
When you pick up a prescription, you might assume the pharmacist will always give you the cheapest version of your medicine. But that’s not true everywhere. In some states, pharmacists must swap your brand-name drug for a generic. In others, they can only do it if you agree. These differences aren’t just paperwork-they directly affect how much you pay, whether you take your medicine as directed, and even your health outcomes.
What’s the Real Difference Between Mandatory and Permissive Substitution?
Mandatory substitution means the law forces pharmacists to switch your brand-name drug to a generic version-unless your doctor specifically says not to. In these states, the default is generic. Permissive substitution means pharmacists are allowed to substitute, but they don’t have to. They can choose to give you the brand name, even if a cheaper generic is available.
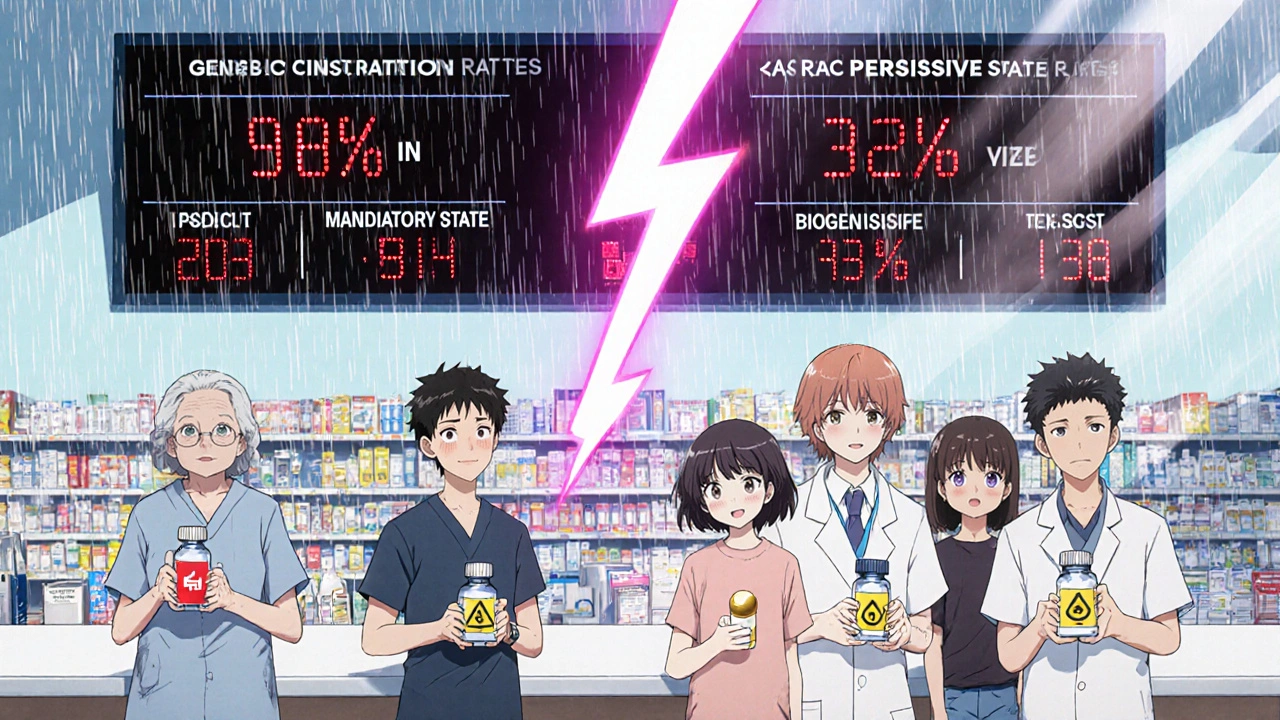
It sounds simple, but the consequences are huge. In states with mandatory substitution, generic drugs are filled at rates nearly 20% higher than in permissive states. For example, after the patent expired for simvastatin (a common cholesterol drug), 48.7% of prescriptions in mandatory states were filled with generics. In permissive states? Only 30%. That’s a massive gap in access and cost savings.
Why Do States Have Different Rules?
The federal government doesn’t control this. Back in 1984, Congress passed the Hatch-Waxman Act, which created the modern system for approving generic drugs. But instead of forcing states to allow substitutions, they left it up to each state legislature. That’s why today, you’ve got a patchwork of rules.
