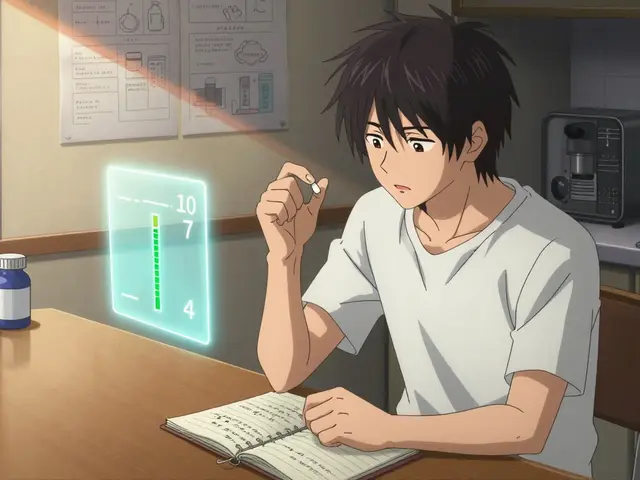
Medication Dry Mouth Risk Checker
Find out the dry mouth risk of your medications and discover lower-risk alternatives. Enter your medication name to see detailed risk information.
Lower-Risk Alternatives
Tip: Always consult your doctor before changing any medication. This tool provides information only.
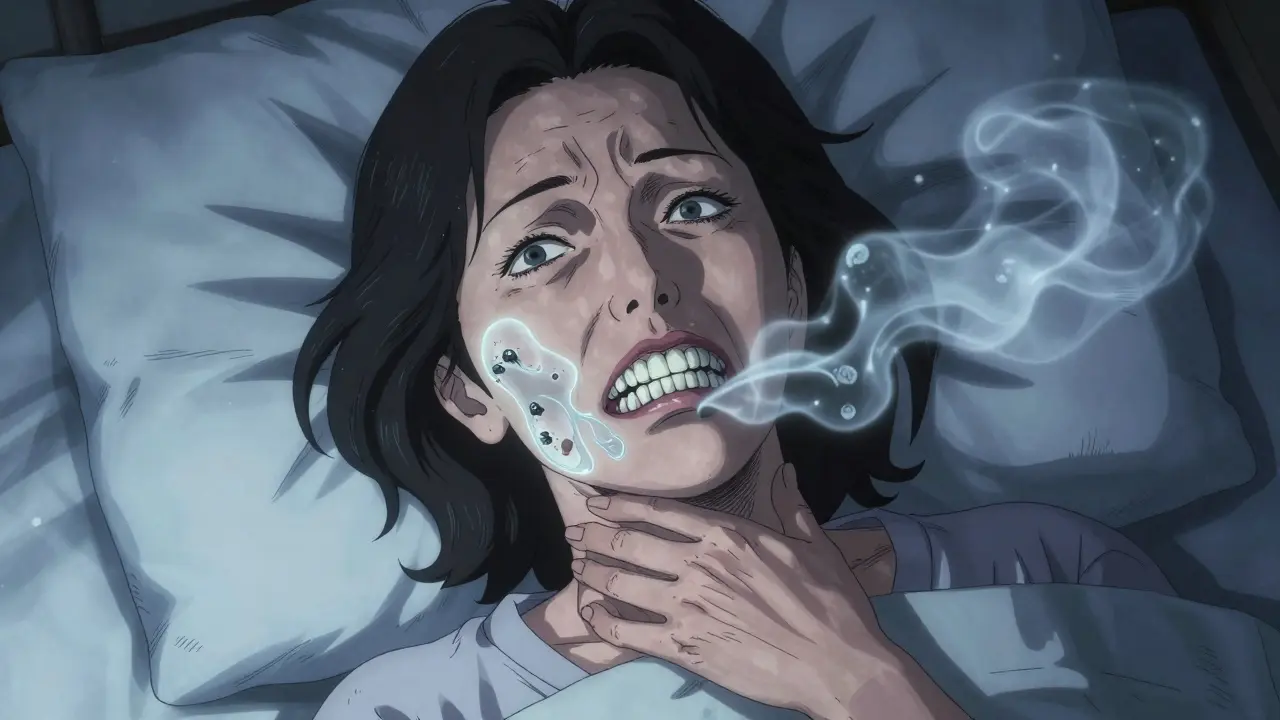
More than 11 million Americans experience dry mouth because of their medications. If you’ve ever woken up with a cottony throat, struggled to swallow your breakfast, or found yourself constantly reaching for water, you’re not alone. Dry mouth isn’t just uncomfortable-it’s a silent threat to your teeth, gums, and overall health. And the worst part? Most doctors don’t talk about it.
