
Taking multiple medications is common-especially as you get older or manage chronic conditions. But mixing drugs without checking for interactions can lead to serious side effects, hospital visits, or even life-threatening reactions. A drug interaction checker is one of the simplest, most powerful tools you can use to stay safe. Whether you’re a patient, caregiver, or healthcare worker, knowing how to use one correctly can prevent harm before it happens.
What Is a Drug Interaction Checker?
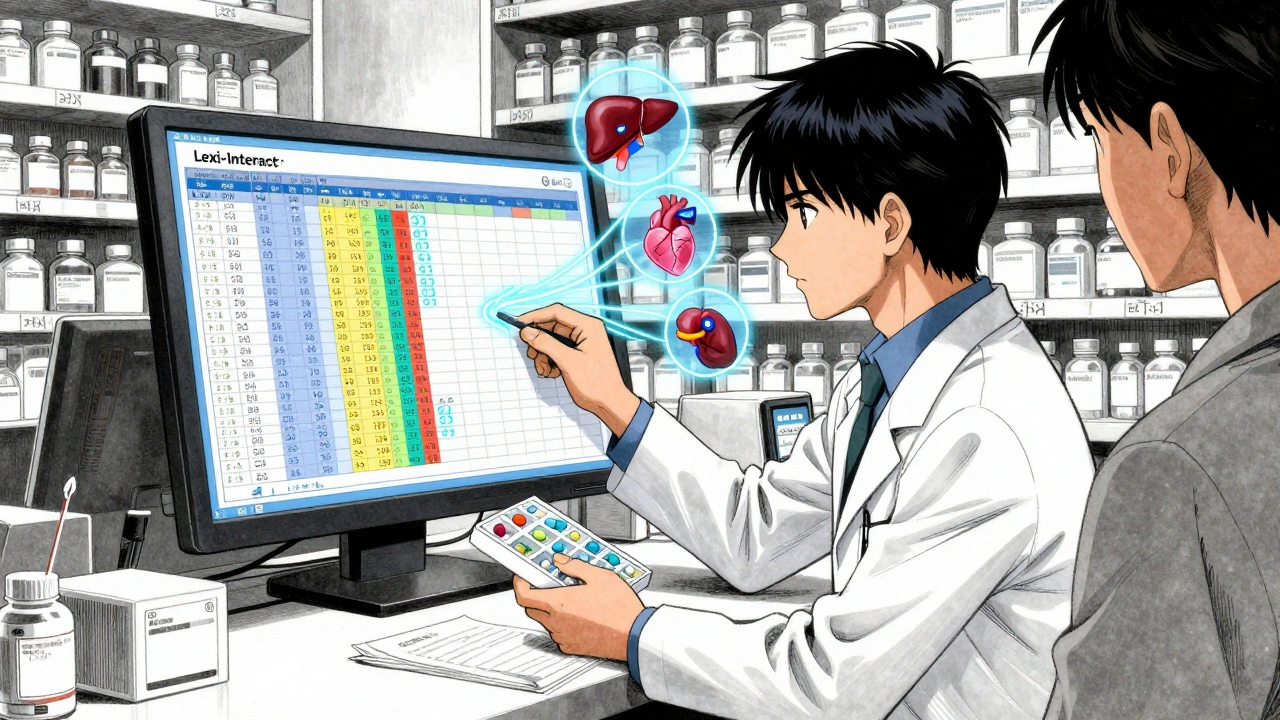
A drug interaction checker is a digital tool that scans the medications, supplements, or even foods you’re taking and flags combinations that could cause problems. These problems aren’t always obvious. For example, taking ibuprofen with warfarin might seem harmless, but it can increase your risk of bleeding. Or combining certain antibiotics with statins can damage your muscles. These tools don’t guess-they use databases built from years of clinical research to predict what might go wrong. There are two main types: consumer apps and professional systems. Consumer apps like Medisafe or Epocrates are designed for everyday users. They’re easy to use on your phone and give you quick alerts. Professional systems like Micromedex, Lexi-Interact, or DrugBank are used in hospitals and pharmacies. They’re more detailed, integrate with electronic health records, and include data on rare interactions-but they require training to use properly.Why You Should Use One
