Mandatory Substitution: What It Means for Your Medications and How It Affects You
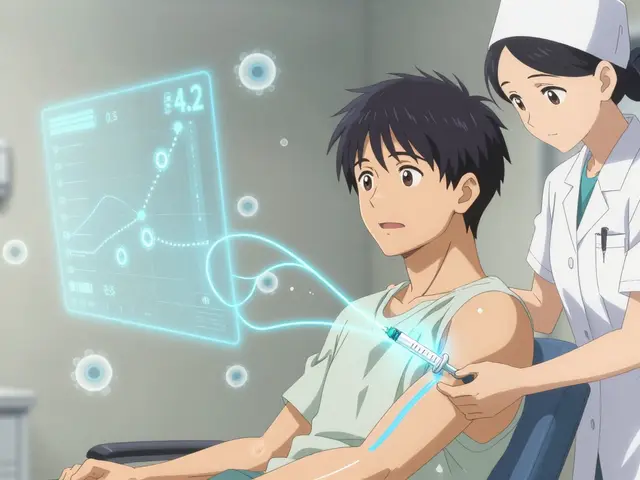
When your pharmacy gives you a generic drug, a lower-cost version of a brand-name medication that contains the same active ingredient. Also known as therapeutic equivalent, it is legally required in many cases under mandatory substitution rules. This isn’t a suggestion—it’s a policy. Insurance companies and state laws often force pharmacies to switch your prescription to the cheapest version available, even if your doctor wrote the brand name. You might not even know it happened until you notice the pill looks different or you feel something off.
Not all generic drugs, medications approved by the FDA as bioequivalent to brand-name versions. Also known as generic equivalents, they work the same for everyone. Some people report differences in side effects, effectiveness, or how quickly the drug kicks in—even though the active ingredient is identical. Why? Because fillers, coatings, and manufacturing processes vary. These differences matter more with drugs like antidepressants, medications used to treat mood disorders where small changes in blood levels can trigger withdrawal or relapse, thyroid meds, hormone replacements where precise dosing affects metabolism and energy, or anti-seizure drugs, medications with narrow therapeutic windows where even minor variations can cause breakthrough seizures. If you’ve ever had a bad reaction after a refill changed, you’re not imagining it.
Mandatory substitution is meant to cut costs, but it doesn’t always save money in the long run. If you end up back at the doctor because the generic didn’t work, or you need extra tests to check your levels, those visits add up. And if you stop taking your meds because the change made you feel worse, that’s a bigger health risk than any savings. You have rights: you can ask for the brand name if your doctor writes "Do Not Substitute" on the prescription, or if you can prove the generic caused problems. Some states allow exceptions for seniors, pregnant people, or those with complex conditions.
The posts below show real cases where drug switching made a difference—whether it was a patient who had to fight their pharmacy to keep their preferred version of alprazolam, or someone who discovered their insulin wasn’t working the same after a generic switch. You’ll find guides on how to check if your meds were substituted, what to ask your pharmacist, and how to document side effects if something goes wrong. This isn’t about resisting generics—it’s about making sure substitution doesn’t become a gamble with your health.