
When you’re in chronic pain, falling asleep isn’t just hard-it feels impossible. And when you finally do sleep, it’s rarely restful. You wake up stiff, sore, and worse off than before. Then the next night, the pain is even louder. This isn’t bad luck. It’s a cycle. And it’s more common than you think.
Over half of the 1.5 billion people living with chronic pain around the world struggle with sleep. For many, it’s not just that pain keeps them awake. It’s that not sleeping makes the pain worse. A single night of poor sleep can drop your pain tolerance by 10 to 20%. That means your usual ache turns into a flare. Your mild back pain becomes unbearable. Your fibromyalgia spikes from a 4 to an 8 on the pain scale. And it doesn’t take long-just four bad nights, and recovery can take weeks.
How Pain and Sleep Feed Each Other
The body doesn’t treat pain and sleep as separate problems. They’re wired together. When you don’t sleep enough, your brain’s natural painkillers slow down. Endogenous opioids-your body’s own morphine-like chemicals-drop by 30 to 40%. At the same time, your inflammatory signals ramp up. Cytokines like IL-6 rise by 25 to 35%, making your nerves more sensitive. Your nervous system starts screaming louder over quieter stimuli.
Meanwhile, your dopamine levels, which help regulate both mood and pain control, can fall by 20 to 30% after a sleepless night. That’s why people with chronic pain often feel more anxious, irritable, and emotionally drained when they’re sleep-deprived. It’s not just fatigue. It’s neurochemistry.
And it works the other way too. Pain doesn’t just keep you awake-it fragments your sleep. People with chronic pain take 25 to 30 minutes longer to fall asleep. They wake up 40 to 50% more often during the night. On average, they lose 45 to 60 minutes of total sleep each night. Their sleep efficiency drops below 90%, while healthy sleepers stay above 95%. The Pittsburgh Sleep Quality Index, a standard measure, shows scores of 10.5 for chronic pain patients versus 5.2 for those without pain. A score above 5 is already considered poor sleep. This isn’t just discomfort. It’s clinical insomnia.
Why Most Treatments Fail
Most pain clinics focus on one thing: reducing pain. Medications. Injections. Physical therapy. All important. But if sleep stays broken, the pain keeps coming back. A 2023 survey of over 1,200 patients found that clinics offering only pain treatment had a 3.2 out of 5 satisfaction rate. Those that included sleep support? 4.7 out of 5.
Why? Because over-the-counter sleep aids don’t fix the root problem. Melatonin, antihistamines, even prescription sleep pills-they might help you fall asleep for a few nights. But they don’t restore deep sleep. They don’t lower inflammation. They don’t reset your brain’s pain filters. And they often leave you groggy the next day, which makes pain perception worse. The Arthritis Foundation found that 42% of people using OTC sleep aids reported next-day grogginess that increased their pain.
Even worse, many doctors still treat pain and sleep as unrelated issues. A 2023 study showed that 68% of negative patient reviews cited one thing: "Doctors only treated pain, not sleep." That’s like trying to fix a leaky roof while ignoring the mold growing underneath.