Why Your Medication Is Drying Out Your Mouth
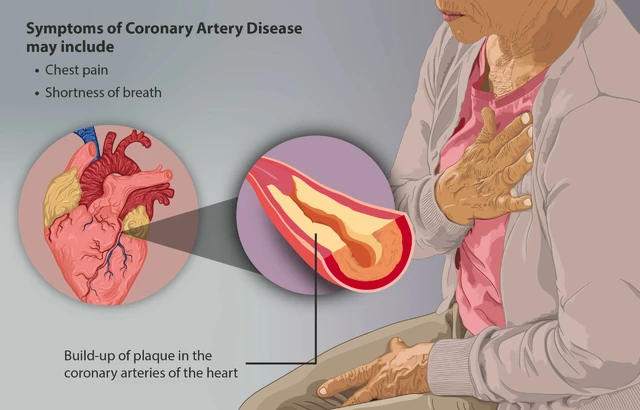
Your saliva doesn’t just help you chew and swallow. It’s your mouth’s natural defense system. It washes away food particles, neutralizes acids, and keeps bacteria in check. When saliva production drops, your mouth becomes a breeding ground for decay, infections, and bad breath. The problem starts with how your body makes saliva. It’s controlled by nerves that respond to a chemical called acetylcholine. Many medications block this chemical-specifically at the M3 muscarinic receptors in your salivary glands. This is called an anticholinergic effect. About 68% of drugs that cause dry mouth work this way. You don’t need to be on a crazy cocktail of pills to get this side effect. Even one medication can do it. Common offenders include:- Antihistamines like diphenhydramine (Benadryl): 58% of users report dry mouth
- Tricyclic antidepressants like amitriptyline: 63% of patients experience it
- Overactive bladder drugs like oxybutynin: over 70% of users get dry mouth
- High blood pressure meds like diuretics and beta-blockers
- Antipsychotics like haloperidol
It’s Not Just an Annoyance-It’s a Dental Emergency
Dry mouth doesn’t just make your lips crack or your tongue feel sticky. It’s accelerating tooth decay at a shocking rate. Studies show that within 12 months of developing dry mouth, the risk of cavities jumps by 300%. That’s not a typo. Three times faster than normal. Why? Saliva is your mouth’s toothpaste. Without it, acids from food and bacteria aren’t washed away. Plaque builds up fast. Gum disease follows. Root decay becomes common-especially in older adults. One study found that people on three or more medications have a 47% higher Root Caries Index than those on one or two. And it’s not just your teeth. Dry mouth makes it hard to speak clearly, taste food, or even wear dentures comfortably. Many people stop eating certain foods because chewing becomes painful. Some lose weight. Others get constant oral thrush infections. And because the symptoms are gradual, most people don’t connect the dots until they’re sitting in the dentist’s chair with multiple new cavities.What Medications Are Worst for Dry Mouth?
Not all drugs that cause dry mouth are created equal. Some are far worse than others.| Medication Class | Example Drug | Dry Mouth Incidence | Lower-Risk Alternative |
|---|---|---|---|
| Overactive Bladder | Oxybutynin (immediate-release) | 70% | Solifenacin (Vesicare) - 49% |
| Antihistamines | Diphenhydramine (Benadryl) | 58% | Loratadine (Claritin) - 12% |
| Antidepressants | Amitriptyline | 63% | Sertraline (Zoloft) - 31% |
| Antipsychotics | Haloperidol | 54% | Aripiprazole - 37% |

What You Can Do Right Now
Don’t just suffer through it. There are real, proven ways to fight back.- Review your meds with your doctor. Don’t stop anything on your own-but ask if there’s a less drying alternative. In 42% of cases, switching one drug improves symptoms without losing effectiveness.
