
Many older adults take medications daily to manage common conditions - overactive bladder, allergies, depression, insomnia, or chronic pain. But what if some of these pills are quietly harming their brain? The truth is, the cumulative effect of certain drugs, known as anticholinergic burden, is one of the most underrecognized causes of memory loss and confusion in seniors. Unlike sudden events like strokes or Alzheimer’s, this risk builds slowly, often unnoticed until it’s too late. And here’s the kicker: most people don’t even know they’re taking them.
What Exactly Is Anticholinergic Burden?
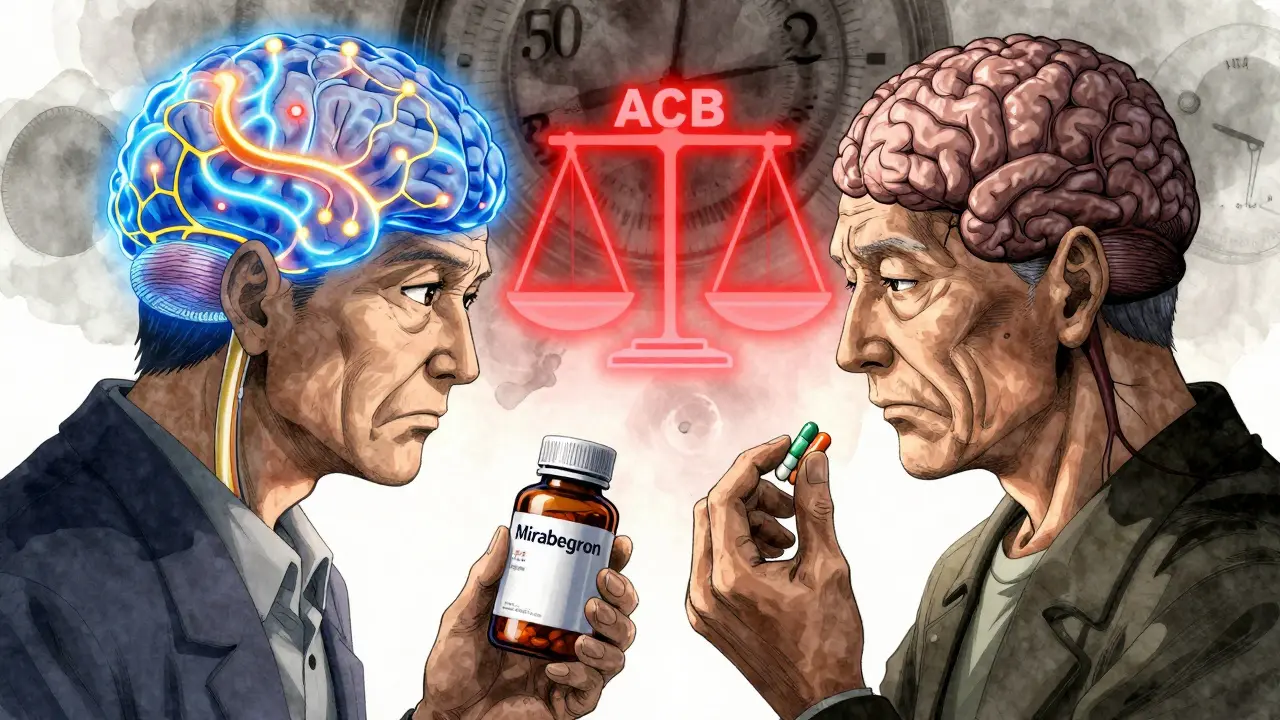
Anticholinergic burden isn’t one drug. It’s the total effect of all the medications you take that block acetylcholine - a brain chemical essential for memory, attention, and learning. Think of acetylcholine as the brain’s messenger for staying sharp. When drugs block it, the signal gets fuzzy. The more drugs you take that do this, the heavier the burden. It’s like turning down the volume on your brain’s most important conversations. The most widely used tool to measure this is the Anticholinergic Cognitive Burden (ACB) scale. It rates drugs from Level 1 (mild) to Level 3 (strong). A single Level 3 drug, like amitriptyline or oxybutynin, can be as damaging as taking three Level 1 drugs together. And here’s what the data shows: older adults with a total ACB score of 3 or higher have a significantly higher risk of dementia. One study found that taking these drugs for three years or more raised dementia risk by 54% compared to short-term use.Which Common Medications Are the Biggest Culprits?
You might be surprised. These aren’t obscure or experimental drugs. They’re the ones you can buy over the counter or get prescribed routinely:- Diphenhydramine - the active ingredient in Benadryl, Unisom, and many sleep aids. It’s a Level 3 anticholinergic. One in five high-burden prescriptions in older adults is this one.
- Oxybutynin - used for overactive bladder. Also Level 3. Many seniors take it for years without knowing it affects their brain.
- Amitriptyline - an old-school antidepressant. Still widely prescribed, even though safer options exist.
- Hydroxyzine - used for anxiety and itching. Often given to seniors for sleep.
- First-generation antihistamines - like chlorpheniramine in cold medicines. They’re everywhere.
