JAK Inhibitors – What They Are and Why You Should Care
If you’ve heard doctors mention “JAK inhibitors” and felt confused, you’re not alone. These are a class of medicines that block tiny proteins called Janus kinases (or JAKs) inside your cells. By stopping those proteins from sending signals, the drugs calm down inflammation and slow disease‑related processes.
Why does this matter? Because many chronic conditions – rheumatoid arthritis, psoriatic arthritis, ulcerative colitis, even certain blood cancers – rely on that over‑active JAK signaling to keep symptoms going. When a JAK inhibitor steps in, it can bring relief where older drugs sometimes fall short.
Common JAK Inhibitor Drugs You Might See
The most talked‑about names are tofacitinib (Xeljanz), baricitinib (Olumiant) and ruxolitinib (Jakafi). Each one targets slightly different JAK proteins, which means doctors pick the right one based on your diagnosis. For example, tofacitinib is approved for rheumatoid arthritis and ulcerative colitis, while ruxolitinib is used mainly for myelofibrosis – a rare bone‑marrow disorder.
These pills are usually taken once or twice daily, which many patients find easier than frequent injections. They’re also oral options when you need something fast‑acting and convenient.
Safety and Monitoring Tips
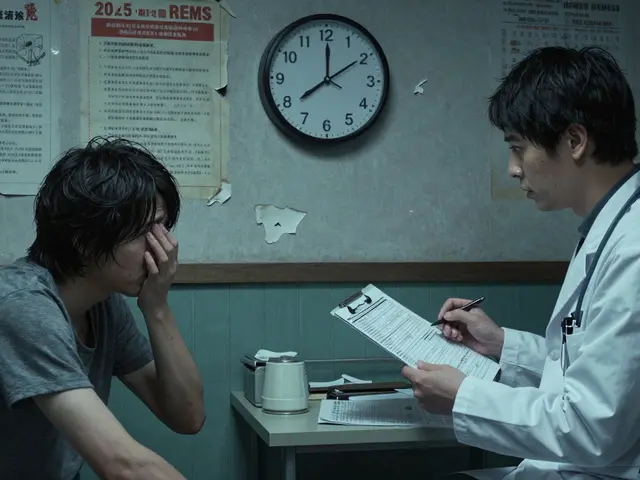
JAK inhibitors aren’t a free pass – they come with real side effects. The biggest concerns are infections (especially shingles), blood clots, and changes in cholesterol or liver enzymes. That’s why regular check‑ups are key. Your doctor will likely run blood work every few months to catch any issues early.
If you’re on a JAK inhibitor, stay alert for fever, persistent cough, unusual bruising, or sudden joint pain. Those could signal an infection or clot risk and need immediate medical attention.
A practical tip: keep a simple health diary. Note the date you start the medication, any new symptoms, and your lab results. Sharing this with your doctor makes it easier to adjust dose or switch drugs if needed.
Another thing to consider is vaccine timing. Because JAK blockers can weaken immune responses, many doctors recommend getting flu and COVID‑19 shots before starting therapy, or at least spacing them out appropriately.
Finally, don’t stop the medicine on your own. If you’re feeling better, that’s great, but abruptly quitting can cause a flare‑up of your condition. Always discuss any changes with your prescriber first.
Bottom line: JAK inhibitors have opened a new door for treating stubborn inflammatory diseases, offering oral convenience and strong results. Knowing how they work, the main drugs available, and what to watch out for will help you use them safely and get the most benefit.