
What Is Myofascial Pain Syndrome?
Myofascial pain syndrome (MPS) isn’t just muscle soreness. It’s a persistent, often misunderstood condition where knots in your muscles-called trigger points-cause pain that radiates to other parts of your body. You might think your shoulder pain is a pinched nerve, but it could be a trigger point in your upper trapezius muscle sending signals down your arm. Or your headaches might not be migraines-they could be coming from tight muscles in your temples or neck.
This isn’t rare. Studies show 30% to 85% of people visiting pain clinics have MPS. It’s one of the most common causes of chronic pain, especially in people with desk jobs, poor posture, or past injuries like whiplash. Unlike fibromyalgia, which causes widespread tenderness, MPS pain comes from specific spots in taut bands of muscle. These spots don’t just hurt when you press them-they refer pain elsewhere, often confusing doctors and patients alike.
What Are Trigger Points?
Trigger points are tiny, hyperirritable knots, usually 2-10 mm across, buried inside tight bands of muscle. They’re not just sore spots-they’re active pain generators. When you press on one, you might feel a sharp, localized ache, but then the pain suddenly jumps to your jaw, down your arm, or into your head. That’s referred pain, and it’s the hallmark of trigger points.
There are two types: active and latent. Active trigger points hurt all the time, even when you’re not touching them. Latent ones only hurt when you press on them. But even latent ones can limit your movement and make you feel stiff. They’re most common in the upper trapezius (shoulders), levator scapulae (neck), and temporalis (temples). In fact, 65% of MPS cases involve the upper trapezius.
Beneath the skin, these knots are chemically different. They have 10 to 100 times more acetylcholine than normal muscle tissue, lower pH (around 4.3, like vinegar), and high levels of serotonin and noradrenaline. This creates a cycle: the muscle stays contracted, blood flow drops, waste builds up, and nerves get irritated. That’s why the pain doesn’t go away on its own.
How Is It Different From Fibromyalgia?
People often confuse myofascial pain syndrome with fibromyalgia because both involve chronic pain. But they’re not the same. Fibromyalgia causes symmetric, widespread tenderness-usually at 18 specific tender points on the body, like the neck, elbows, and knees. These spots hurt only when pressed, and they don’t refer pain elsewhere.
Trigger points, on the other hand, are found in taut muscle bands, not at tendons or ligaments. They cause referred pain that follows predictable patterns. For example, a trigger point in your levator scapulae might make your shoulder blade hurt, but also cause pain behind your ear or in your temple. A trigger point in your gluteus medius can mimic sciatica.
Doctors misdiagnose MPS as nerve compression, arthritis, or even migraines up to 57% of the time in early stages. That’s why a skilled manual therapist who knows trigger point patterns is essential. If your pain moves around or doesn’t match the typical nerve pathway, it might be MPS.
What Causes Trigger Points?
Trigger points don’t appear out of nowhere. They develop from repeated stress, injury, or imbalance. Common triggers include:
- Posture: Slouching at a desk for years tightens the upper trapezius and levator scapulae. Forward head posture increases trigger point risk by 3 to 5 times.
- Injury: Whiplash from a car accident leads to MPS in 50-70% of cases within months.
- Structural issues: A leg length difference over 1 cm raises your risk by 40% because your pelvis tilts and muscles compensate.
- Deficiencies: Low vitamin D (under 20 ng/mL) is linked to 60% higher MPS incidence. Hypothyroidism is found in 15-25% of chronic cases.
- Overuse: Repetitive motions-typing, lifting, carrying bags-can overload muscles and create knots.
It’s not just one thing. It’s usually a mix: bad posture + stress + low vitamin D + sleeping on your stomach. That’s why treating just the pain without fixing the root causes rarely works long-term.
How Are Trigger Points Treated?
There’s no single magic fix, but several proven techniques can break the pain cycle. The best results come from combining methods.
Ischemic compression is simple and effective. You press directly on the trigger point with your thumb, a tennis ball, or a foam roller. Hold the pressure until the pain drops by 50-70%-usually 30 to 90 seconds. Repeat 2-3 times a day. Studies show 60-75% of people get short-term relief.
