When your heart stops getting enough blood, it doesn’t scream. It whispers. And too many people ignore the whisper until it’s too late.
Every minute counts during a heart attack. Each passing minute kills about 1.5 million heart muscle cells. If you act fast, your chance of surviving jumps by up to 50%. But if you wait, or worse - if you think it’s just indigestion or stress - you’re playing Russian roulette with your life.
What a Heart Attack Really Feels Like
The classic image of a heart attack - a man clutching his chest, collapsing dramatically - is mostly Hollywood. Real heart attacks often start quietly. The most common sign is discomfort in the center of your chest. It’s not always sharp pain. It’s more like pressure, tightness, fullness, or a heavy weight sitting on your ribs. It lasts longer than a few minutes, or it comes and goes.
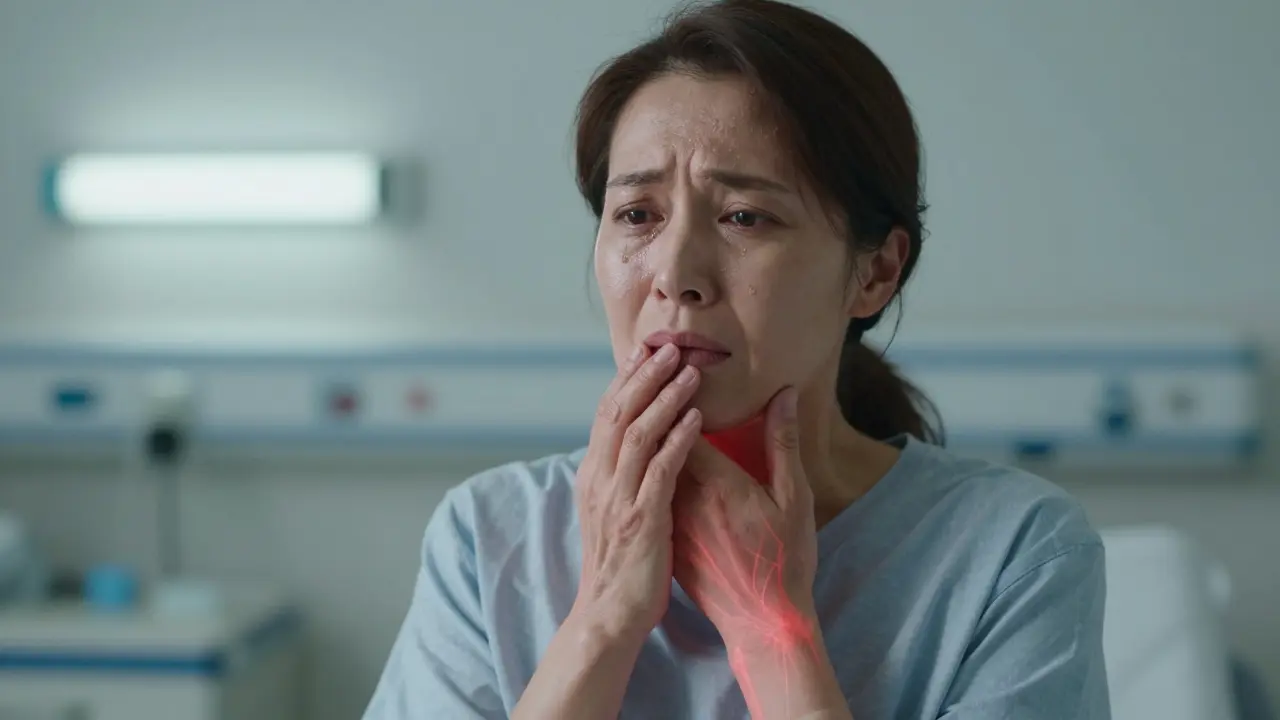
But here’s what most people don’t know: you don’t need chest pain to be having a heart attack. About 36% of women and 20% of men don’t feel chest discomfort at all. Instead, they feel pain in their arms, back, neck, jaw, or stomach. One woman I spoke to thought she had a bad toothache. It was her jaw. Another thought she was having a panic attack. It was her heart.