- Use a prescription salivary stimulant. Pilocarpine (Salagen) and cevimeline (Evoxac) are FDA-approved for this. In clinical trials, they boost saliva by 63-72% within two weeks. They’re not magic, but they work.
- Use a dentist-recommended moisturizer. Biotene Dry Mouth Oral Rinse, Xerostom, or GC Dry Mouth Gel can give you 4-7 hours of relief. Apply them 5-6 times a day, especially after meals and before bed.
- Chew sugar-free gum with xylitol. Xylitol doesn’t just stimulate saliva-it fights cavity-causing bacteria. Gum with 100% xylitol as the first ingredient is best.
- Hydrate smartly. Sip water all day. Avoid caffeine, alcohol, and sugary drinks. They make dry mouth worse.
- Use a humidifier. Especially at night. A cool-mist humidifier in your bedroom can cut nighttime dryness by half.
When to See a Dentist (And How Often)
If you’re on meds and have dry mouth, you need to see your dentist more often. Not every six months. Every three. Standard cleanings won’t cut it. You need aggressive prevention: fluoride treatments, sealants on vulnerable teeth, and early detection of decay. Dentists can also prescribe high-strength fluoride toothpaste or antibacterial rinses that aren’t available over the counter. And here’s something most people don’t know: dentists are now trained to ask about your medications. In 2023, 89% of dentists routinely ask patients what they’re taking during their first visit. But only 52% feel confident managing the side effects. That’s why you need to speak up. Bring your medication list. Write down when your dry mouth started. Note if it’s worse after meals or at night. The more details you give, the better they can help.
The Bigger Picture: Why This Is Still Overlooked
It’s frustrating because this is one of the most common side effects-and one of the least talked about. Only 28% of primary care doctors screen for dry mouth during medication reviews. Most assume it’s just a “minor annoyance.” But it’s not. The American Dental Association calls it the single most significant medication-related oral health risk factor for older adults. And older adults are the most affected-76% of dry mouth cases are in people over 65. That’s the group taking the most meds. There’s progress. In 2023, 47 health systems launched pharmacist-dentist collaboration programs. Patients in these programs had 38% fewer dental complications. The FDA approved a new drug (cevimeline) in 2023. NIH is funding $15.7 million to find non-anticholinergic alternatives for bladder meds. But until doctors start asking and patients start demanding answers, this will keep slipping through the cracks.Real People, Real Stories
On Reddit, a user named XeroWarrior87 wrote: “I started Detrol for my bladder. Two weeks later, I had three cavities. I brushed twice a day. I flossed. I didn’t eat candy. How?” Another user on Healthgrades said: “I’ve been on sertraline for two years. I carry a water bottle everywhere. I wake up three times a night to drink. My dentist says I’m at high risk for root decay. No one ever warned me.” These aren’t rare cases. They’re the norm.What’s Next
The future is starting to shift. By 2027, the ADA predicts all new medications will need a dry mouth risk label. Insurance companies are slowly starting to cover salivary stimulants-though only 43% of dental plans do now. But you don’t have to wait for policy changes. You have power right now. Ask your doctor: “Is there a version of this drug that doesn’t dry out my mouth?” Ask your dentist: “Based on my meds, what’s my risk for decay? What can we do to prevent it?” Keep a log: When did the dry mouth start? What meds were added? Did it get worse after a dosage change? You’re not just managing a symptom. You’re protecting your long-term health.Can dry mouth from medication be permanent?
In most cases, no. Once you stop or switch the medication, saliva production usually returns within days to weeks. But if dry mouth has gone untreated for a long time, the salivary glands can become damaged. That’s why early action matters. If you’ve had dry mouth for over a year, talk to your dentist about whether your glands still function properly.
Does drinking more water help dry mouth from meds?
Drinking water helps with comfort, but it doesn’t fix the root problem. Your body isn’t making saliva-you’re just adding external moisture. That’s why water alone isn’t enough. You need products that stimulate saliva or replace its protective functions, like xylitol gum or prescription rinses.