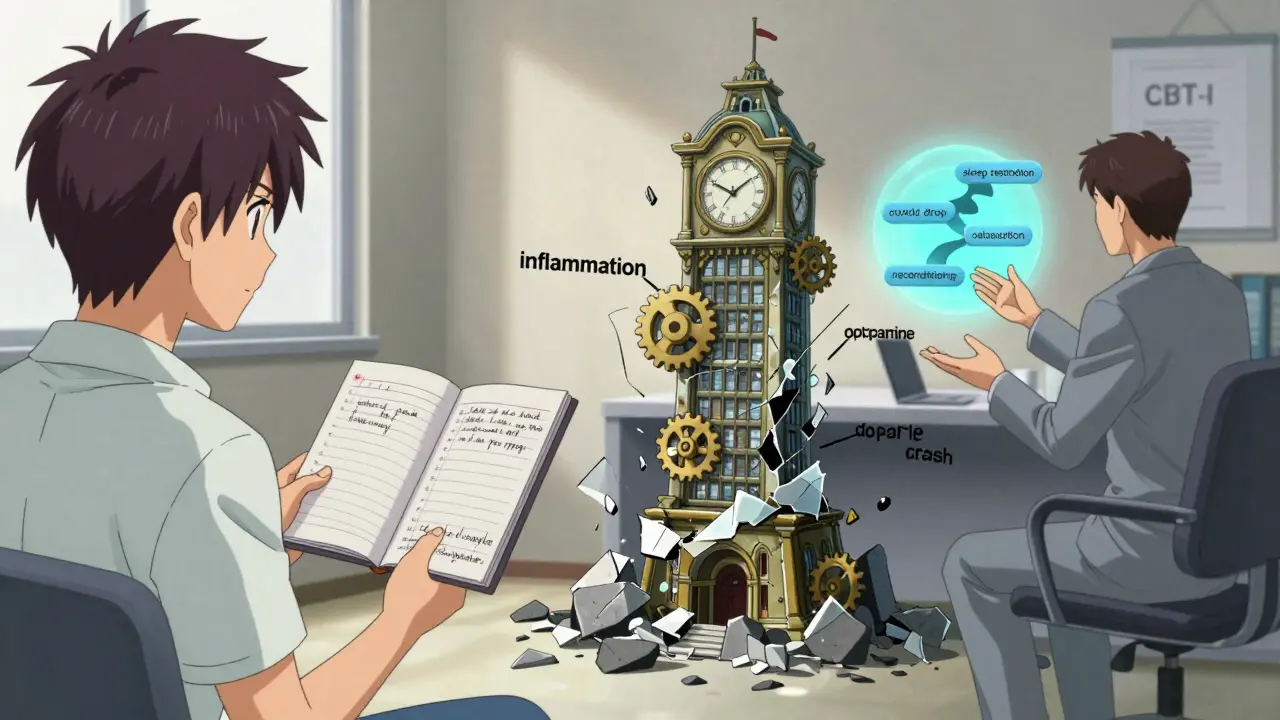
The Only Treatment That Breaks the Cycle
There’s one approach that consistently breaks the pain-sleep loop: Cognitive Behavioral Therapy for Insomnia (CBT-I). It’s not a pill. It’s not a gadget. It’s a structured, evidence-based program that rewires how you think about sleep.
Studies show CBT-I reduces insomnia symptoms in 65 to 75% of chronic pain patients. And it doesn’t stop there-it lowers pain intensity by 30 to 40%. How? By targeting the behaviors and thoughts that keep you stuck.
Here’s what CBT-I actually does for pain patients:
- Restricts time in bed to match actual sleep (so you’re not lying there for hours frustrated)
- Teaches you to stop associating your bed with pain and wakefulness
- Replaces anxiety about sleep with relaxation techniques
- Uses sleep diaries to identify patterns (like how pain flares after 3 nights of poor sleep)
- Gradually rebuilds deep sleep without relying on medication
After 8 to 10 weekly sessions, patients gain back 12 to 15 percentage points in sleep efficiency. Sleep onset latency drops by 25 to 30 minutes. Nighttime awakenings shrink by 35 to 40 minutes. And pain scores follow suit.
And it works even if you’re not a "perfect" sleeper. Digital CBT-I platforms like Sleepio have 60 to 65% effectiveness in chronic pain patients. While completion rates are lower than for people without pain (55% vs. 75%), those who stick with it see real change.
What About Medication?
There’s promising new research on drugs that target the biological link between pain and sleep. Researchers at the University of Arizona found that modulating kappa opioid receptors improved sleep quality by 40 to 60% in animal models. Human trials are underway, with phase 2 results showing 30 to 35% improvement in sleep and 25 to 30% reduction in pain scores for neuropathic pain patients.
But here’s the catch: these drugs aren’t available yet. And even when they are, they won’t replace behavioral therapy. They’ll complement it. Because pain isn’t just a chemical signal. It’s a learned response. And sleep isn’t just a biological function. It’s a habit.
Dr. Shiqian Shen from Massachusetts General Hospital puts it plainly: "Pain in human beings is a very subjective experience." Sleep loss doesn’t just make you sensitive to pain. It can create pain where none existed before.

How to Start Breaking the Cycle Today
You don’t need to wait for a new drug or a specialist appointment. Here’s what you can do right now:
- Keep a sleep and pain diary for two weeks. Track when you go to bed, how long it takes to fall asleep, how many times you wake up, how long you’re awake, and rate your pain on a scale of 1 to 10 each morning. You’ll spot patterns you never noticed.