About 44% of adults over 65 take five or more medications daily. That’s a recipe for accidental clashes. The U.S. Agency for Healthcare Research and Quality estimates that preventable drug interactions cause over $2.2 billion in medical costs every year-and countless hospitalizations. A 2022 study showed that clinical decision support tools like interaction checkers prevent around 1.5 million adverse drug events annually in U.S. hospitals alone. But it’s not just about hospitals. A user on Medisafe reported that the app caught a dangerous interaction between warfarin and ibuprofen before they had a serious bleed. That’s the kind of real-life safety net these tools provide. Even if you think you know your meds, your memory isn’t perfect. A checker doesn’t forget.Step-by-Step: How to Use a Drug Interaction Checker
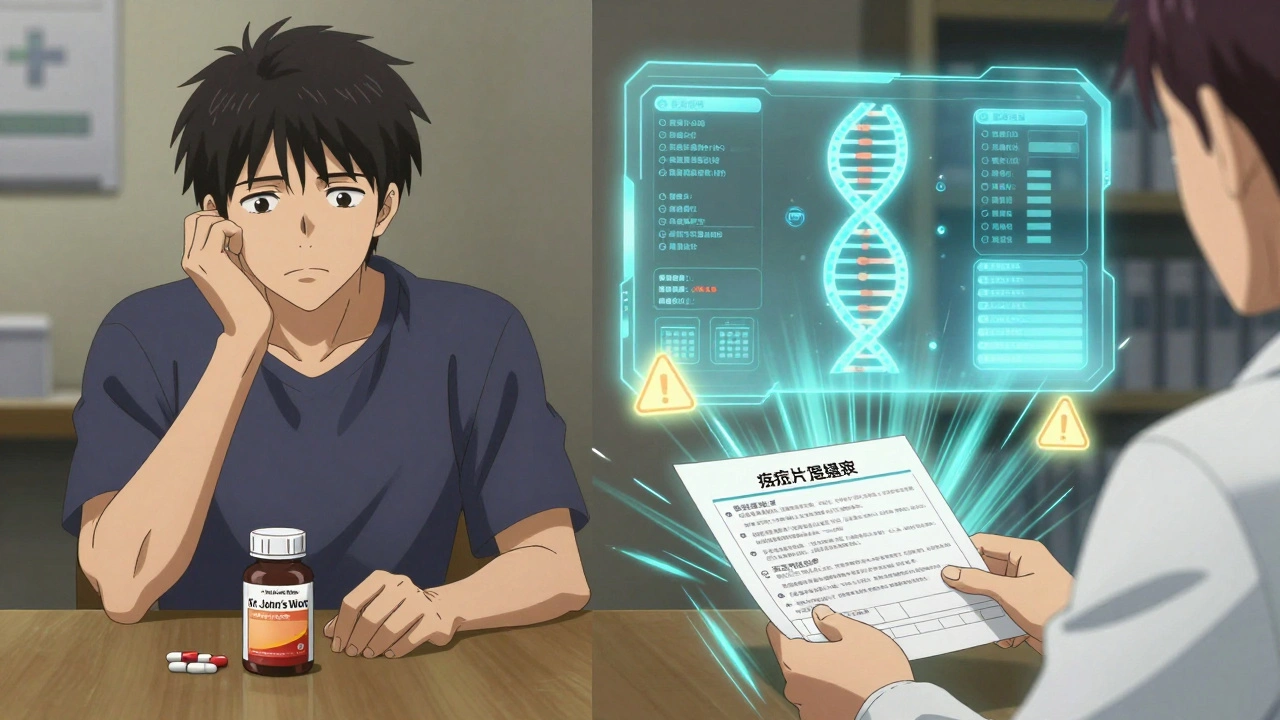
Using a drug interaction checker is straightforward-but only if you do it right. Here’s how:- Start with a complete list of everything you take. This includes prescription drugs, over-the-counter meds (like painkillers or antacids), vitamins, herbal supplements (like St. John’s Wort or turmeric), and even recreational substances like alcohol. Many people forget supplements, but they’re just as likely to interact as pills.
- Choose your tool. If you’re a patient, use a consumer app like Medisafe or Epocrates. If you’re a clinician, use a hospital system like Micromedex or Lexi-Interact. Don’t mix tools unless you’re cross-checking for accuracy.
- Enter each medication one at a time. Type the name exactly as it appears on the bottle. Don’t abbreviate. For example, type “ibuprofen 200 mg” instead of “Advil.” Some tools let you scan barcodes or select from a dropdown list-use those options if they’re available. Avoid typing vague names like “blood pressure pill.” Be specific.