Gender Differences: Why Women Are at Higher Risk
Women’s heart attacks look different. Not because they’re weaker, but because their bodies respond differently. While 90% of men report chest pain during a heart attack, only 64% of women do. Women are far more likely to have shortness of breath, nausea, vomiting, back or jaw pain, and extreme fatigue. In fact, nearly half of women report unusual tiredness in the days or weeks before a heart attack - something doctors often dismiss as burnout or aging.
Women over 55 are twice as likely as men their age to experience what’s called ‘atypical’ symptoms. That means overwhelming anxiety, upset stomach, or even a sense of impending doom. One study found women are 58% more likely to have shortness of breath as their main symptom. And here’s the scary part: women are 50% more likely to be misdiagnosed in the ER. Their symptoms get written off as anxiety, acid reflux, or the flu. That delay kills.
Age and Silent Heart Attacks
Older adults - especially those over 75 - are more likely to have what’s called a ‘silent’ heart attack. No chest pain. No warning. Just sudden weakness, confusion, or trouble breathing. About 30% of heart attacks in people over 75 show no chest symptoms at all. That’s why family members need to be alert. If your elderly parent suddenly seems off, tired, or confused, don’t assume it’s just getting older. Call for help.
And it’s not just older people. Heart attacks in adults aged 25 to 44 have been rising by 2% every year since 2000. Younger people aren’t immune. Stress, poor diet, lack of movement, and undiagnosed high blood pressure are quietly increasing risk. You don’t have to be 60 to have a heart attack. You just have to be alive.

Other Warning Signs You Can’t Ignore
Here’s a quick list of symptoms that aren’t normal, no matter your age or gender:
- Breaking out in a cold sweat - not from heat, not from exercise. Just suddenly, for no reason.
- Feeling dizzy or lightheaded - like you might pass out.
- Heart racing or skipping beats - especially if it’s new and unexplained.
- Unexplained nausea or vomiting - not from food poisoning, not from the flu.
- Extreme fatigue - so tired you can’t get out of bed, even after sleeping.
- Swelling in the legs or ankles - if it’s new and sudden.
Some people report feeling like they’ve been hit by a truck. Others say they just felt ‘wrong’ - like something inside them didn’t feel right. Trust that feeling.
What to Do When You Suspect a Heart Attack
If you or someone else shows any of these signs, don’t wait. Don’t call your doctor. Don’t drive yourself to the hospital. Call emergency services right away.
Why? Because ambulances can start treatment on the way. They have EKG machines, oxygen, and medications that can save your heart before you even reach the ER. People who call 911 get to the hospital 25% faster than those who drive themselves.
While you wait for help:
- If you’re not allergic to aspirin and your doctor hasn’t told you not to, chew one 300mg tablet. It helps thin the blood and can reduce damage.
- Stay seated. Don’t lie down - it can make breathing harder.
- Don’t eat or drink anything.
- Keep calm. Panic makes your heart work harder.
And if you’re with someone who collapses, starts gasping, or becomes unresponsive - start CPR. Push hard and fast in the center of the chest. Don’t wait for permission. People who get CPR immediately are twice as likely to survive.
Why People Wait - and Why That’s Deadly
The average person waits three hours before calling 911. That’s three hours too long. Why? Fear. Embarrassment. Denial.
‘I don’t want to make a fuss.’
‘Maybe it’s just heartburn.’
‘I’m not old enough for this.’
These thoughts kill. A 2022 survey found that 33% of heart attack victims waited over two hours because they were afraid they were wrong. And here’s the truth: it’s better to be wrong and safe than right and dead.
Women are especially prone to this delay. They’re more likely to downplay symptoms, worry about being seen as dramatic, or assume they’re just ‘stressed.’ But heart attacks don’t care how strong you are. They don’t care if you’re a mom, a CEO, or a fitness trainer. They strike silently. And they strike fast.
