Getting the right dose of medication isn’t just about following the label. For many people, especially those over 65, with kidney issues, or who are underweight or obese, the standard dose can be too much-or too little. Too high, and you risk poisoning your body. Too low, and the drug does nothing. The truth is, medication dosing isn’t one-size-fits-all. It’s shaped by your age, your weight, and how well your kidneys are working. Ignore any one of these, and you’re playing Russian roulette with your health.
Why Your Kidneys Matter More Than You Think
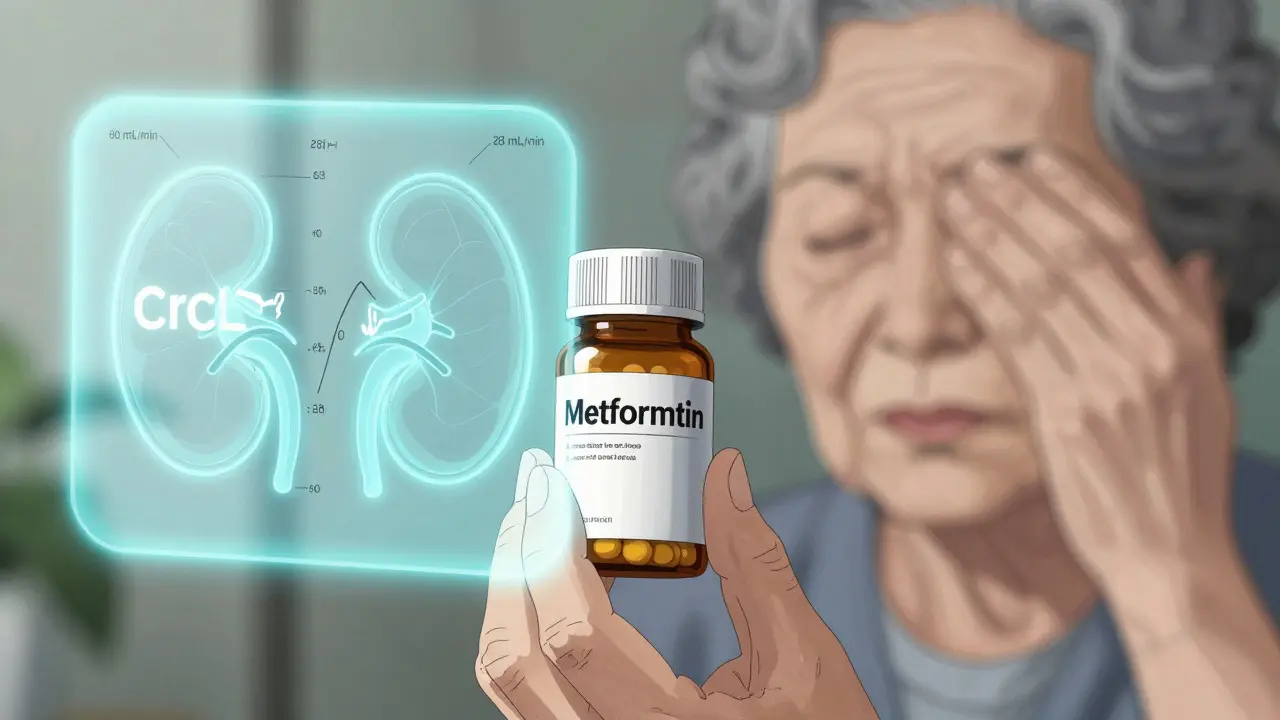
Your kidneys don’t just filter waste. They’re the main exit ramp for most drugs. About 40% to 60% of commonly prescribed medications-antibiotics, blood pressure pills, diabetes drugs, pain relievers-leave your body through your kidneys. If your kidneys are slowing down, those drugs build up. That’s how you end up with dizziness, confusion, or even kidney failure from a pill meant to help you. The standard way doctors check kidney function is with a blood test for creatinine. But creatinine alone doesn’t tell the full story. That’s why we use formulas. The most common one used in drug labels is the Cockcroft-Gault equation. It takes your age, weight, sex, and creatinine level to estimate how fast your kidneys filter blood-called creatinine clearance (CrCl). For example, a 78-year-old woman weighing 52 kg with a creatinine of 1.4 mg/dL might have a CrCl of just 28 mL/min. That’s Stage 4 kidney disease. Her metformin dose should drop from 1,000 mg twice daily to 500 mg once daily. But if her doctor just saw her creatinine and assumed she was fine? She could end up in the hospital. The CKD-EPI equation, developed in 2009, is now used to stage kidney disease. It’s more accurate for people with normal or near-normal kidney function. But here’s the catch: drug dosing guidelines were mostly built using Cockcroft-Gault numbers. So even if your eGFR (from CKD-EPI) says you’re Stage 2, your actual drug clearance might be closer to Stage 3. That’s why pharmacists still use CrCl for dosing, not eGFR. It’s confusing, and it’s dangerous if you don’t know the difference.Weight Isn’t Just About Size-It’s About How Drugs Move in Your Body
A 120-pound person and a 280-pound person aren’t just different in size. Their bodies handle drugs differently. Drugs need space to spread out. In someone with a lot of body fat, many medications get trapped in fat tissue and never reach the bloodstream where they’re supposed to work. In someone very thin, the same drug can flood the system. For obese patients (BMI over 30), using actual body weight leads to massive overdosing. That’s why we use adjusted ideal body weight. Here’s how it works: First, calculate your ideal body weight. For men, it’s 50 kg plus 2.3 kg for every inch over 5 feet. For women, 45.5 kg plus 2.3 kg per inch. Then, take 40% of the difference between your actual weight and your ideal weight, and add it to your ideal weight. That’s your adjusted weight for dosing. Take vancomycin, an