- If your sleep score on the Insomnia Severity Index (ISI) is above 15, you have clinically significant insomnia. Don’t ignore it.
- Reserve your bed for sleep and sex only. No scrolling. No watching TV. No lying there worrying. If you’re not asleep in 20 minutes, get up and sit in dim light until you feel sleepy.
- Get sunlight within 30 minutes of waking. Natural light resets your body clock better than any supplement.
- Avoid caffeine after 2 p.m. and alcohol within three hours of bedtime. Both fragment deep sleep, even if you think they help.
- Try a 10-minute guided relaxation before bed-not sleep hypnosis, just breathing and muscle release. Apps like Calm or Insight Timer have free options.
And if you can, find a therapist trained in CBT-I. Not every sleep specialist offers it. Look for certifications from the American Academy of Sleep Medicine or the Behavioral Sleep Medicine Society. You can also ask your pain clinic if they have a behavioral health provider on staff.
The Bigger Picture
The pain-sleep cycle isn’t just about you. It’s a public health issue. In 2023, the NIH invested $12.7 million into research specifically targeting this cycle. Over 47 active clinical trials are underway. Pain clinics across the U.S. and Europe now screen for insomnia as standard practice-up from 35% in 2018 to 92% today.
Why? Because we finally understand: you can’t treat pain without sleep. And you can’t fix sleep without addressing pain.
The market for integrated solutions is growing fast-from $3.2 billion in 2023 to over $5.7 billion by 2028. But money doesn’t fix this. Knowledge does. Action does.
If you’ve been told, "Just deal with the pain," or "Take a pill to sleep," you’ve been given half a solution. The real answer is deeper. It’s in your routine. In your habits. In your mind. And it’s within reach.
Can chronic pain cause insomnia even without obvious physical triggers?
Yes. Chronic pain doesn’t need to be constant to disrupt sleep. Even intermittent pain, like flare-ups from arthritis or fibromyalgia, can condition your brain to stay alert at night. Your nervous system learns to expect pain, so it stays on guard-even when you’re not actively hurting. This hypervigilance prevents deep sleep, leading to insomnia even on days when pain feels mild.
Is it true that sleep deprivation can make you feel pain you don’t actually have?
Yes. Studies show that healthy people without prior pain conditions can develop widespread pain after just one night of total sleep deprivation. This isn’t psychological-it’s biological. Sleep loss lowers the brain’s pain threshold and increases activity in areas that process discomfort. In one experiment, participants reported muscle aches and joint pain after being kept awake for 24 hours, even though no injury or inflammation was present.
Why doesn’t sleeping more always help with chronic pain?
Because quantity doesn’t equal quality. Many chronic pain patients sleep for 8+ hours but spend most of it in light sleep, never reaching deep or REM stages. This leaves their body without the restorative processes needed to repair tissue and reset pain pathways. That’s why someone can sleep all night and still wake up exhausted and in pain. The goal isn’t more hours-it’s better sleep architecture.
Can CBT-I work if I’m on pain medication?
Yes. CBT-I is designed to work alongside medication. In fact, many patients use it to reduce their reliance on painkillers and sleep aids over time. CBT-I doesn’t interfere with medication-it helps you build habits that make medication less necessary. Some patients reduce opioid use by 30% after completing CBT-I, simply because their sleep improved and their pain sensitivity dropped.
How long does it take to see results from CBT-I for pain-related insomnia?
Most people notice small improvements within the first two weeks-like falling asleep 10 to 15 minutes faster or waking up fewer times. But meaningful changes in pain levels usually appear after 6 to 8 weeks. The key is consistency. CBT-I isn’t a quick fix. It’s a rewiring process. The brain needs time to unlearn the fear of sleep and relearn healthy patterns. Patients who complete the full 8-10 sessions report the most lasting results.
If you’ve been stuck in this cycle for months or years, it’s not your fault. It’s the system. But now you know the path out. Start with the diary. Build one small habit. And don’t wait for permission to treat your sleep like the medical issue it is.