Are over-the-counter dry mouth products effective?
Yes-but only if they’re the right kind. Look for products with xylitol, carboxymethylcellulose, or enzymes like lactoperoxidase. Avoid anything with alcohol, sugar, or citric acid. Brands like Biotene, GC Dry Mouth Gel, and Xerostom are clinically tested. Generic brands often just add flavor and sugar, which can make decay worse.
Can I switch my antidepressant to avoid dry mouth?
Possibly. Tricyclic antidepressants like amitriptyline cause dry mouth in 63% of users. SSRIs like sertraline or escitalopram cause it in only 31%. Talk to your doctor about whether switching is safe and appropriate for your mental health needs. Never stop antidepressants abruptly.
Why doesn’t my doctor mention this side effect?
Many doctors aren’t trained to connect dry mouth with dental health. They focus on the main reason you’re taking the drug-like lowering blood pressure or treating depression-and assume oral side effects are minor. But research shows it’s a major risk factor. Bring up the topic yourself. Say: “I’ve been having dry mouth. Is this a known side effect? Are there alternatives?”


Sally Denham-Vaughan
January 2, 2026Medication-induced xerostomia is a well-documented pharmacological side effect, primarily mediated through anticholinergic receptor antagonism at M3 muscarinic sites in salivary acinar cells. The clinical significance is grossly underappreciated in primary care settings.
Saliva's buffering capacity, lysozyme activity, and amylase-mediated clearance are critical for oral homeostasis. Its reduction directly correlates with increased caries incidence, as demonstrated in longitudinal cohort studies.
It's not merely discomfort-it's a systemic oral health risk multiplier.
Recommendation: Always audit polypharmacy regimens for anticholinergic burden using the Anticholinergic Cognitive Burden Scale.
Alternatives like solifenacin over oxybutynin are not just preferable-they're clinically superior in this context.
sharad vyas
January 3, 2026My uncle in Delhi takes five pills a day. His mouth is always dry. He drinks water like it’s oxygen. But he never told his doctor. He thought it was just old age.
Now he’s got five new fillings. No one warned him. Not the doctor. Not the pharmacist. Just the dentist, who asked one day, ‘What are you taking?’
People here don’t talk about this stuff. We just suffer. Maybe that’s why we have so many toothless grandpas.
LIZETH DE PACHECO
January 4, 2026This is so important. I’ve been on sertraline for years and thought my dry mouth was just ‘me being dehydrated.’ Turns out, it’s the med.
I started chewing xylitol gum and using Biotene at night. My dentist said my cavity risk dropped by half in six months.
You’re not being dramatic if you’re thirsty all the time. It’s real. And you deserve to feel better.
gerard najera
January 6, 2026Saliva is your mouth’s immune system. No saliva = no defense.
Kristen Russell
January 6, 2026Thank you for writing this. I’ve been too afraid to ask my doctor about switching meds because I didn’t want to seem ‘difficult.’ But now I’m going to bring my list and say: ‘Is there a less drying option?’
You’re not overreacting. You’re being smart.
Bill Medley
January 6, 2026My father took amitriptyline for ten years. He lost half his teeth by 72. No one ever connected the dots.
He didn’t brush poorly. He didn’t eat sugar.
His meds did it.
jaspreet sandhu
January 8, 2026Everyone’s blaming the meds, but what about the system? Doctors don’t care. Pharmacies push the cheapest option. Dentists get mad when you show up with rotting teeth. But no one asks: ‘Why did this happen?’
We’re just numbers in a spreadsheet. The system doesn’t care if you can’t chew your food or talk without swallowing air.
And don’t even get me started on how they charge $200 for a fluoride treatment while the pills that cause this cost $4.
It’s rigged.
Austin Mac-Anabraba
January 10, 2026Of course this is happening. Big Pharma doesn’t want you to know. They profit from your cavities. They profit from your root canals. They profit from your dentures.
They make the drugs that dry your mouth. Then they sell you the toothpaste to fix it.
It’s not an accident. It’s a business model.
And you’re the mark.