As of 2020, 19 states-including Alabama, Alaska, Colorado, Indiana, and West Virginia-require pharmacists to substitute generics unless the prescriber blocks it. The rest operate under permissive rules. Some states, like California and New York, used to be in the permissive camp but have moved toward mandatory over time. The trend is clear: more states are adopting mandatory substitution because it cuts costs and improves adherence.
What Else Do These Laws Control?
It’s not just about whether substitution is required. States also decide:
- Whether you must be notified when a substitution happens
- Whether you have to give explicit consent
- Whether pharmacists are protected from lawsuits if something goes wrong after substitution
Thirty-one states and Washington, D.C., require pharmacists to tell you they switched your drug-beyond just the label on the bottle. Seven states plus D.C. require you to sign off on the switch. That consent rule makes a huge difference. In states where consent isn’t needed, generic use for simvastatin hit 98.1%. In states that required consent? Only 32.1% of prescriptions were filled with generics.
And here’s the scary part: 24 states don’t protect pharmacists from liability if a patient has a bad reaction after a generic substitution. That means pharmacists in those states might avoid substituting-even when it’s safe-just to stay out of legal trouble.
How Do Doctors Stop Substitution?
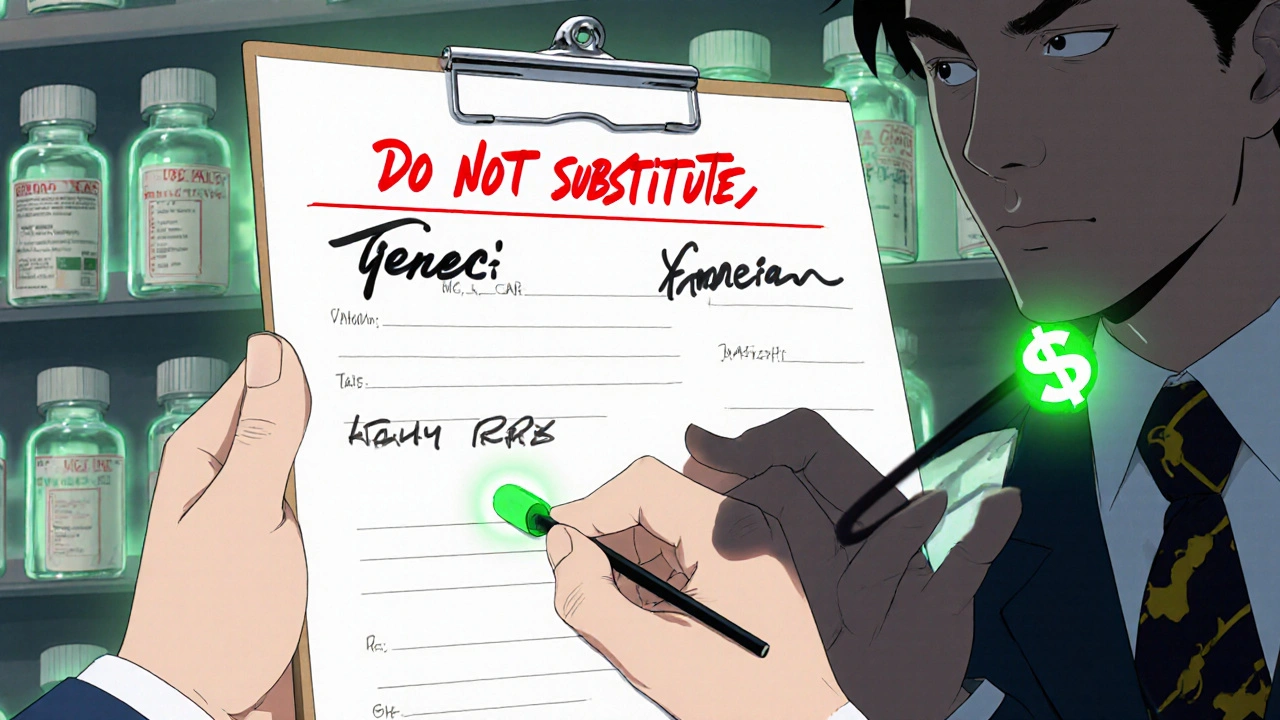
Every state lets doctors block substitution. They write “Dispense as Written,” “Do Not Substitute,” or “Brand Medically Necessary” on the prescription. But how they do it varies.