- Confirm the formulation and route. This matters more than you think. Oral aspirin and topical aspirin cream can have different interactions. DrugBank’s system requires this step because the route changes how the drug behaves in your body. If your tool lets you choose “oral,” “topical,” or “injectable,” pick the right one.
- Review the results carefully. Results are usually color-coded: red means stop taking them together, orange means monitor closely, yellow means note it but no action needed, and green means safe. Don’t ignore yellow. Some interactions cause slow, cumulative damage. Click on any information icon next to a result-it’ll explain why it’s flagged and what symptoms to watch for.
- Don’t skip the details. Many users see “possible interaction” and assume it’s not serious. But a 2021 study found that 37% of dangerous combinations were missed because people ignored low-severity alerts. Read the description. Is it about liver stress? Kidney strain? Heart rhythm? That tells you how urgent it is.
- Share the results with your pharmacist or doctor. Even the best tool can miss something. A 2023 survey found that 68% of pharmacists use at least two interaction checkers and still double-check manually. Don’t rely on automation alone.
Top Tools Compared
Not all checkers are created equal. Here’s how the most popular ones stack up:| Tool | Best For | Accuracy | Ease of Use | Special Features |
|---|---|---|---|---|
| Medisafe | Patients and caregivers | Good | Very easy | Syncs with pill reminders, iOS/Android, alerts via app |
| Lexi-Interact | Hospitals and pharmacists | Excellent | Medium | Most comprehensive database, integrates with Epic and Cerner |
| DrugBank | Developers and researchers | Excellent | Hard (requires technical skill) | API for custom apps, includes supplements and food interactions |
| University of Liverpool DDI Checker | COVID-19 or infectious disease patients | Excellent for targeted use | Easy | Visual color system, free, updated for long-COVID treatments |
| Epocrates | Doctors and nurses | Good | Very easy | Fast lookup, 82% satisfaction on speed, 63% on accuracy |
Pitfalls to Avoid
Even the best tools have flaws. Here’s what goes wrong-and how to fix it:- False alarms. Some tools flag every possible interaction, even ones that are extremely rare or clinically insignificant. Micromedex users report up to 30 irrelevant alerts per search. Solution: Don’t panic. Look at the severity level. If it’s yellow or green, ask your pharmacist if it’s worth worrying about.
- Missed names. Generic names aren’t always recognized. If “metoprolol” doesn’t show up, try “Lopressor.” If “sertraline” fails, try “Zoloft.” Some tools are better with brand names, others with generics.
- Outdated data. New interactions are discovered all the time. A 2023 update to DrugBank added over 200 new supplement interactions. Make sure your app or system is updated. Consumer apps auto-update; hospital systems require IT admin approval.
- Over-reliance. A 2023 Medscape study found clinicians ignored nearly half of all DDI alerts because they’d been trained to “tune out” noise. Don’t be that person. Always think: Is this interaction relevant to me? Does it match my symptoms? Is there a safer alternative?
When to Trust the Tool-and When to Call Your Pharmacist
A drug interaction checker is a guide, not a doctor. It doesn’t know your full medical history, kidney function, allergies, or other conditions that change how your body handles drugs. That’s why experts say no tool has more than 85% sensitivity. That means 1 in 7 dangerous interactions might slip through. You should always consult a pharmacist if:- The checker flags a red alert and you’re unsure what to do.
- You’re taking more than five medications.
- You’ve recently been hospitalized or had a change in health.
- The interaction involves blood thinners, heart meds, seizure drugs, or antidepressants.
What’s Next for Drug Interaction Checkers
The field is evolving fast. New systems now use AI to reduce false positives-Lexicomp’s 2023 update cut them by 22%. Some hospitals are testing tools that factor in your genetics. Mayo Clinic’s pilot program showed that combining DNA data with interaction checkers improved accuracy by 31%. The FDA is also pushing vendors to use real-world patient data from its Sentinel Initiative, making predictions more accurate over time. But the biggest change? Integration. More apps now link directly with your pharmacy’s system. If you use Medisafe, your pharmacist might soon see your interaction alerts too. That means fewer mistakes and better teamwork.Final Thoughts
You don’t need to be a doctor to use a drug interaction checker. You just need to be careful. Taking a few minutes to check your meds before you start a new one can save you from a hospital stay, a dangerous side effect, or worse. Use the tool. Read the results. Ask questions. Don’t assume it’s fine because “it’s just a supplement.” The safest people aren’t the ones who know the most about drugs. They’re the ones who check-and double-check.Can I use a drug interaction checker if I’m not a healthcare professional?