Patrick Jarillon
February 8, 2026Okay but have you ever considered that this whole 'pain-sleep cycle' is just a pharmaceutical scam to sell CBT-I apps and sleep trackers?
My cousin in Dublin got diagnosed with 'chronic pain insomnia' after a chiropractor told him his spine was 'misaligned from WiFi radiation'. He spent $3k on a $200 mattress and now he sleeps on the floor with a tin foil hat.
They're not fixing sleep. They're selling you a new religion. CBT-I? More like CBT-Industrial Complex.
And don't get me started on 'sleep diaries'. Who writes those? The NSA? Next they'll be tracking your REM cycles to sell you targeted ads for melatonin gummies.
Wake up. This isn't medicine. It's a subscription model wrapped in neuroscience jargon. They want you dependent on apps, not your own body.
Try sleeping in a bunker. No screens. No data. No therapists. Just silence. That's the real cure. Not some 8-week digital program that charges you $99/month to count your breaths.
Jesse Lord
February 9, 2026Man I felt this so hard
I was in bed for 8 hours last night and still woke up like I'd been run over by a truck
Turns out I was only in deep sleep like 22 minutes
My doc just kept giving me pain meds and I was like why am I still a mess
Then I tried the bed-only-for-sleep thing and it felt weird at first but now I actually fall asleep in 15 mins instead of 2 hours
Not magic just simple dumb stuff that works
Also sunlight in the morning changed my life like literally
Amit Jain
February 10, 2026CBT-I is just another capitalist trap for broke people with chronic pain
Meanwhile the rich are getting gene therapies and IV melatonin drips while we're told to 'track our sleep diaries'
Who wrote this article a pharma rep?
I’ve had fibro for 12 years and no therapist in India gave me CBT-I because they don’t have the infrastructure
So I just took 3 Advil and passed out
And guess what? I slept better than after 6 weeks of breathing exercises
Stop gaslighting us with behavioral solutions when the system is broken
Fix healthcare. Not our bedtime routines.
Tola Adedipe
February 11, 2026Bro I tried the sleep restriction thing and I was a mess for the first week
Like I was crying at 3am because I was so tired and my back was screaming
But then on day 5 I actually slept 5 hours straight for the first time in 3 years
Now I’m at 7 hours most nights
And my pain score dropped from 8 to 5
It’s not easy but it’s not magic either
Just consistent stupid discipline
And yes I still take my meds
They work better now
Eric Knobelspiesse
February 12, 2026So if sleep deprivation can induce pain in healthy people... does that mean pain is just a glitch in the nervous system?
Like maybe it's not tissue damage at all... maybe it's just the brain overreacting because it's tired?
And if that's true... then maybe chronic pain isn't a disease... it's a software bug?
And CBT-I is like a system update?
Wait... is this why my therapist keeps saying 'your pain is real but your brain is lying'?
That sounds like something a cult leader would say... but also... kinda makes sense?
My head hurts now.
Heather Burrows
February 13, 2026I find it deeply irresponsible to suggest that people with chronic pain should 'just fix their sleep habits' when they’re already exhausted from navigating a broken healthcare system.
Who has the energy to keep a sleep diary when they can barely get out of bed?
And why is the burden always on the suffering to adapt?
Not on the system that ignores them?
It’s not about discipline. It’s about dignity.
And this article feels like a lecture from someone who’s never missed a night of REM sleep.
Ritu Singh
February 15, 2026While the scientific basis of the pain-sleep nexus is compelling, I must emphasize the cultural dimension often overlooked in Western-centric discourse.
In India, where chronic pain is frequently stigmatized as a sign of weakness, the very notion of 'sleep hygiene' clashes with familial obligations, multigenerational living, and the absence of private sleeping spaces.
CBT-I assumes individual autonomy - a luxury for many.
Perhaps the real intervention is not behavioral therapy alone, but community-based restorative ecosystems - where silence is not enforced, but shared; where rest is not a personal project, but a collective responsibility.
Let us not medicalize suffering into another individualized burden.
Let us heal together.
Mark Harris
February 15, 2026Just started my sleep diary today and already saw a pattern - my pain spikes after I drink coffee at 4pm
Who knew?
Also got up at 6am and walked outside for 10 mins - felt like a new person
Small changes. Big results.
You got this.
One day at a time.