antibiotic used for serious infections. If a 110 kg man with a BMI of 35 gets dosed by actual weight, he might get 2,500 mg. But his adjusted weight is only 82 kg. Giving him the full dose means his blood levels spike dangerously high. He could develop hearing loss or kidney damage. But if you use his adjusted weight? He gets 1,800 mg-enough to kill the infection without harming him. On the flip side, an elderly woman weighing 45 kg with no muscle mass might need half the dose of a 70 kg adult. Her kidneys may be slow, her body small, and her liver less able to process drugs. Standard doses can be toxic.
Aging Changes How Your Body Handles Medicine
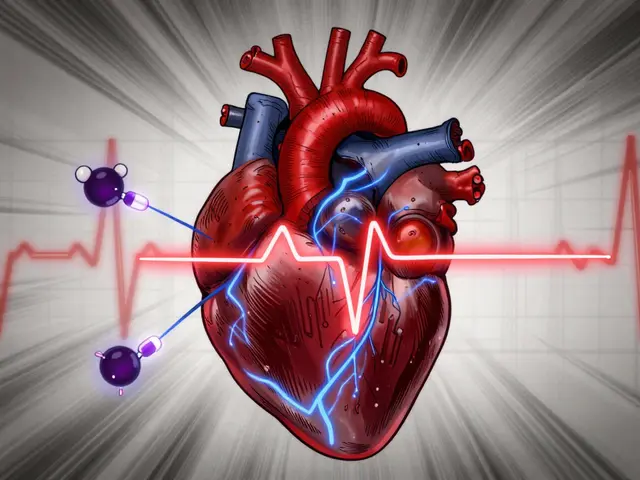
As you get older, your body changes in ways no pill can reverse. Kidney function drops naturally-about 1% per year after age 40. Liver enzymes slow down. Body water decreases. Fat increases. All of this means drugs stick around longer, build up more easily, and hit harder. Older adults take an average of four to five medications daily. That’s a recipe for interaction and overdose. A 2020 study found that 30% of adverse drug events in people over 65 were because of kidney-related dosing errors. One common example: digoxin, used for heart rhythm. It’s cleared almost entirely by the kidneys. In a 70-year-old with mild kidney decline, the dose should be cut by 30-50%. But many doctors still prescribe the standard 0.125 mg daily. The result? Nausea, confusion, irregular heartbeat-symptoms often mistaken for dementia. Even something as simple as ibuprofen can be risky. It’s not just a painkiller-it’s a kidney stress test. In someone over 70 with even mild kidney disease, daily use can cause acute kidney injury. Yet, it’s still sold over the counter as if age doesn’t matter.Real-World Mistakes and How to Avoid Them
Pharmacists see it every day. A patient on metformin for 10 years with an eGFR of 28-still taking 1,000 mg twice daily. A diabetic on insulin with declining kidney function, not having their dose reduced, and ending up with dangerous low blood sugar. A patient on cefazolin for a skin infection, given a dose based on eGFR instead of CrCl, and not responding to treatment. A 2022 survey found that 68% of pharmacists encountered incorrect renal dosing at least once a week. Antibiotics, heart meds, and diabetes drugs were the top offenders. Why? Because dosing guidelines aren’t consistent. One hospital formulary says give 50% of the normal dose if CrCl is under 30. Another says 25%. A third says don’t use it at all. It’s chaos. The fix? Use the right tool. If you’re a clinician, always calculate CrCl using Cockcroft-Gault for drug dosing. For obese patients, use adjusted body weight. For elderly patients, assume kidney function is lower than it looks-even if creatinine seems normal. Always check the drug label. The FDA requires all new drugs to include renal dosing info based on CrCl categories: normal (>60), mild (60-89), moderate (30-59), severe (15-29), and end-stage (<15). Electronic health records now have built-in alerts. One hospital cut dosing errors by 53% in 18 months by auto-calculating CrCl and flagging unsafe doses. But alerts aren’t perfect. They can be ignored, overridden, or based on wrong data. Always double-check. Ask: Is this dose based on CrCl? Did we use adjusted weight? Is this drug even safe for kidney patients?