How Do These Drugs Actually Damage the Brain?
It’s not just about feeling drowsy. Brain imaging studies show real, measurable harm. In a 2016 study published in JAMA Neurology, people taking medium-to-high anticholinergic drugs had 4% less glucose use in the temporal lobe - the same area that lights up in early Alzheimer’s. Less glucose means less energy for brain cells to function. MRI scans from the Indiana Memory and Aging Study revealed something even more alarming: seniors on these drugs lost brain volume 0.24% faster per year than those not taking them. That’s like losing a teaspoon of brain tissue every year - extra, just from the medication. And the damage isn’t random. It hits specific areas of thinking:- Executive function - planning, organizing, making decisions. This takes the biggest hit. Each point increase in ACB score was linked to a 0.15-point drop per year on tests measuring this.
- Episodic memory - remembering names, events, where you put your keys. Each ACB point added a 0.08-point decline per year.
- Processing speed - how fast you react or think. This was barely affected, which shows the damage is targeted, not general.
Real People, Real Stories
Behind the numbers are real lives. On the AgingCare.com forum, a caregiver named Jen wrote: “My mom’s confusion cleared within two weeks of stopping her bladder medication. Her doctor didn’t even know it was an anticholinergic.” The FDA recorded over 1,200 cognitive-related adverse events in seniors between 2018 and 2022. Confusion was the most common. Memory loss came second. Delirium - sudden, severe mental disorientation - was third. Many of these cases were preventable. A 2021 survey by the National Council on Aging found that 63% of seniors were never told their medication could affect their thinking. And 41% said they’d have chosen a different treatment if they’d known.Can the Damage Be Reversed?
Yes - but it takes time and careful planning. The DICE trial, which followed 286 older adults, showed that after 12 weeks of reducing or stopping anticholinergic drugs, participants improved their Mini-Mental State Exam (MMSE) scores by 0.82 points on average. That’s not a cure, but it’s meaningful. It means better memory, clearer thinking, and more independence. The catch? It doesn’t happen overnight. It takes 4 to 8 weeks for the brain to start recovering. And you can’t just quit cold turkey. Some of these drugs, like antidepressants or bladder meds, need to be tapered slowly under a doctor’s care to avoid withdrawal symptoms or worsening of the original condition.What Can You Do?
If you or a loved one is over 65 and takes multiple medications, here’s what to do:- Make a full list - include everything: prescriptions, over-the-counter drugs, supplements, and herbal remedies.
- Use the ACB Calculator - the American Geriatrics Society launched a free mobile app in 2024. Just type in the names of medications, and it gives you the total anticholinergic burden score.
- Ask your doctor these questions:
- “Is this drug necessary?”
- “Is there a non-anticholinergic alternative?”
- “Could this be contributing to my memory issues?”
- “Can we try reducing or stopping it?”
What Are the Alternatives?
There are safer options for almost every anticholinergic drug:- For overactive bladder: Instead of oxybutynin, try mirabegron (Myrbetriq) or behavioral therapy like bladder training.
- For insomnia: Skip diphenhydramine. Try melatonin, sleep hygiene, or low-dose doxepin (which has minimal anticholinergic effects).
- For depression: Avoid amitriptyline. SSRIs like sertraline or citalopram are safer for the brain.
- For allergies: Use second-generation antihistamines like loratadine (Claritin) or cetirizine (Zyrtec). They don’t cross into the brain the same way.
Why Is This Still Happening?
Despite the evidence, the problem persists. A 2022 study found that only 38.7% of nursing home residents with high anticholinergic scores had their meds reviewed within three months. Primary care doctors say they need 23 minutes per patient to do a full review - but most appointments last 10 to 15 minutes. And here’s the hardest truth: many of these prescriptions are given because they’re cheap, easy, and familiar. Doctors aren’t always aware of the latest guidelines. The American Geriatrics Society’s 2023 Beers Criteria clearly says: avoid strong anticholinergics in older adults. But guidelines don’t change practice unless systems change too.The Bigger Picture
The Lancet Healthy Longevity Commission now ranks anticholinergic burden as one of the top 10 modifiable risk factors for dementia - possibly responsible for 10 to 15% of cases. That’s like saying: if we fixed this, we could prevent 1 in 10 dementia cases. This isn’t about blaming doctors or patients. It’s about awareness. It’s about asking the right questions. It’s about realizing that a pill for a bladder problem might be stealing your grandfather’s memories. The good news? This is one of the few dementia risk factors we can actually control. Unlike genetics or aging, you can change your medications. You can choose safer options. You can protect your brain - one pill at a time.Can anticholinergic drugs cause dementia?
Long-term use of anticholinergic medications is strongly linked to higher dementia risk, especially when taken for three years or more. Studies show a 54% increased risk compared to short-term use. While these drugs don’t directly cause Alzheimer’s, they accelerate cognitive decline by blocking acetylcholine, a key brain chemical for memory and thinking. The risk is dose-dependent and reversible in many cases when the drugs are stopped safely.
What are the most common anticholinergic drugs in seniors?
