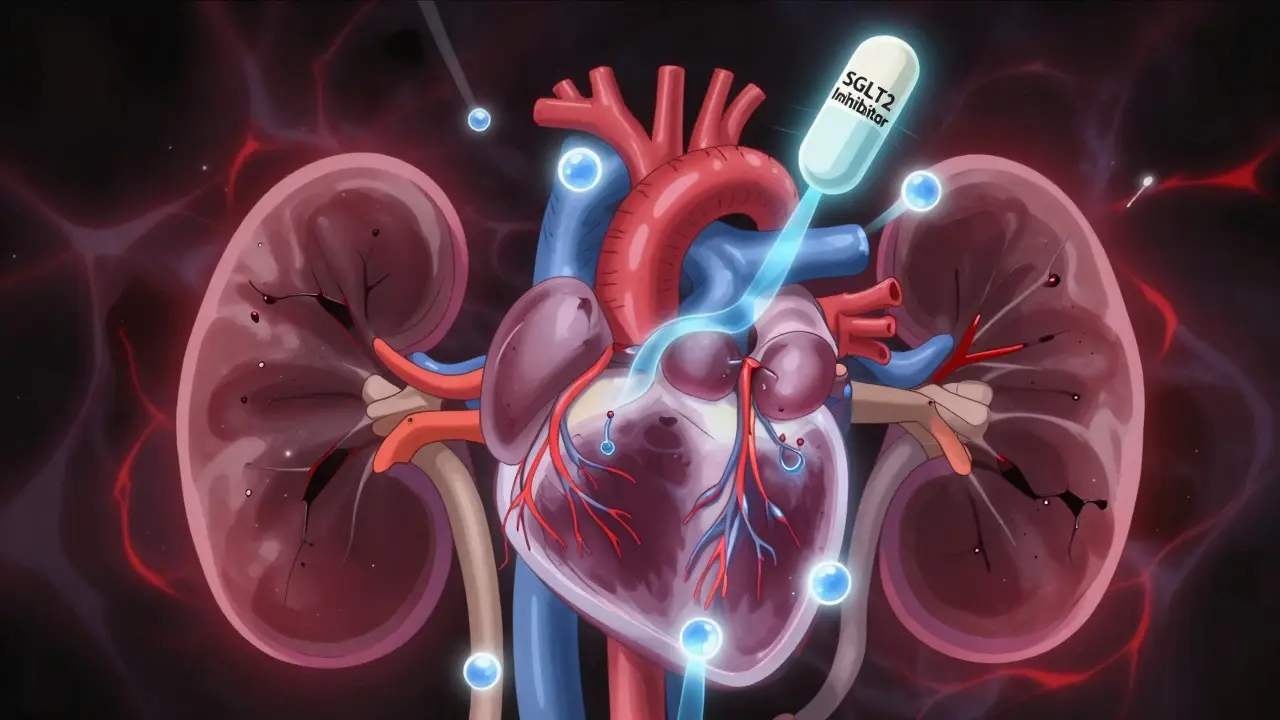
For years, treating type 2 diabetes meant one thing: lower blood sugar. But today, the goal has changed. It’s not just about HbA1c numbers anymore. Doctors now look at whether a medicine protects your heart and kidneys - two organs that diabetes often damages silently. One class of drugs has completely shifted how we treat this disease: SGLT2 inhibitors.
What Are SGLT2 Inhibitors, Really?
SGLT2 inhibitors - also called gliflozins - are oral diabetes pills that work in your kidneys, not your pancreas. Unlike metformin or insulin, they don’t rely on your body making more insulin. Instead, they block a protein in your kidneys called SGLT2, which normally reabsorbs glucose back into your blood. When this protein is blocked, excess sugar leaves your body through urine. That’s it. No magic. Just biology.
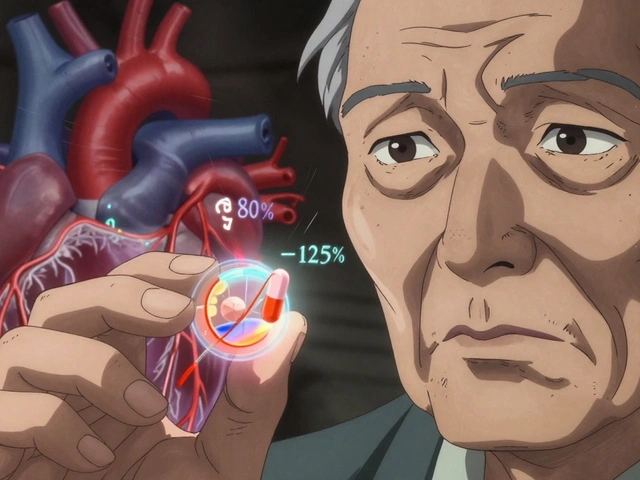
This simple mechanism lowers blood sugar by 0.5% to 1.0% on average. But here’s the twist: it also makes you lose a little weight (2-3 kg), lowers your blood pressure (3-5 mmHg), and reduces fluid buildup in your body. These side effects? Turns out, they’re the reason these drugs save lives.