What’s Changing in Heart Attack Care
Technology is helping. AI-powered tools can now detect heart attack patterns on an EKG 30 minutes before symptoms even start. These tools are being rolled out in hospitals across the U.S. and Australia. Wearable EKG devices - like those in smartwatches - are now used by 38% of U.S. adults. They can catch irregular heart rhythms that might lead to a heart attack.
Hospitals are also improving. Since 2021, U.S. hospitals have been required to follow standardized heart attack protocols. That means faster testing, faster treatment, and fewer mistakes. But none of that matters if you don’t call for help.
Community training programs - like the American Heart Association’s ‘Heart Attack 101’ - have cut response times by nearly 50 minutes. People who’ve been trained recognize symptoms faster. They act faster. They save lives.
What You Can Do Today
You don’t need to be a doctor to save a life. Here’s what you can do right now:
- Learn the symptoms - not just the chest pain ones. Know the ones women and older adults get.
- Talk to your family. Make sure your partner, kids, or elderly parents know what to look for.
- Know your risk factors: high blood pressure, high cholesterol, smoking, diabetes, obesity, family history.
- Get regular checkups. Even if you feel fine.
- Keep aspirin in your medicine cabinet - if your doctor says it’s okay.
- Learn CPR. It’s not hard. A 20-minute online video is all it takes.
Heart attacks don’t announce themselves with sirens. They creep in. But you can stop them - if you know what to look for, and if you act before it’s too late.




Cassie Widders
January 13, 2026My grandma ignored her jaw pain for days. Thought it was a tooth. Turned out it was a heart attack. She’s fine now, but barely made it. Don’t wait.
Craig Wright
January 13, 2026It is a matter of national responsibility. The British NHS has long underprioritized cardiac triage. This article is correct but lacks systemic critique. We must demand policy reform, not just personal vigilance.
Lelia Battle
January 15, 2026There’s something deeply human about how we deny our own fragility. We treat the body like a machine that should never break down - but it’s alive, not engineered. The silence of the heart isn’t weakness. It’s biology whispering truths we’ve trained ourselves not to hear.
Rinky Tandon
January 15, 2026Let me be clear - this is a catastrophic failure of modern medicine’s patriarchal bias. Women’s symptoms are pathologized as psychosomatic. Endocrine dysregulation, autonomic nervous system divergence - these aren’t ‘atypical,’ they’re biologically normative in female physiology. The medical establishment is still stuck in 1950s textbooks. And no, aspirin isn’t a panacea if you’re on anticoagulants - don’t self-prescribe without lipid panel and troponin context.
Ben Kono
January 16, 2026My buddy thought he was just tired after work then passed out in the shower. No chest pain. Just felt off. 911 saved him. Don't be dumb. Call now.
Konika Choudhury
January 17, 2026Why do Americans always act like they invented heart attacks We have been treating this for centuries in India with Ayurveda and yoga. You people just wait until you collapse then blame the system
Darryl Perry
January 18, 2026Three hours is unacceptable. The data is clear. Delay equals death. Stop rationalizing. Call 911. Period.
Windie Wilson
January 19, 2026Oh so now my ‘stress’ is a heart attack? I guess my 3 a.m. crying spells over deadlines are just myocardial ischemia in disguise. Thanks for making anxiety feel like a death sentence, Dr. Wellness Blog.
Daniel Pate
January 20, 2026If we accept that heart attacks often present without chest pain, then the diagnostic framework must shift from symptom-based to pattern-recognition models. The absence of classical signs doesn’t imply absence of pathology - it implies a failure of our classification systems. We need to train clinicians to treat the patient, not the textbook.
Amanda Eichstaedt
January 21, 2026I taught my 72-year-old mom CPR last weekend. We watched a 20-minute video on YouTube, practiced on a mannequin from Amazon, and now she knows to call 911 even if she thinks she’s being dramatic. She said, ‘I’d rather look silly than be dead.’ Best thing she’s ever said.