Asthma Types: Understanding Triggers, Symptoms, and Treatment Differences
When people talk about asthma, a chronic lung condition that causes airways to narrow, swell, and produce extra mucus. Also known as bronchial asthma, it affects over 26 million people in the U.S. alone. But not all asthma looks the same. Some folks wheeze only during pollen season, others struggle after exercise, and some can’t sleep because their airways tighten at night. The type you have changes how you treat it, what triggers it, and even what meds work best.
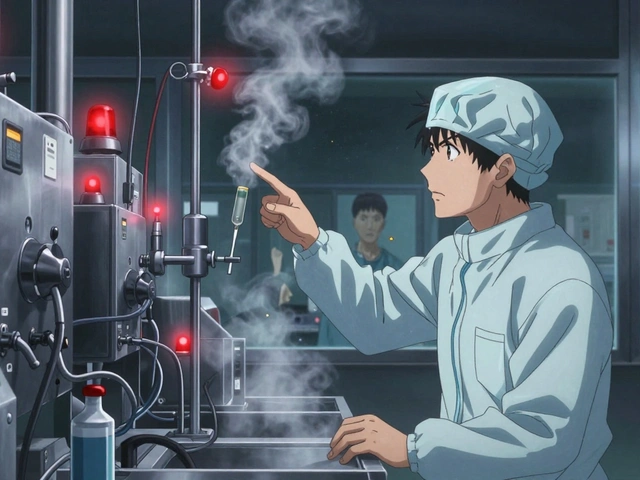
Allergic asthma, the most common form, happens when your immune system overreacts to things like dust mites, pet dander, or mold. You’ll notice symptoms spike around certain seasons or after being near pets. Then there’s non-allergic asthma, triggered by cold air, stress, smoke, or infections—not allergens. This one doesn’t show up on allergy tests, so it’s often missed or misdiagnosed. Exercise-induced asthma, also called EIA, hits during or right after physical activity, even in people without other asthma symptoms. And occupational asthma, caused by workplace irritants like chemical fumes, dust, or gases, affects workers in factories, farms, or labs. Each type needs a different approach.
Knowing your asthma type isn’t just about labels—it’s about survival. If you have allergic asthma, avoiding triggers like ragweed or keeping your home dust-free can cut flare-ups in half. But if you have exercise-induced asthma, you might need a quick-relief inhaler before workouts, not just daily steroids. People with occupational asthma might need to change jobs or use better ventilation. Even your meds can vary: some respond well to inhaled corticosteroids, others need leukotriene modifiers or biologics. The wrong treatment doesn’t just waste time—it can land you in the ER.
What you’ll find below isn’t a generic list of asthma facts. These are real stories and data-driven posts about how people manage their specific type—whether it’s controlling nighttime symptoms with the right inhaler timing, avoiding drug interactions that worsen breathing, or understanding why some asthma meds don’t work for everyone. You’ll see how medication safety, drug substitutions, and even environmental factors like air quality play into daily control. No fluff. Just what works—and what doesn’t—for different kinds of asthma.