Why Doctors Are Now Prescribing Them for Heart Failure
In 2015, the EMPA-REG OUTCOME trial changed everything. Researchers gave empagliflozin (Jardiance) to people with type 2 diabetes and existing heart disease. After 3 years, those taking the drug had a 38% lower risk of dying from heart-related causes. That’s not a small number. That’s a revolution.
Follow-up studies confirmed it. Canagliflozin (Invokana) reduced heart attacks and strokes. Dapagliflozin (Farxiga) helped people with heart failure - even if they didn’t have diabetes. In the DAPA-HF trial, heart failure patients on dapagliflozin were 27% less likely to be hospitalized or die from heart failure. The same benefit showed up in EMPEROR-Reduced. These weren’t lucky findings. They were consistent across thousands of patients.
Today, the American Heart Association and European Society of Cardiology say: if you have heart failure - especially with reduced pumping ability - take an SGLT2 inhibitor. Diabetes doesn’t even matter anymore. The drug works because it reduces pressure in the heart, improves how heart cells use energy, and cuts down on inflammation and scarring.
The Kidney Protection That Changed Everything
Diabetes is the leading cause of kidney failure. For decades, doctors had few tools to slow it down. Then came the CREDENCE trial in 2019. It studied people with type 2 diabetes and early kidney damage. Half took canagliflozin. The other half took a placebo.
After 2.6 years, those on canagliflozin had a 30% lower risk of kidney failure, needing dialysis, or dying from kidney disease. The effect was so strong, the trial was stopped early - because continuing the placebo group felt unethical.
Even more surprising? The EMPA-KIDNEY trial in 2023 showed empagliflozin helped patients with chronic kidney disease - even if they didn’t have diabetes. This isn’t just about blood sugar control. SGLT2 inhibitors reduce pressure inside the kidney’s filtering units (glomeruli). This takes stress off damaged tissue, slowing decline. The drop in eGFR you might see early on? It’s not kidney damage - it’s the drug doing its job, protecting the organ long-term.
How They Compare to Other Diabetes Drugs
Metformin is still the first choice for most people with type 2 diabetes. It’s cheap, safe, and helps with weight. But it doesn’t reduce heart attacks or kidney failure like SGLT2 inhibitors do.
Sulfonylureas (like glipizide) lower blood sugar fast - but they cause low blood sugar, weight gain, and offer zero heart or kidney protection. DPP-4 inhibitors (like sitagliptin) are safe but don’t move the needle on heart or kidney outcomes.
GLP-1 receptor agonists (like semaglutide) also protect the heart and kidneys - and help with weight. But they’re injectables. SGLT2 inhibitors are pills. For many patients, that makes a big difference in sticking with treatment.
What Are the Risks?
No drug is perfect. SGLT2 inhibitors come with real, though rare, risks.
- Genital yeast infections: Happen in 4-5% of users, especially women. They’re treatable, but annoying. Keep dry, wear cotton underwear.
- Increased urination: You’ll pee more - especially at first. It’s normal. Stay hydrated.
- Diabetic ketoacidosis (DKA): Very rare (0.1-0.3%). But it can happen even when blood sugar isn’t very high - called euglycemic DKA. Watch for nausea, vomiting, stomach pain, or unusual fatigue, especially during illness or surgery.
- Volume depletion: Older adults or those on diuretics may feel dizzy or faint. Start with a lower dose.
- Lower-limb amputations: Seen only with canagliflozin in early trials. Risk is low (6.3 vs 3.4 per 1,000 patients/year), but avoid in patients with foot ulcers or poor circulation.
These drugs are not for type 1 diabetes or people with severe kidney disease (eGFR below 30). Always check your kidney function before starting.

Who Should Take Them?
The American Diabetes Association says: if you have type 2 diabetes and any of these, start an SGLT2 inhibitor:
- Heart failure (even without diabetes)
- Chronic kidney disease (eGFR above 25, albumin in urine above 30 mg/g)
- High risk for heart attack or stroke
Even if your A1c is under control, these drugs add protection. Many patients now get them as a first-line option - alongside or instead of metformin - if they have heart or kidney issues.