The most common include diphenhydramine (Benadryl, sleep aids), oxybutynin (for overactive bladder), amitriptyline (an older antidepressant), hydroxyzine (for anxiety or itching), and chlorpheniramine (in cold medicines). These are often prescribed without awareness of their brain effects. First-generation antihistamines and bladder medications are the biggest contributors to high anticholinergic burden in older adults.
Is it safe to stop anticholinergic medications on my own?
No. Stopping some of these drugs suddenly can cause serious side effects like rebound bladder issues, severe anxiety, or withdrawal symptoms. Always work with your doctor to create a safe tapering plan. Cognitive improvements usually take 4 to 8 weeks to appear, and full recovery can take months. A gradual reduction under medical supervision is the safest approach.
Are there safe alternatives to anticholinergic drugs?
Yes. For allergies, use loratadine or cetirizine instead of diphenhydramine. For overactive bladder, mirabegron or behavioral therapy can replace oxybutynin. For depression, SSRIs like sertraline are safer than amitriptyline. For sleep, melatonin or sleep hygiene practices are better than sedating antihistamines. Most conditions have non-anticholinergic options - the key is asking for them.
How can I check my anticholinergic burden?
Use the free ACB Calculator app from the American Geriatrics Society. It’s designed for patients and caregivers. Just enter the names of all your medications - including over-the-counter ones - and it calculates your total anticholinergic score. A score of 3 or higher is considered high risk. Bring the results to your doctor for a medication review.




doug b
January 28, 2026My dad was on Benadryl for sleep for years. One day he couldn’t remember his own birthday. We pulled him off it, and within three weeks, he was back to telling his old stories like nothing happened. Doctors never warned us. Why is this still a thing?
Mel MJPS
January 29, 2026This hit home so hard. My grandma was on oxybutynin and started forgetting how to use the microwave. She thought the TV was talking to her. We didn’t connect it until her pharmacist mentioned anticholinergics. She’s on mirabegron now and acts like a new person. Please, if you’re on any sleep aid or bladder med - check the label. It’s not just ‘getting old.’
Rhiannon Bosse
January 30, 2026Oh, so now Big Pharma is quietly turning seniors into zombies so they’ll need more meds? Classic. They’ve been doing this since the 80s - push the cheap, profitable drugs, ignore the brain damage, then sell you dementia care later. And don’t get me started on how the FDA only ‘updated labels’ after 1,200 cases. That’s not a warning - that’s a funeral notice with a corporate logo. Wake up, people. They don’t care if you forget your keys. They care if you forget to pay your co-pay.
Timothy Davis
January 30, 2026Actually, the 54% increased dementia risk is misleading. That’s from a 2019 JAMA study with confounding variables - people on anticholinergics often have more comorbidities, depression, or poor sleep hygiene. The real causal link isn’t proven. Also, many of these drugs are still first-line because alternatives like mirabegron cost 10x more and aren’t covered by Medicare. This post is fearmongering without context. You can’t just yank meds from elderly patients without considering withdrawal risks. It’s not that simple.
fiona vaz
January 30, 2026I’m a geriatric nurse. I see this every week. A patient comes in confused, and we find they’re on three Level 2+ anticholinergics - Benadryl for allergies, amitriptyline for pain, hydroxyzine for anxiety. We taper them slowly, and within two months, they’re asking about their grandkids’ soccer games again. It’s not magic. It’s just biology. Your brain isn’t broken - it’s just been drowned in static. This is the easiest win in senior care. Talk to your doctor. Bring this list. You’ve got nothing to lose.
Sue Latham
January 31, 2026Wow. So you’re telling me that people who take Benadryl to sleep are just… dumb? Like, is this the new ‘anti-sleep-aid’ movement? Next you’ll say coffee causes dementia because it’s a stimulant. People are just trying to get through the night. Maybe instead of demonizing meds, we should fix the healthcare system that makes 70-year-olds choose between rent and their prescriptions. But no, let’s blame the pills. Classic.
John Rose
February 2, 2026Thank you for this thorough breakdown. I’ve been researching this since my mother’s cognitive decline started. The brain imaging data - particularly the 0.24% annual volume loss - is chilling. What’s not discussed enough is how this burden accumulates silently over decades. A single diphenhydramine here, an amitriptyline there - all add up. The ACB app is a game-changer. I printed my mom’s list, brought it to her PCP, and within a month, two meds were switched. She’s more alert now. This isn’t just medical advice - it’s a lifeline.
Lexi Karuzis
February 3, 2026I’ve been saying this for YEARS!! And who listens? NO ONE!! The doctors are ALL in on it!! They’re paid by the pharma giants!! And the FDA? They’re just puppets!! My neighbor’s husband died from ‘dementia’ - but he was on 5 anticholinergics!! They never tested him!! They never asked!! They just kept prescribing!! It’s a cover-up!! A MASSIVE, CORRUPT, LETHAL COVER-UP!! And now you’re just… telling people to ‘ask their doctor’??!! HA!! They’ll just say ‘it’s fine’!! You need to go public!! Start a petition!! Get on the news!! THIS IS A CRIME!!