What You Can Do as a Patient
You don’t need to be a doctor to protect yourself. Here’s what works:- Ask your doctor or pharmacist: "Is my dose based on my kidney function?"
- Know your creatinine and eGFR numbers. Ask for them after your blood test.
- If you’re over 65, overweight, or underweight, ask: "Should my dose be adjusted?"
- Keep a list of all your meds-including over-the-counter ones. Bring it to every appointment.
- If you feel dizzy, confused, nauseous, or unusually tired after starting a new drug, call your provider. Don’t wait.
The Future: Smarter Dosing, Not Just More Rules
The system is still broken. But change is coming. The FDA is pushing for real-time dosing tools. AI algorithms are being tested to combine kidney function, genetics, age, and weight into one personalized dose. Wearable sensors that estimate kidney filtration in real time are in early trials. By 2030, your smartwatch might tell your doctor: "Your patient’s kidney filter is dropping-adjust their dose now." For now, though, the best tool is still knowledge. Your body isn’t a textbook. Your dose shouldn’t be either. Age, weight, and kidney function aren’t just numbers on a chart-they’re the keys to safe, effective medicine. If you’re not being asked about them, ask yourself: Am I getting the right dose-or just the standard one?How do I know if my medication dose needs to be adjusted for kidney function?
If you’re over 65, have diabetes, high blood pressure, or have been told you have kidney disease, your dose likely needs adjustment. Ask your doctor for your creatinine level and estimated creatinine clearance (CrCl). If your CrCl is below 60 mL/min, many drugs require a lower dose or less frequent dosing. Check the drug’s prescribing information or ask your pharmacist to review it with you.
Why do some doctors use eGFR and others use CrCl for dosing?
eGFR (from the CKD-EPI equation) is used to stage kidney disease and track long-term health. CrCl (from the Cockcroft-Gault equation) is used for drug dosing because most medication guidelines were developed using CrCl. The two numbers are similar but not the same. For dosing, CrCl is still the gold standard-even if your doctor uses eGFR for diagnosis.
Should I use my actual weight or ideal weight for calculating my dose?
If you’re obese (BMI over 30), use adjusted ideal body weight-not your actual weight. Using actual weight can lead to dangerous overdosing, especially with antibiotics like vancomycin or chemotherapy drugs. If you’re underweight (BMI under 18.5), your dose may need to be reduced because drugs can reach toxic levels faster. Always confirm with your pharmacist or doctor.
Can I just take half the dose if I’m older or have kidney problems?