Phoebe McKenzie
January 10, 2026Oh my god. I’ve been on oxybutynin for three years. I thought I was just ‘getting old.’ Now I’m terrified. I’ve got four cavities I didn’t even know about. My dentist said I’m at ‘high risk for full-mouth reconstruction.’
My doctor never mentioned this. NEVER. I’m so mad right now.
I’m switching meds tomorrow. And I’m telling every person I know. This is a crime.
Alex Warden
January 11, 2026Why are we letting foreign drug companies control our health? The FDA approves these dry-mouth monsters while we import cheap pills from China and India. We need American-made alternatives.
And stop giving these meds to veterans. They’re already suffering enough.
Stephen Gikuma
January 12, 2026They’re doing this on purpose. The government wants us to be dependent on dentists. More visits = more control. More money for the dental-industrial complex.
They don’t want you to know you can just stop the meds. They want you to keep buying the rinses, the gum, the $80 fluoride treatments.
Wake up.
Todd Nickel
January 13, 2026There’s a fascinating neuropharmacological nuance here that rarely gets discussed: the differential affinity of second-generation anticholinergics for M1 vs M3 receptors. While oxybutynin has high M3 affinity (leading to pronounced salivary suppression), solifenacin’s selectivity for M3 over M1 reduces central and oral side effects while maintaining bladder efficacy.
Similarly, SSRIs like sertraline have minimal muscarinic receptor binding compared to tricyclics, which is why their dry mouth incidence is roughly half. This isn’t just ‘better’-it’s mechanistically superior.
Also, the 300% increase in caries risk isn’t linear-it’s exponential after 12 months, because plaque biofilm maturation accelerates in low-saliva environments. The critical window for intervention is under six months.
And yes, humidifiers help, but only if you’re using a true HEPA cool-mist model. Ultrasonic ones can spread mold spores, which worsens oral thrush risk in immunocompromised patients.
Most people don’t realize that xylitol isn’t just a sugar substitute-it’s a bacteriostatic agent that disrupts Streptococcus mutans ATP synthesis. That’s why 100% xylitol gum works better than anything with sorbitol or aspartame.
Also, the ADA’s 2027 labeling mandate is already being implemented by 12 major pharma companies preemptively. It’s not just a prediction-it’s a regulatory inevitability.
And if you’re on five or more meds? You’re statistically likely to have <10% of normal salivary flow. That’s not ‘a little dry.’ That’s pathological. You need a salivary scintigraphy scan to assess gland function, not just a ‘drink more water’ suggestion.
Olukayode Oguntulu
January 14, 2026Ah, the Western medical paradigm-reductionist, profit-driven, and utterly disconnected from holistic bodily intelligence. We treat symptoms like isolated events, not emergent phenomena of systemic imbalance.
Saliva isn’t just a fluid-it’s the body’s liquid wisdom, a biomarker of autonomic harmony. When it vanishes, it’s not the drug’s fault-it’s the *system’s* failure to honor homeostasis.
Why not ask: What is this medication trying to suppress? And what is the body trying to express through dryness?
Perhaps the real cure is not a new pill, but a new relationship with the self.
Meanwhile, I’ll be sipping herbal tea, meditating, and ignoring the dentists’ invoices.
Ann Romine
January 15, 2026I’ve been on a beta-blocker for five years. I never thought about dry mouth until I started having trouble swallowing pills.
Then I realized I couldn’t taste my coffee anymore.
I started using GC Dry Mouth Gel before bed. It’s not glamorous, but it’s the only thing that lets me sleep without waking up feeling like my tongue is sandpaper.
I wish my doctor had asked. I didn’t know to bring it up.
Sally Denham-Vaughan
January 16, 2026Re: Comment from user 6482 - switching from oxybutynin to solifenacin is not just advisable, it’s standard of care in urology guidelines as of 2023. The NNT for reduced dry mouth is 2.3. That’s better than most statins are for LDL reduction.
Also, the 70% incidence rate for oxybutynin is from older studies. Newer extended-release formulations reduce it to 42%. But most prescribers still default to immediate-release because it’s cheaper.
Ask for the extended-release version. It’s the same drug. Just slower. Less dry mouth. Same bladder control.