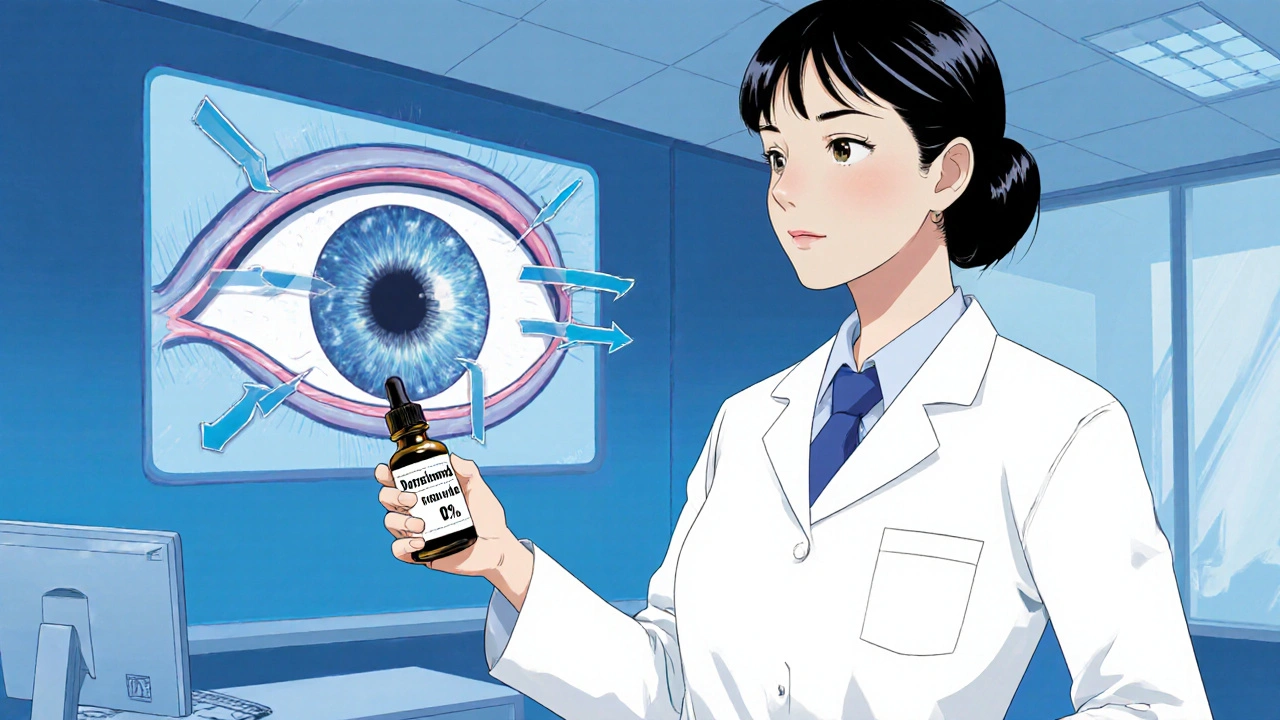
Off-Label Eye Treatments: What Works, What Doesn't, and What Doctors Really Use
When it comes to treating eye conditions, off-label eye treatments, the use of approved medications for unapproved eye conditions. Also known as unapproved indications, it happens more often than you think—especially in ophthalmology, where options for some conditions are limited. The FDA approves drugs for specific uses, but once a medication is on the market, doctors can legally prescribe it for anything they believe will help. This isn’t guesswork—it’s based on clinical experience, peer-reviewed studies, and real patient outcomes.
For example, dry eye, a chronic condition causing irritation, redness, and blurred vision often gets treated with antidepressants like amitriptyline or fluoxetine, even though they’re only approved for depression. Why? Because these drugs affect nerve signaling in the tear glands. Similarly, glaucoma, a group of diseases that damage the optic nerve sometimes gets managed with topical beta-blockers originally meant for high blood pressure, like timolol, which reduce fluid pressure in the eye. These aren’t random choices—they’re targeted, evidence-backed adjustments made because approved eye drops don’t work for everyone.
It’s not just about repurposing pills. Topical antibiotics, antifungals, and even oral medications like doxycycline are used off-label for eyelid inflammation (blepharitis) and meibomian gland dysfunction. One study from the Journal of Ocular Pharmacology and Therapeutics found that over 60% of ophthalmologists regularly prescribe off-label drugs for chronic eye conditions. Patients often don’t even know they’re on an off-label treatment because the doctor doesn’t always mention it—unless they’re asked.
But here’s the catch: off-label doesn’t mean unsafe. It means unapproved for that specific use. The risk isn’t higher than approved uses—it’s just less studied for the eye. That’s why you’ll find many of the posts below diving into exactly this: how drugs like alendronate (used for bones) or selegiline (used for depression) show unexpected effects in other systems, including the eyes. The same principle applies. If a drug changes nerve activity, reduces inflammation, or alters fluid flow, it might help the eye—even if the bottle says otherwise.
What you’ll find here aren’t wild claims or miracle cures. These are real cases, real comparisons, and real patient experiences where off-label use made a difference. Some treatments work wonders. Others fail quietly. All of them reflect how medicine is practiced—not just how it’s labeled.