In some states, prescriptions come on two-line forms: one line for the drug name, another for the prescriber’s signature. If the doctor signs on the second line, substitution is allowed. If they sign on the first, it’s blocked. In other states, there’s no special form. The doctor has to write out the phrase in full. That creates confusion-especially if a patient gets a prescription from a doctor in a different state.
Some states even require doctors to justify why they’re blocking substitution. That’s meant to prevent unnecessary brand-name prescriptions. But in practice, many doctors just write “Do Not Substitute” without explaining why-especially for drugs with narrow therapeutic indexes, like warfarin or lithium, where tiny dosage changes can be dangerous.
Biosimilars Are a Whole Different Ballgame
Generic drugs are copies of simple chemical medicines. Biosimilars are copies of complex biologic drugs-like those used for rheumatoid arthritis, cancer, or Crohn’s disease. These are harder to replicate. So states treat them differently.
Forty-five states have stricter rules for biosimilars than for regular generics. Most require the prescribing doctor to be notified before substitution happens. Only nine states and D.C. treat biosimilars the same as small-molecule generics. That’s because switching between biologics can trigger immune reactions, and long-term data on switching is still limited.
As biologics make up 42% of Medicare Part D spending (even though they’re only 2% of prescriptions), these rules will shape future healthcare costs. States are moving slowly here-rightly so-but the pressure to cut costs will keep pushing them toward more substitution, even with biologics.
What This Means for You
If you’re on a chronic medication-like high blood pressure pills, antidepressants, or insulin-you’re probably paying more than you need to if you live in a permissive state. In mandatory states, you’re getting the generic by default. That means lower copays, fewer out-of-pocket costs, and better chances you’ll stick with your treatment.
But if you’re in a state that requires consent, you might not even know a substitution happened. Pharmacists are busy. If they don’t have to tell you, they often won’t. And if you don’t ask, you might end up with the brand name, even if the generic is just as safe.
Here’s what to do: Always check your prescription label. If the name doesn’t match what your doctor wrote, ask. If you’re in a state with mandatory substitution and your doctor didn’t block it, you should get the generic. If you don’t, ask why. And if you’re on a narrow therapeutic index drug, make sure your doctor explicitly says “Do Not Substitute.”
What This Means for the System
The savings from generic substitution are massive. Generics cost 80-85% less than brand-name drugs. The Congressional Budget Office estimated that a 1% increase in generic use saves Medicare Part D $160 million a year. Multiply that by the 18.7 percentage point gap between mandatory and permissive states, and you’re talking about billions in potential savings.
Pharmaceutical companies know this. That’s why brand-name manufacturers spend millions lobbying in permissive states-running ads, funding patient advocacy groups, and training doctors to write “Dispense as Written.” Their goal? Keep you on the expensive brand.
But the real winners are patients and taxpayers. Lower costs mean fewer people skip doses because they can’t afford their meds. Fewer skipped doses mean fewer hospital visits, ER trips, and complications. That’s better health-and cheaper care-for everyone.
What’s Changing?
The number of mandatory substitution states has grown from 14 in 2014 to 19 in 2020. That trend is likely to continue. As biosimilars become more common, states will need to update their laws. Some will tighten rules. Others will loosen them to save money.
One thing’s certain: the system won’t stay the same. If you’re managing a chronic condition, stay informed. Know your state’s rules. Ask questions. And don’t assume the pharmacy will do the right thing unless the law forces them to.
What’s the difference between mandatory and permissive substitution?
Mandatory substitution means pharmacists are legally required to give you a generic version of your drug if it’s available and approved, unless your doctor says not to. Permissive substitution means pharmacists can choose to substitute, but they’re not required to. In permissive states, you might still get the brand-name drug even if a cheaper generic exists.
How do I know if my state requires substitution?
Check your state’s board of pharmacy website or call your local pharmacy. As of 2025, 19 states require substitution, including Alabama, Alaska, Colorado, Indiana, and West Virginia. The rest are permissive. If your prescription is filled with a brand-name drug and your doctor didn’t block substitution, ask why.