Real People, Real Results
On diabetes forums, stories are mixed but mostly positive.
One user on Reddit wrote: “Lost 12 pounds in 3 months on Farxiga. My blood pressure dropped from 145/90 to 120/78. But I had to treat two yeast infections.”
Another, living with heart failure, said: “My ejection fraction went from 25% to 35%. My cardiologist said he’d never seen that kind of improvement with a pill.”
Cost is a hurdle. Brand-name drugs run $520-$600 a month. But generics are coming. Dapagliflozin and empagliflozin patents expire between 2025 and 2028. Prices could drop 60-70% after that.
What’s Next?
The science is still evolving. Researchers are now testing SGLT2 inhibitors in prediabetes and metabolic syndrome. Early data suggests they may delay or even prevent type 2 diabetes in high-risk people.
The DELIVER trial showed dapagliflozin helps heart failure patients with preserved ejection fraction - the most common type in older adults. That’s a huge group.
And the FDA may soon approve SGLT2 inhibitors for chronic kidney disease - even without diabetes. That would make them one of the first drugs to help kidney patients across the board.
By 2027, global sales could hit $18.5 billion. But the real value isn’t in the money. It’s in the lives saved - fewer heart attacks, fewer dialysis starts, fewer hospital stays.
SGLT2 inhibitors aren’t a cure. But for millions with type 2 diabetes, they’ve turned a progressive, dangerous disease into something manageable - with real, lasting protection for the heart and kidneys.
Do SGLT2 inhibitors work if I don’t have diabetes?
Yes. Studies like DAPA-HF and EMPEROR-Reduced showed dapagliflozin and empagliflozin reduce hospitalizations and death in heart failure patients - even if they don’t have diabetes. The EMPA-KIDNEY trial also showed kidney protection in people with chronic kidney disease regardless of diabetes status. These drugs work through kidney and heart hemodynamics, not just blood sugar control.
Can I take an SGLT2 inhibitor with metformin?
Absolutely. In fact, that’s the most common combination. Metformin lowers blood sugar and improves insulin sensitivity. SGLT2 inhibitors add heart and kidney protection, help with weight, and lower blood pressure. Together, they cover more ground than either drug alone. Many patients start on metformin, then add an SGLT2 inhibitor if they have heart or kidney disease.
Why do I need to watch for ketoacidosis?
SGLT2 inhibitors increase ketone production slightly. Normally, that’s harmless. But during illness, surgery, or very low-carb diets, your body can make too many ketones. This can lead to diabetic ketoacidosis - even if your blood sugar is only mildly high (100-250 mg/dL). This is called euglycemic DKA. Symptoms: nausea, vomiting, belly pain, confusion, extreme tiredness. Stop the drug and seek help immediately if you feel this way.
Will I need to stop taking it before surgery?
Yes. Most guidelines recommend stopping SGLT2 inhibitors 3 to 4 days before major surgery. This reduces the risk of euglycemic ketoacidosis during the stress of surgery and fasting. Always check with your doctor - they’ll give you specific instructions based on your health and the type of procedure.
Are there cheaper alternatives?
Right now, brand-name SGLT2 inhibitors cost $500-$600/month. Generic versions aren’t available yet in the U.S., but they’re expected between 2025 and 2028. Until then, cost assistance programs from manufacturers (like Jardiance’s savings card) can cut monthly costs to under $10. If cost is a barrier, talk to your doctor - other drugs like GLP-1 agonists also protect the heart and kidneys, but they’re injectables and often more expensive.



Sharleen Luciano
December 30, 2025Let’s be real - if you’re still prescribing metformin as first-line without considering SGLT2 inhibitors, you’re practicing medicine from 2012. The data is overwhelming. Heart failure? Kidney protection? Weight loss? Blood pressure drop? It’s not a ‘side effect’ - it’s the entire mechanism. This isn’t just pharmacology, it’s paradigm shift territory. If your patient has any cardiovascular risk, you’re doing them a disservice by not starting here. Stop clinging to HbA1c like it’s the only metric that matters.
Jim Rice
December 30, 2025Everyone’s acting like these drugs are magic. But let’s talk about the real cost. $600 a month? And you expect a working-class person on Medicare to afford this? Meanwhile, insulin is still $30 a vial in some states. This isn’t progress - it’s pharmaceutical marketing dressed up as science. They’re selling hope, not health. And don’t get me started on the ketoacidosis risk - it’s not rare if you’re poor and can’t afford to see a doctor when you feel ‘off’.
