how senior medications are handled—and how to fix them.