Production Halt: Why Drug Supply Chains Break and What It Means for Your Medications
When a production halt, a sudden stop in the manufacturing of a medication due to regulatory, quality, or supply issues. Also known as a drug manufacturing shutdown, it doesn’t just mean empty shelves—it means people can’t get the pills they rely on to stay alive or function daily. This isn’t rare. In 2023, over 300 drugs faced shortages in the U.S. alone, and many of them were generics you’ve never even thought twice about—like digoxin, levothyroxine, or even basic antibiotics. These aren’t niche drugs. They’re the ones your doctor prescribes because they work, they’re cheap, and you’ve been taking them for years.
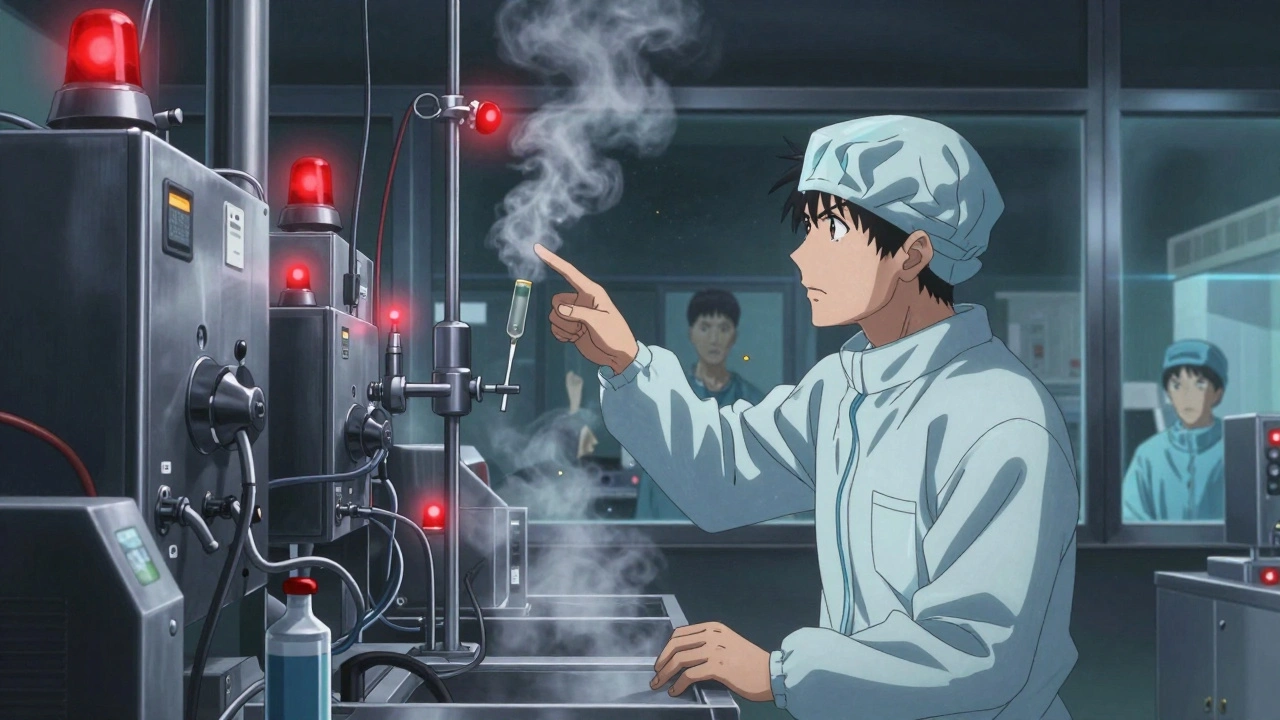
A production halt, a sudden stop in the manufacturing of a medication due to regulatory, quality, or supply issues. Also known as a drug manufacturing shutdown, it doesn’t just mean empty shelves—it means people can’t get the pills they rely on to stay alive or function daily. usually starts with a single factory. Maybe the FDA found contamination. Maybe the company didn’t fix a broken machine. Maybe the raw ingredients stopped coming from overseas because of weather, war, or trade rules. Once that factory shuts down, there’s no backup. Most generic drugs are made in just one or two plants worldwide. When one goes dark, the whole supply chain freezes. That’s why a drug shortage, a situation where the demand for a medication exceeds its supply, often due to manufacturing or distribution failures. Also known as a medication shortfall, it doesn’t just affect hospitals—it affects your kitchen counter, your pill organizer, and your peace of mind. This isn’t theoretical. Look at the digoxin crisis. Patients switching between different generic versions saw dangerous spikes and drops in blood levels. That’s because pharmaceutical manufacturing, the complex, highly regulated process of producing medications under strict quality control standards. Also known as a drug production, it’s not like making soda—it’s more like building a precision watch with chemicals. One tiny change in how a pill is pressed, coated, or mixed can alter how your body absorbs it. And when manufacturers rush to fill gaps after a halt, corners get cut. You don’t always know it’s happening until you feel the difference.
And here’s the kicker: most people don’t realize their medication could vanish overnight. You think your pharmacy has it because they always have it. But pharmacies don’t stockpile. They order what they need week to week. When the factory stops shipping, the pharmacy runs out. Then the doctor gets calls. Then the pharmacist calls around. Then you’re stuck. Some patients get switched to brand names—only to find those cost ten times more. Others get nothing. That’s why medication supply, the continuous flow of drugs from manufacturer to patient, dependent on manufacturing, logistics, and regulatory oversight. Also known as a drug distribution network, it’s only as strong as its weakest link. matters. It’s not about convenience. It’s about safety. It’s about whether your blood pressure stays steady, your thyroid stays balanced, your heart keeps rhythm.
The posts below show you exactly how this plays out in real life. You’ll see how a single production halt in India knocked out digoxin generics across the U.S., how pharmacist substitution rules can help—or hurt—when a drug disappears, and why buying from unlicensed online pharmacies during a shortage is a deadly gamble. You’ll learn how to spot early signs of a shortage before your pharmacy calls, what to ask your doctor when your usual pill isn’t available, and how to track drug availability yourself. This isn’t theory. These are stories from people who ran out of meds and had to fight to get them back. You’re not alone. But you need to know what to do before it happens to you.