Yes. Many tools like Medisafe, Epocrates, and the University of Liverpool’s DDI Checker are designed for patients and caregivers. They’re free, easy to use on your phone, and give clear warnings. Just make sure you enter all your medications-including vitamins and supplements-and always share the results with your pharmacist or doctor.
Are drug interaction checkers 100% accurate?
No. Even the best systems miss about 15% of dangerous interactions. Accuracy depends on the tool, how up-to-date it is, and whether you entered the right drug names and doses. That’s why experts recommend using more than one tool if you’re unsure, and always confirming with a pharmacist.
What if my drug isn’t in the checker?
Try typing the generic name instead of the brand name. If that doesn’t work, check the manufacturer’s website or contact your pharmacist. Some newer supplements or experimental drugs aren’t in databases yet. When in doubt, don’t assume it’s safe-ask a professional.
Can food or alcohol cause interactions too?
Yes. Grapefruit juice can make some statins dangerously strong. Alcohol can increase drowsiness with sedatives or painkillers. Some interaction checkers, like DrugBank and Medisafe, include food and alcohol interactions. Always check for them-especially if you drink regularly or eat a lot of citrus fruits.
How often should I check for interactions?
Check every time you start a new medication, stop one, or change the dose. Also check if you’ve added a new supplement or started drinking more alcohol. Even if nothing changed, review your list every six months. Your body and your meds can change over time.
Do I need to pay for a drug interaction checker?
No. Many reliable tools are free. The University of Liverpool’s checker, Medisafe, and Epocrates offer free versions. Hospital systems like Micromedex cost money, but you don’t need them unless you’re a clinician. Stick to free, trusted apps for personal use.



Norene Fulwiler
December 5, 2025I’ve been using Medisafe for my mom’s meds since she started on seven different pills last year. It caught a dangerous combo between her blood thinner and a common NSAID she was taking for arthritis-she’d been doing it for months without knowing. We called her pharmacist right away and switched her to acetaminophen. That app literally saved her from a bleed. Honestly, if you’re managing multiple meds, this isn’t optional-it’s survival.
And yes, even the ‘harmless’ supplements like turmeric or fish oil can mess with your meds. Don’t underestimate them.
Harry Nguyen
December 6, 2025Of course the government wants you to rely on apps. Meanwhile, the real solution is fewer prescriptions. Stop letting Big Pharma push you into polypharmacy. You don’t need five drugs to manage ‘chronic conditions’-you need better food, sleep, and less stress. But no, let’s just slap a QR code on your pill bottle and call it healthcare innovation.
Also, ‘DrugBank’? That’s not a tool, it’s a corporate data mine. You think they’re helping you? They’re selling your meds profile to insurers.
Mark Ziegenbein
December 7, 2025Let me tell you about the time I spent three hours cross-referencing every single item in my mother’s medicine cabinet across five different interaction checkers because I refused to trust any single database. Medisafe flagged warfarin and St. John’s Wort-obvious. But Lexi-Interact didn’t even list the interaction between her magnesium supplement and her thyroid med until I manually typed in the chemical compound name. DrugBank? It gave me a 17-page PDF with citations from 1989. I had to call a pharmacist just to confirm whether the ‘yellow’ alert meant ‘probably fine’ or ‘you’re one sip of grapefruit juice away from the ER.’
And don’t get me started on Epocrates. It’s like using a Swiss Army knife to open a can of soup-convenient, but you’re not actually sure if you’re getting the right blade. The real problem isn’t the tools-it’s that we’ve outsourced our medical literacy to apps that don’t know if you’re 78 or 28, if you’re diabetic, if you’ve got kidney disease, or if you’re just trying to survive on a fixed income while your doctor won’t return your calls.
These tools are not magic. They’re mirrors. And if you walk into the mirror with incomplete data, you’re not going to see your reflection-you’re going to see a glitch.