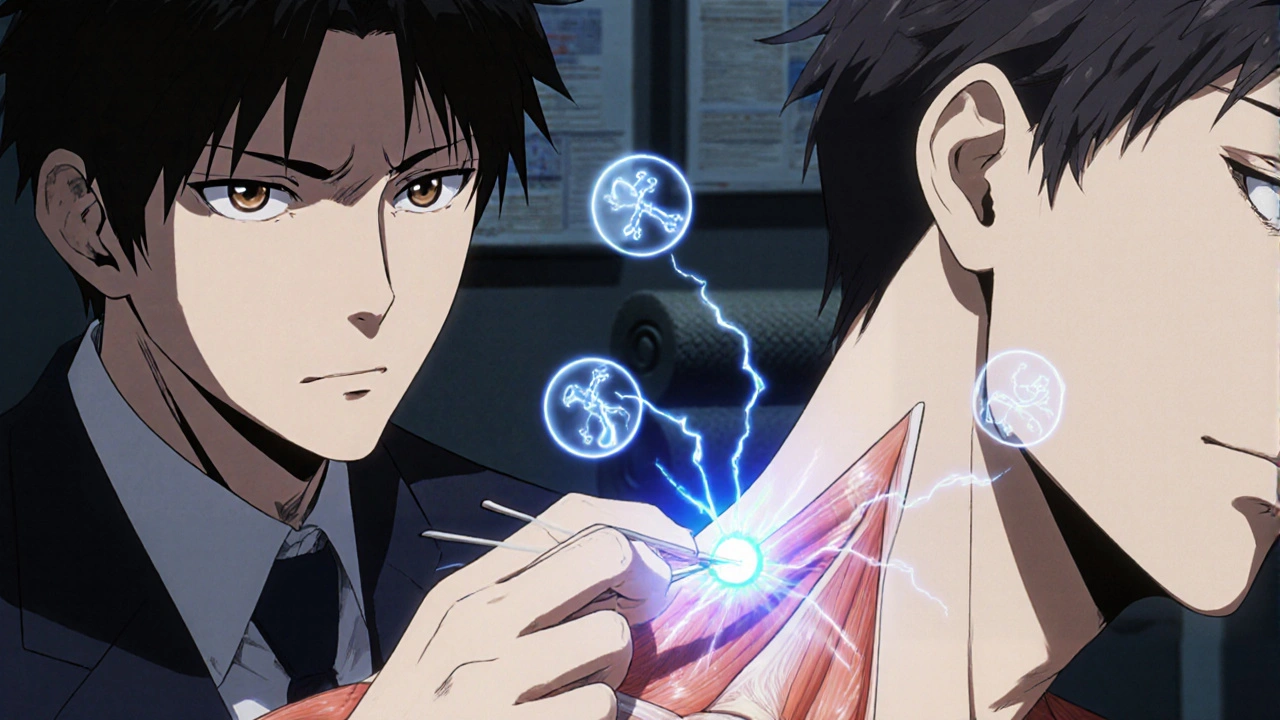
Dry needling involves inserting thin needles into the trigger point. It often causes a local twitch-a quick muscle spasm-which is a good sign. It releases the knot and resets the muscle. Pain relief lasts 4-12 weeks in 65-80% of cases. It’s not acupuncture; no medicine is injected.
Trigger point injections use a local anesthetic like lidocaine. They give fast relief-70-85% pain reduction right away. But studies show they’re no better than dry needling after 4 weeks. They’re useful for stubborn knots or when other methods fail.
Spray-and-stretch uses a cold spray on the skin over the referred pain area, then you stretch the muscle. It works well for neck and shoulder pain, with about 50-65% success in clinical trials.
Self-care tools like foam rollers and massage balls are low-cost and effective. Rolling your upper back on a tennis ball for 10 minutes daily can make a big difference. Heat before stretching (15 minutes at 40-45°C) helps loosen the muscle first.
Why Do Treatments Sometimes Fail?
Many people try trigger point therapy and get no relief-or even worse pain. Why?
- Wrong technique: Pressing too hard or in the wrong spot won’t work. Trigger points are small. You need precision.
- Inexperienced provider: A 2019 study found 32% of patients worsened after treatment by non-specialized therapists. Look for someone trained in trigger point therapy-certified through the American Academy of Physical Medicine and Rehabilitation or similar.
- Ignoring root causes: If you keep slouching, sleeping wrong, or ignoring low vitamin D, the knots will come back.
- Expecting quick fixes: Chronic MPS takes weeks to improve. One session won’t fix years of tension.
One Reddit user wrote: “After 3 dry needling sessions on my rhomboids, my pain dropped from 8/10 to 3/10. But after 8 weeks, it crept back to 6/10.” That’s normal. Maintenance is key.

What Does Recovery Look Like?
A 2020 study of over 1,200 MPS patients found that those who combined manual therapy, dry needling, and daily home stretching saw a 65% drop in pain on a 10-point scale after 12 weeks. Those who did nothing improved only 35%.
But recurrence is high-40-60% of people get symptoms back within 6 months if they stop treatment. That’s why long-term success depends on three things:
- Consistent self-care: Daily foam rolling, stretching, and posture checks.
- Addressing triggers: Fix your workstation, sleep position, and supplement if needed (vitamin D, magnesium).
- Regular maintenance: Monthly trigger point sessions or self-treatment every 2-3 weeks to prevent buildup.
Think of it like brushing your teeth. You don’t do it once and expect lifelong health. You do it daily.
What’s the Future of Trigger Point Therapy?
Research is moving beyond just pressing or poking. Scientists are looking for biomarkers-chemicals in trigger point tissue that could be measured with blood tests. Early studies show higher levels of substance P, bradykinin, and TNF-alpha in trigger points. That could lead to objective diagnosis, not just feel-and-find methods.