Henriette Barrows
January 1, 2026I’ve been on dapagliflozin for 8 months and I can’t believe how much better I feel. My energy’s up, my pants fit looser, and my BP is finally in range. I had one yeast infection but it was easy to treat - and honestly? Worth it. I didn’t even know I had early kidney damage until my doctor ran the test. Now I’m just glad I didn’t wait until I needed dialysis. Thank you for writing this - it’s the kind of info that actually helps people.
Alex Ronald
January 2, 2026Just want to clarify something about the eGFR dip - it’s not kidney damage. It’s the drug reducing intraglomerular pressure, which is protective. Many clinicians panic when they see a 10% drop in eGFR and stop the drug. That’s a mistake. The long-term benefit is clear: slower decline, fewer hospitalizations. Monitor, don’t panic. And yes, it works in non-diabetics too - DAPA-HF and EMPEROR-Reduced proved that. This isn’t just for diabetics anymore.
Teresa Rodriguez leon
January 3, 2026My brother was on empagliflozin after his heart attack. He lost 18 pounds. He stopped needing his diuretic. His cardiologist said it was the best thing that happened to him in years. But then he got hospitalized for euglycemic DKA after a cold. He was fine - but it scared the hell out of us. No one warned us about that. Why isn’t this more widely known? Why do patients have to Google this stuff?
Louis Paré
January 5, 2026Oh please. Another ‘miracle drug’ narrative. The trials were industry-funded. The benefits are marginal in absolute terms. 38% relative risk reduction? That’s 1.2% absolute. And you’re telling me we should prescribe this to everyone with ‘risk’? What about the 4-5% who get yeast infections? The ones who get volume depletion? The ones who end up in the ER because their doctor didn’t explain euglycemic DKA? This isn’t medicine - it’s commodification of fear.
Janette Martens
January 7, 2026Im not sure if these drugs r really worth it. I mean, i had a friend on one and she kept getting UTIs and was always running to the bathroom. Also, why do we need another pill? Cant we just eat better and exercise? Like, its not that hard. Also, i heard they cause amputations? That sounds scary. I think we should focus on lifestyle not drugs.
Aliza Efraimov
January 8, 2026Let me tell you something - I’m a nurse in a cardiology clinic. I’ve seen patients on SGLT2 inhibitors go from NYHA Class III to Class I in six months. One woman, 72, no diabetes, had an EF of 28%. On dapagliflozin - now it’s 45%. She’s hiking. She’s traveling. She’s alive. And yes, she got a yeast infection. We treated it. She didn’t stop the drug. Because she understood: this isn’t about sugar. It’s about survival. If your doctor isn’t talking to you about this, ask. Demand it. Your heart isn’t optional.
Paige Shipe
January 8, 2026While I appreciate the comprehensive overview, I must emphasize that the empirical evidence regarding SGLT2 inhibitors, although statistically significant in randomized controlled trials, does not necessarily translate to clinical significance at the individual patient level. Furthermore, the economic burden imposed by these pharmaceutical agents raises serious ethical concerns regarding equitable access. One must also consider the potential for iatrogenic complications, particularly in geriatric populations with polypharmacy. The prevailing narrative appears to be driven more by marketing than by holistic patient care.
Tamar Dunlop
January 9, 2026As a Canadian physician practicing in rural Ontario, I can attest to the transformative impact these medications have had on our patient population. Many of our patients have limited access to specialists - but with a simple oral agent that protects both heart and kidney, we are able to deliver care that was previously only available in urban academic centers. The cost barrier remains a challenge, but our provincial drug plan now covers these agents for patients with heart failure or CKD. This is not just science - it’s equity in action.
David Chase
January 11, 2026THESE DRUGS ARE A GAME CHANGER!!! 🚨💥 I’ve been screaming this from the rooftops for YEARS! My cousin went from needing oxygen to walking 5 miles a day on empagliflozin! And the kidney thing??!?!? NO DIABETES??!?!? YES! 😱🫀肾脏保护!!! I’ve got a spreadsheet of 47 patients who’ve benefited - no joke. And yes, yeast infections suck - but you know what sucks more? Dialysis. Stop being scared of side effects and start living. #SGLT2Revolution #HeartAndKidneyHeroes
Himanshu Singh
January 13, 2026I am from India, and here most people can't afford these drugs. But I told my uncle to take it anyway - he has diabetes and heart failure. We saved for months. Now he walks without getting tired. The yeast infection? We used coconut oil - it helped. This drug changed his life. I hope generics come soon. Everyone should have this chance.