No. Not all drugs are reduced the same way. Some need a smaller dose, others need to be given less often. Some shouldn’t be used at all. For example, metformin must be stopped if CrCl drops below 30, but insulin doses may need to be lowered, not stopped. Never guess. Always check the specific guidelines for your medication.
Are over-the-counter painkillers safe if I have kidney disease?
Not always. NSAIDs like ibuprofen and naproxen can reduce blood flow to your kidneys and cause sudden kidney injury, especially in older adults or those with existing kidney disease. Acetaminophen (Tylenol) is usually safer for short-term use, but even that can be risky if taken in high doses or with alcohol. Always talk to your doctor before taking any OTC pain reliever if you have kidney issues.



Lyle Whyatt
February 9, 2026Man, this post hit me right in the feels. I’ve been on metformin for 12 years, and my last bloodwork showed CrCl at 29. My PCP just said, 'Keep taking it, you’re fine.' I went to a pharmacist instead-she nearly had a heart attack. She switched me to 500 mg once daily and made me sign a waiver because she said, 'If you keep taking double that, you’re gonna end up on dialysis before 70.' I didn’t even know kidney function was tracked like this. Now I check my numbers every 3 months. Thanks for the wake-up call.
Also, side note: I used to think 'eGFR' and 'CrCl' were the same. Turns out they’re like comparing apples to rocket fuel. Pharmacists are the real MVPs here.
Brandon Osborne
February 10, 2026Ugh. Another one of these 'medical complexity' rants. People just don’t take responsibility anymore. If you’re over 65 and still taking ibuprofen daily, you’re an idiot. If you’re obese and think you deserve the same dose as a 150-pound person, you’re asking for trouble. This isn’t rocket science-it’s basic biology. Stop blaming doctors. Start reading the damn label. And if you can’t understand it? Go to a pharmacy. Not every drug company is out to kill you.
Also, why do we let people self-diagnose with 'kidney issues'? You get one blood test and suddenly you’re a nephrologist? Ridiculous.
MANI V
February 12, 2026It’s pathetic how Western medicine keeps pretending it’s precise when it’s just a series of educated guesses wrapped in jargon. I’ve seen 80-year-olds in India on full-dose antibiotics because their family insisted-no labs, no creatinine, just 'he’s sick, give him the pill.' And guess what? Most of them survive. Because their bodies are lean, their diets are clean, and they don’t have 12 meds floating around their system.
Here’s the truth: Western medicine overmedicates because it’s profitable. Dosing algorithms? They’re built for insurance billing, not for human biology. I’ve worked in clinics in Kerala-we use weight, age, and common sense. No equations. No eGFR. Just: 'Does this person look like they can handle this dose?' And guess what? Fewer ER visits.
Stop trusting formulas. Trust experience. Trust culture. Trust your grandmother’s intuition.
Ken Cooper
February 12, 2026Okay so I’m a nurse’s aide and I’ve seen this first hand. My grandma (81, 47kg, creatinine 1.3) was on 500mg metformin twice a day. She started getting super dizzy, confused, falling a lot. We thought it was dementia. Turned out her CrCl was 24. We switched her to 500mg once a day. Within a week, she was back to knitting and yelling at the TV. No more falls.
Also-obese patients? My cousin is 310 lbs, BMI 42. Took vancomycin for a staph infection. They dosed him on actual weight. He got 3g. He nearly went deaf. They had to pull him off it. Then they recalculated with adjusted weight (he’s 89kg adjusted) and gave him 1.6g. Perfect. No side effects. So yeah, this isn’t theory. It’s life or death.
And honestly? I think every ER should have a CrCl calculator on every computer. Like, right next to the EKG. It’s that important.
Sam Dickison
February 14, 2026Just chiming in as a clinical pharmacist. The Cockcroft-Gault vs. CKD-EPI thing is a mess. Most hospitals still use CG for dosing because it’s validated in trials. CKD-EPI is great for staging, but not for predicting drug clearance. You can’t just swap them. I’ve seen patients on vancomycin with eGFR 45 but CrCl 22. Gave them standard dose? Toxic. Adjusted? Perfect.