Can I refuse a generic drug even if my state mandates substitution?
Yes. You can always ask for the brand-name drug, even in mandatory states. But you’ll likely pay more out of pocket. In some cases, your insurance won’t cover the brand if a generic is available. Your pharmacist can tell you what your copay will be for each option.
Why do some states require patient consent for substitution?
Some states believe patients should have a say in what they take, especially with drugs that have narrow therapeutic indexes. But research shows consent requirements drastically reduce generic use-dropping it from nearly 100% to under one-third. These rules often benefit drug manufacturers more than patients, because they create friction that keeps people on expensive brands.
Are biosimilars treated the same as generic drugs?
No. Biosimilars-copies of complex biologic drugs-are subject to stricter rules in 45 states. Most require the prescriber to be notified before substitution, and some require explicit consent. This is due to concerns about immune reactions and limited long-term data on switching. As biosimilars become more common, these rules are likely to evolve.
What should I do if I think I was given the wrong drug?
Always check the name on your prescription label against what your doctor wrote. If they don’t match, ask the pharmacist why. If you’re on a drug with a narrow therapeutic index-like warfarin, lithium, or levothyroxine-ask your doctor to write “Do Not Substitute” on your prescription. Never assume the pharmacy made the right choice without confirming.
What’s Next?
If you’re on a long-term medication, your best move is to know your state’s rules and speak up. Don’t wait for the pharmacy to explain. Ask: “Is this a generic? Is substitution required here?” If you’re paying more than you should, you have the right to push back.
And if you’re a caregiver, parent, or someone managing multiple medications, this knowledge is power. The difference between mandatory and permissive substitution isn’t just legal jargon-it’s the difference between paying $10 or $80 for your pill, between taking your medicine every day or skipping it because it’s too expensive.
Stay informed. Ask questions. And make sure the system works for you-not just the companies.




Sameer Tawde
November 19, 2025Love this breakdown. In India, generics are the norm and people don’t even blink. If your medicine costs less and works the same, why pay extra? It’s not magic-it’s chemistry.
Jeff Hakojarvi
November 20, 2025my doc always writes 'do not substitute' on my blood pressure med but i never asked why... maybe i should. i’ve been paying $75 for a pill that’s $8 elsewhere 😅
Timothy Uchechukwu
November 20, 2025why do we even care what some pharmacist does its not like they know medicine anyway the real problem is the government letting big pharma control everything and now they want to force generics on us like its some kind of socialist plot
Ancel Fortuin
November 21, 2025Consent requirements? Yeah right. That’s just a backdoor way to keep people on brand-name drugs while pretending to care about ‘patient autonomy.’ Funny how the same people who scream about bodily autonomy don’t care when it costs them $80 instead of $8.
Samkelo Bodwana
November 23, 2025I’ve been thinking about this a lot since my mom got switched to a generic for her thyroid med last year. She was terrified at first-said she’d been on the brand for 12 years and ‘it just worked.’ But after two months, her labs were better, her energy improved, and she saved $1,200. The fear is real, but so is the data. Maybe we need better education, not more legal barriers.
Also, the liability thing is wild. Pharmacists are getting sued for giving you a cheaper version that’s FDA-approved? That’s like suing a grocery store for selling store-brand cereal instead of Cheerios. The system’s broken.
And biosimilars? Yeah, they’re complex, but we’ve been switching biologics in Europe for over a decade without mass immune meltdowns. The U.S. is still acting like we’re testing this on lab rats.
Doctors need training too. Not everyone knows how to write ‘Dispense as Written’ correctly. I’ve seen prescriptions where the doctor signed on the wrong line and the pharmacy gave the brand anyway. No one knew until the bill came.
We need a national standard. Not because the feds should control everything, but because patients shouldn’t have to Google their state’s pharmacy laws just to afford their meds.
And honestly? If you’re on warfarin or lithium and you’re not already asking for a generic, you’re playing Russian roulette with your kidneys.
kim pu
November 23, 2025generic? more like generic-ly priced. Big pharma’s got lawyers on speed dial to make sure you never even see a $5 pill. And don’t get me started on ‘therapeutic equivalence’-it’s a marketing term dressed up like science. I’ve seen generics that look like they were made in a garage.
