NTI Drugs: What They Are, Why They Matter, and How to Stay Safe
When a drug has a Narrow Therapeutic Index, a small difference between a safe dose and a toxic one. Also known as NTI drugs, these medications leave almost no room for error—take a little too much, and you risk poisoning; take too little, and the treatment fails. Think of them like walking a tightrope: one misstep, and things go wrong fast. Drugs like warfarin, levothyroxine, phenytoin, and cyclosporine fall into this category. They’re not rare—they’re commonly prescribed. But their danger isn’t widely understood by patients or even some providers.
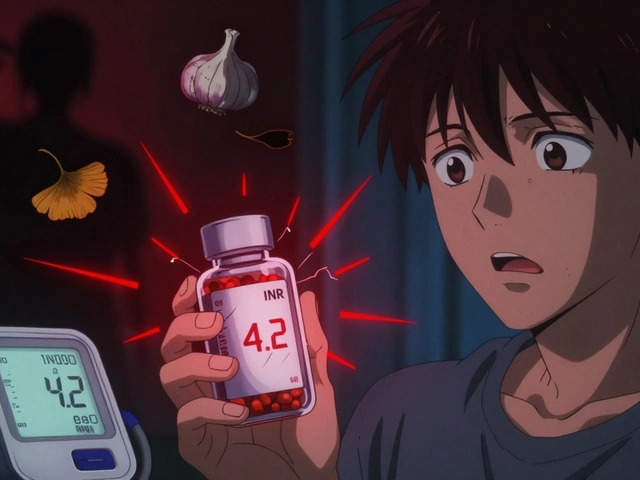
NTI drugs demand precision. That’s why generic substitution, when a pharmacist swaps a brand-name drug for a chemically identical generic version. Also known as bioequivalent drugs, they’re usually safe—but not always with NTI medications. Studies show that even tiny differences in how generics are absorbed can push blood levels into dangerous territory. One patient switching from brand-name warfarin to a generic might see their INR spike overnight, leading to internal bleeding. Another might slip below the therapeutic range, risking a stroke. That’s not theory—it’s documented in emergency rooms across the country. And it’s not just about generics. drug interactions, when two or more medications or supplements interfere with each other’s effects. Also known as medication conflicts, they can turn a stable NTI drug into a ticking time bomb. Think of ginkgo with warfarin, or St. John’s wort with cyclosporine. These aren’t just "may cause" warnings—they’re red alerts. Even something as simple as changing your diet (like eating more leafy greens while on warfarin) can throw your levels off.
NTI drugs aren’t avoided—they’re managed. That means consistent dosing, regular blood tests, and never switching brands or generics without talking to your doctor. It means keeping a full list of everything you take, including herbal supplements and over-the-counter meds. It means asking your pharmacist: "Is this the same as what I was on before?" And it means recognizing that if you feel different after a refill—dizzy, fatigued, unusually bruised, or jittery—you shouldn’t just wait it out. You need to call your provider. The system isn’t perfect. Pharmacists don’t always know your full history. Doctors don’t always check for interactions. But you can be the one who catches the gap.
Below, you’ll find real-world stories and hard facts about how NTI drugs behave in practice: how they interact with other meds, why some people react differently, what happens when you mix them with supplements, and how to spot when something’s gone wrong. These aren’t abstract guidelines—they’re survival tips from people who’ve been there. Whether you’re on one of these drugs now or just want to understand the risks, this collection gives you the tools to stay in control.