Also-adjusted body weight formula? Yeah, it’s clunky, but it works. For obese patients, we use: IBW + 0.4*(actual - IBW). That’s the sweet spot. Don’t use actual weight. Don’t use ideal. Use adjusted. And yes, this applies to aminoglycosides, beta-lactams, even antivirals.
One thing I wish doctors did: always check the drug’s prescribing info. The FDA requires renal dosing tables. If it’s not there? Proceed with extreme caution. And if you’re unsure? Consult a pharmacist. We’re not just pill counters-we’re safety nets.
Joseph Charles Colin
February 15, 2026As a nephrology fellow, I can say this: the biggest gap in clinical practice is not knowing which formula to use when. Cockcroft-Gault is outdated? Maybe. But it’s still the gold standard for dosing because it’s the one used in the original trials. CKD-EPI is better for predicting mortality, not drug clearance.
Also-obesity dosing. Most guidelines are based on the 1980s data from the NIH. The formula we use? It’s literally from a 1979 paper. We’ve updated everything else-why not this? I’ve pushed for AI-based dosing models that incorporate body composition, not just weight. But bureaucracy moves slower than kidney filtration in a diabetic.
And yes, ibuprofen in elderly? It’s a silent killer. We screen every patient over 65 for NSAID use. One 75-year-old woman came in with AKI because she’d been taking 800mg ibuprofen daily for 'arthritis.' She didn’t even know it was an NSAID. She thought it was 'just a pain pill.'
Bottom line: if you’re over 65, on more than 3 meds, or have any kidney risk? Get a med review. Ask for CrCl. Ask for adjusted weight. Don’t assume anything. And if your doctor says 'it’s fine'-get a second opinion.
John Sonnenberg
February 16, 2026THIS. IS. A. DISASTER.
Every single day. Every. Single. Day. I’ve seen patients on 1000mg metformin with CrCl 25. I’ve seen 80-year-olds on full-dose cefazolin. I’ve seen obese men getting 3g vancomycin like they’re NFL linemen. And guess what? The system doesn’t care. It’s all automated. EHRs don’t even flag it. Pharmacists are screaming into the void.
And then you get the 'but the label says 500mg bid' crowd. The label is based on a 70kg 40-year-old with perfect kidneys. Your grandma is not that person.
There’s a reason we have pharmacy committees. There’s a reason we have clinical guidelines. And there’s a reason I’m about to lose my mind.
Someone needs to make a mandatory CrCl calculator app for every prescriber. And it needs to be linked to the EHR. And it needs to block the order if it’s wrong. That’s not innovation. That’s basic safety.
Joshua Smith
February 17, 2026Hey, I’m a 72-year-old retired engineer. I’ve been on blood pressure meds for 20 years. My doctor always used eGFR. Last year I asked my pharmacist to check CrCl. It was 38. She immediately cut my lisinopril dose. I didn’t even know that was a thing.
Now I check my creatinine every 6 months. I’ve started asking every doctor: 'What’s my CrCl?' They all look at me like I’m crazy. But I’m not. I’m just paying attention.
Also-my neighbor’s 80-year-old wife was on metformin and got hospitalized for lactic acidosis. Turned out her CrCl was 21. She’d been on the same dose for 8 years. She’s fine now, but… why didn’t anyone catch it?
Just saying: if you’re older, ask. Don’t assume. And if your doctor doesn’t know CrCl from eGFR? Find a new one.
Jessica Klaar
February 19, 2026I’m from rural Iowa, and I’ve seen so many older folks just… keep taking pills because 'that’s what the doctor said.' My aunt took her full dose of digoxin for years even after her kidneys slowed. She thought it was 'just a heart pill.' Then she started seeing halos around lights and couldn’t remember her grandson’s name. We thought it was Alzheimer’s. Turns out it was digoxin toxicity.
My mom, who’s 68, now carries a little card in her wallet: 'CrCl: 34. Metformin: 500mg once daily. Vancomycin: use adjusted weight.' She showed it to her new PCP last week. He said, 'I wish more patients did this.'
It’s not about being a medical expert. It’s about being your own advocate. A simple question-'What’s my kidney number?'-could save your life. And if you’re scared to ask? Bring someone with you. I did. And I’m so glad I did.