Also-why are we still using paper scripts? This is 2025. My phone can order pizza, but my doctor still scribbles on a sticky note like it’s 1998.
malik recoba
November 24, 2025i never knew this was a thing. i just assumed the pharmacy gave me the cheapest one. i just found out my insulin is $100 because my state is permissive and my doc never blocked it. wow.
Angela J
November 26, 2025Did you know the FDA gets funding from big pharma? And that’s why they approve generics so fast. It’s all a scheme. They want you sick so you keep buying. That’s why they won’t let you know when they switch your med. They’re watching you through your pill bottle.
Also, I think the pharmacist is a spy. My last bottle had a different color cap. I swear they replaced it with something else. I checked the batch number. It was different. I’m not crazy. I’ve seen it.
Hannah Blower
November 27, 2025Let’s be real: mandatory substitution isn’t about cost-it’s about eroding patient agency under the guise of efficiency. You think you’re saving money? You’re just becoming a cog in a corporate healthcare machine that reduces human beings to dosage units.
The real tragedy? We’ve normalized the idea that health is a commodity. That your life’s quality can be determined by a state’s legislative whim. We don’t need more laws-we need a revolution in how we think about care.
And biosimilars? Don’t even get me started. They’re not ‘copies.’ They’re approximations. Biologics are living molecules. You can’t replicate a protein the way you replicate aspirin. This isn’t substitution-it’s pharmacological alchemy with unpredictable consequences.
And yet, the media glorifies this as ‘progress.’ Meanwhile, the patients who die from immune reactions? They’re just ‘statistical noise.’
Ask yourself: Who benefits when a patient can’t afford their medication? Not the patient. Not the pharmacist. Not the doctor. The shareholder.
Gregory Gonzalez
November 29, 2025Oh look, another think piece on how generics are ‘good for society.’ Tell that to the guy whose depression got worse after switching to a generic SSRI because the fillers were different. Oh wait-you won’t. Because your data ignores the 1% who suffer.
‘Cost savings’ is just corporate speak for ‘we don’t care if you feel like a zombie.’
Ronald Stenger
November 30, 2025States that allow substitution are letting big pharma off the hook. Why? Because they’re owned by the same lobbyists who fund the FDA. This isn’t healthcare-it’s a corporate takeover dressed in white coats.
And don’t tell me ‘generics are safe.’ My cousin got hospitalized after switching. The pharmacy didn’t even notify him. That’s not freedom. That’s negligence.
Emily Entwistle
December 1, 2025OMG I just checked my state and we’re permissive 😱 I’ve been overpaying for years. I’m calling my doctor tomorrow. Also, I’m sending this to my mom-she’s on 7 meds and has no idea. 💪💊 #GenericRevolution 🙌
Duncan Prowel
December 1, 2025While the economic rationale for mandatory substitution is compelling, one must also consider the epistemological asymmetry between regulatory frameworks and clinical reality. The assumption that pharmacokinetic equivalence guarantees therapeutic equivalence remains, in many cases, empirically unsubstantiated.
Furthermore, the legal liability landscape-particularly in jurisdictions lacking indemnification for pharmacists-introduces a perverse incentive structure wherein risk aversion supersedes cost-efficiency. This phenomenon, observable in the 32.1% substitution rate under consent regimes, suggests that patient safety concerns are not merely rhetorical, but structurally embedded in the system.
One might posit that the solution lies not in binary legal mandates, but in layered, tiered protocols calibrated by drug class, therapeutic index, and patient history. A one-size-fits-all approach is, frankly, a relic of 20th-century bureaucratic thinking.
Bruce Bain
December 2, 2025Man, I’m from Texas and we’re permissive. I didn’t even know this was a thing. My grandma takes blood thinners and she just gets whatever the pharmacy gives her. I’m gonna sit her down and explain this. She’s on a fixed income. She deserves to save money.
Don Angel
December 2, 2025Wait… so if I live in a mandatory state, and my doctor didn’t block it, but I still got the brand-name drug… is that illegal? Do I have a right to a refund? I’m confused. And also, why do pharmacies still use those tiny labels that you need a magnifying glass to read? 🤦♂️