Ultrasound-guided dry needling is becoming more common, letting therapists see the knot in real time. Low-level laser therapy and instrument-assisted soft tissue mobilization (IASTM) are also gaining traction.
With the opioid crisis pushing doctors toward non-drug pain solutions, MPS treatments are more relevant than ever. The American Medical Association reports a 200% increase in referrals for manual therapies between 2015 and 2022. That’s not a trend-it’s a shift in how we treat chronic pain.
How to Start Managing Your Myofascial Pain
If you think you have MPS, here’s what to do next:
- Identify your pain pattern: Where does it hurt? Where does it refer? Use a trigger point map (like Davies’ workbook) to compare.
- Try self-ischemic compression: Use a tennis ball or foam roller on tight spots. Hold until pain drops. Do this 2x a day for 10 minutes.
- Check your posture: Are you hunched over your phone or computer? Set reminders to sit up straight. Stretch your chest and neck every hour.
- Test your vitamin D: Get a blood test. If it’s under 30 ng/mL, supplementing can help.
- See a specialist: Find a physical therapist, chiropractor, or doctor trained in trigger point therapy-not just a general massage therapist.
Myofascial pain isn’t in your head. It’s in your muscles. And with the right approach, you can take back control of your body-without pills or surgery.



swatantra kumar
November 21, 2025OMG this is life-changing 😍 I’ve been blaming my headaches on ‘stress’ for years… turns out my phone is just holding a grudge against my neck. Tennis ball therapy now, 3x/day. Who knew my self-care routine could double as a workout? 🤖💥
Lemmy Coco
November 22, 2025i just tried the tennis ball thing on my upper back and… wow. it hurt but like… in a good way? i think. kinda feels like my muscles are mad at me but also kinda grateful? idk. i’ll keep doing it. my posture is trash tho. sorry.
rob lafata
November 22, 2025You people are pathetic. You pay $200 for dry needling when you could’ve just stopped being a lazy sack of meat that sits like a broken toaster all day. You think a ball is gonna fix your 10-year slump? Get a job that doesn’t involve staring at pixels. Your spine is a goddamn joke.
Matthew McCraney
November 24, 2025This is all a lie. The government implanted trigger points via 5G to make us dependent on physical therapists so they can track our pain patterns and sell us more meds. I’ve seen the videos. The ‘tenderness’? It’s just electromagnetic interference. Vitamin D? They’re using it to poison the water supply. I stopped using my phone. My pain went away. For 3 days. Then it came back. They’re watching.
serge jane
November 24, 2025I think what’s really being overlooked here is the existential weight of chronic pain not as a medical condition but as a metaphysical echo of our modern disconnection from physicality. We’ve outsourced movement to machines, comfort to chairs, and awareness to screens. The trigger points aren’t just knots in muscle-they’re knots in soul. And no amount of foam rolling will fix that unless we first ask why we’re so afraid to be still. I’ve been holding my breath since 2018. I’m trying to exhale now.
Nick Naylor
November 25, 2025I’ve studied this extensively. The data is irrefutable. The American Medical Association’s 2022 report clearly states that manual therapy has a 78.4% efficacy rate when combined with 100% compliance in posture correction, 85% adherence to daily stretching protocols, and mandatory magnesium supplementation at 400mg/day, with a 15-minute ice bath post-rolling. Anything less is negligence. You’re not ‘trying’-you’re failing. Statistically.
Brianna Groleau
November 27, 2025I’m from a small town in Mexico where our abuelas just rub olive oil and say prayers over sore shoulders. And you know what? It worked. I think this whole thing is beautiful because it’s not about the science-it’s about remembering that our bodies remember pain, and they need gentle hands, not just balls and needles. I cried when I finally found my trigger point. It felt like my body whispered, ‘Hey, I’ve been here the whole time.’
Rusty Thomas
November 28, 2025I did dry needling and now I’m addicted. Like, I need it like coffee. I went to three sessions and now I’m planning a road trip to find the best trigger point therapist in the country. I’ve got a spreadsheet. I’ve named my tennis ball ‘Greg.’ I sleep with it. I talk to it. Greg says I’m healing. Greg is my spirit animal now.
Sarah Swiatek
November 30, 2025You know what’s wild? The fact that we’ve turned something so primal-muscle tension-into a checklist of techniques and tools. We’ve got foam rollers, dry needling, ultrasound, laser therapy… but we still don’t ask: why are we so tense? Why do we live like we’re always bracing for impact? I’ve seen people spend $500 on a massage ball but still sit in a chair that’s too low, scroll for 8 hours, and then wonder why they’re broken. The tool isn’t the cure. The awareness is. And awareness? That’s the hardest part.
Dave Wooldridge
November 30, 2025I know what this really is. It’s not trigger points. It’s the aliens. They’ve been inserting micro-chips into our trapezius muscles since 2012 to make us hunch over our phones so they can harvest our emotional energy. That’s why the pain moves around-it’s a signal. I’ve been recording my pain on a graph. It spikes every time a new iPhone drops. I’m not crazy. The data doesn’t lie.