Stephanie Bodde
December 8, 2025Yessss this is so important!! 🙌 I used to think supplements were ‘natural’ so they were safe-until my aunt had a scary episode after mixing her antidepressant with kava root. Now I check EVERYTHING-even the gummy vitamins. My phone’s Medisafe alerts are basically my personal health bodyguard. Don’t be like me and wait for a hospital visit to learn this lesson. Check. Then check again. You’ve got this!! 💪❤️
Ali Bradshaw
December 10, 2025Been a nurse for 18 years. Used Lexi-Interact daily in the hospital. The system’s great-but I’ve seen too many residents ignore red alerts because they’re ‘too busy.’ One guy prescribed clarithromycin with simvastatin to a 72-year-old. Muscle breakdown. ICU. All because the app said ‘severe interaction’ and he clicked ‘next’.
Tools don’t replace judgment. They amplify it. Use them like a seatbelt-not a self-driving car.
an mo
December 10, 2025Let’s be real: the entire drug interaction checker industry is a regulatory arbitrage play. Pharma companies fund the databases, the FDA turns a blind eye to false negatives, and clinicians are trained to treat alerts as noise. The 1.5 million ‘prevented events’? Half of them are inflated by system logs counting every pop-up as a ‘preventative action.’ Meanwhile, the real crisis-polypharmacy in the elderly-isn’t being solved. It’s being gamified.
Also, ‘free’ apps? They’re data farms. You think your supplement list is private? It’s being sold to supplement marketers who then target you with ‘better’ versions of what you’re already taking. Welcome to healthcare capitalism.
aditya dixit
December 12, 2025There’s a quiet wisdom in checking your meds-not because you fear them, but because you respect your body’s complexity. We live in an age of instant answers, but health isn’t a Google search. It’s a conversation-with your pharmacist, your history, your symptoms, your sleep, your stress.
A tool is just a mirror. The real work is looking into it honestly. And sometimes, the most powerful interaction checker is silence-the quiet moment before you swallow that pill, asking yourself: ‘Do I really need this? And what’s it doing to me?’
Not every answer needs an app.
Jimmy Jude
December 13, 2025Wow. A whole 1200-word essay on how to use an app that could’ve been summarized in two sentences: ‘Type in your meds. Read the red ones. Call your pharmacist.’
But no-let’s make it a TED Talk. Let’s turn a basic safety step into a cult of digital dependency. Next they’ll sell us a subscription to ‘Drug Interaction Pro’ with AI-powered emotional support alerts when you’re ‘too scared’ to take your blood pressure pill.
Meanwhile, in 2024, people still don’t know what ‘generic’ means. We’re not fixing the system. We’re just putting glitter on the dumpster fire.
Juliet Morgan
December 15, 2025OMG I JUST REALIZED I’VE BEEN TAKING MELATONIN WITH MY ANTI-DEPRESANT AND DIDN’T EVEN KNOW IT COULD CAUSE SEROTONIN SYNDROME 😱 THANKS FOR THIS POST!! I JUST CALLED MY PHARMACY AND THEY SAID I SHOULD STOP IT TILL I TALK TO MY DOCTOR. SO GLAD I READ THIS BEFORE SOMETHING BAD HAPPENED.
Y’all gotta check your stuff. Even if it’s just a gummy. 💛
William Chin
December 15, 2025It is imperative to underscore the critical necessity of verifying the authenticity and regulatory compliance of the digital platforms utilized for pharmacological interaction assessment. In the absence of FDA-validated data integrity protocols, the deployment of unlicensed consumer-facing applications constitutes a violation of the standard of care as defined by the American Medical Association’s 2022 guidelines on digital therapeutics.
Furthermore, the reliance upon algorithmic outputs devoid of clinician oversight introduces a material risk of liability exposure under the Health Insurance Portability and Accountability Act. I strongly recommend that all users procure only those tools certified under the ANSI/HL7 2023 Interoperability Standard.
Ada Maklagina
December 17, 2025app works but sometimes it says ‘possible interaction’ for stuff like vitamin C and blood pressure meds and I’m like… it’s just orange juice? I ignore the yellows. Red? Yeah I call my doc. Green? I’m good. Simple.
Also grapefruit juice is a sneaky one. I learned that the hard way.
Norene Fulwiler
December 18, 2025William Chin, you’re not wrong about standards-but most people don’t have access to HL7-certified systems. My mom uses Medisafe because it’s free, on her phone, and she can show it to her pharmacist. That’s not ‘violating care’-that’s democratizing safety. You want everyone to use Lexi-Interact? Fine. But first, make it free and teach grandma how to use it. Until then, apps like this save lives. Even if they’re imperfect.