Rapid-Acting Insulin: How It Works and What You Need to Know
When you eat, your blood sugar rises — and rapid-acting insulin, a fast-acting form of insulin designed to mimic the body’s natural response to meals. Also known as mealtime insulin, it starts working in as little as 15 minutes and clears your system within 3 to 4 hours. This makes it the go-to choice for people with type 1 diabetes and many with type 2 who need precise control after eating. Unlike longer-acting insulins that keep your baseline level steady, rapid-acting insulin is all about timing: you take it right before or just after a meal to match the sugar spike.
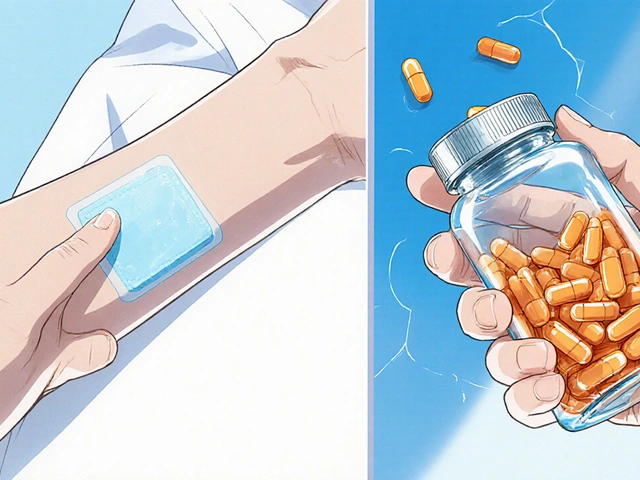
It’s not just about the insulin itself — it’s about how it fits into your daily life. People who use it often pair it with continuous glucose monitors, devices that track blood sugar in real time to fine-tune doses. Others rely on insulin pens, portable, easy-to-use tools that deliver exact doses without syringes. These aren’t just gadgets — they’re critical for avoiding dangerous highs and lows. If your blood sugar jumps too high after eating, rapid-acting insulin can bring it down fast. But if you take too much or eat less than planned, you risk hypoglycemia — which is why knowing your carb intake matters as much as the dose.
What you won’t find in most doctor’s offices is how messy this can get in real life. One person might take it before a big breakfast; another might skip it for a light salad. Some use it with insulin pumps, wearable devices that deliver small, steady doses throughout the day, while others stick to injections. The key is personalization. There’s no one-size-fits-all plan. Your body, your meals, your schedule — they all shape how you use it. That’s why so many of the posts below dive into real-world challenges: how to avoid dosing errors, how diet affects insulin needs, and why some people switch between different types of insulin over time.
What you’ll find in the collection below isn’t just theory. It’s stories from people managing diabetes every day, comparisons of insulin brands, and practical tips on avoiding common mistakes — like taking insulin too early or too late, or not adjusting for activity. You’ll see how rapid-acting insulin fits into bigger conversations about medication safety, cost, and long-term health. Whether you’re new to insulin or have been using it for years, these posts give you the real details — not the brochures.
Insulin stacking-giving rapid-acting insulin too soon after a previous dose-can cause dangerous low blood sugar. Learn how to avoid it with safe dosing intervals, real-world examples, and practical prevention tips.