Insulin Dosing Intervals: When to Take Insulin for Best Blood Sugar Control
When you take insulin, a hormone used to manage blood sugar in people with diabetes. Also known as insulin therapy, it's not just about how much you inject—it's about when you inject it. Take it too early, and your blood sugar crashes before you eat. Take it too late, and your numbers spike hard after meals. Millions of people with type 1 diabetes, a condition where the body doesn’t make insulin at all and many with type 2 diabetes, where the body doesn’t use insulin properly struggle with this daily.
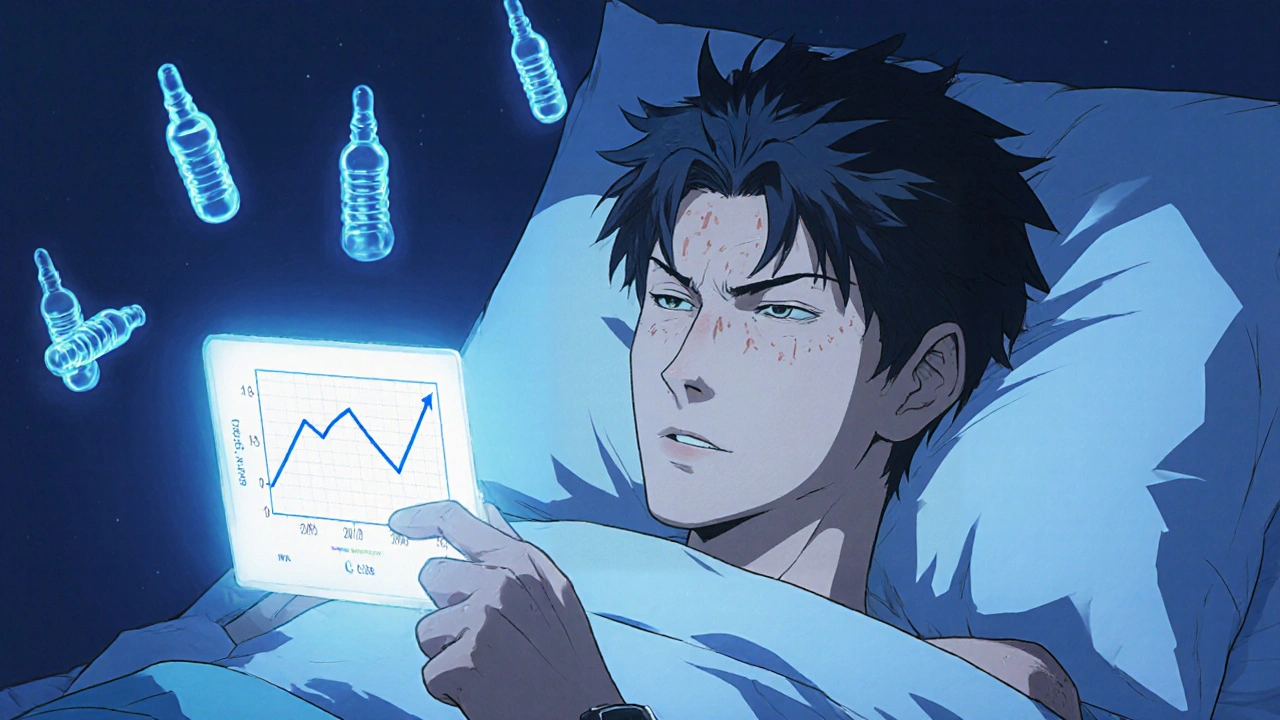
There’s no universal rule. Some need rapid-acting insulin 15 minutes before meals. Others take it right after eating. Some use long-acting insulin once a day at bedtime. The timing depends on your insulin type, your meals, your activity level, and even your body’s natural insulin resistance patterns. A person eating a high-fat meal might need a different schedule than someone eating carbs alone. Studies show that even a 30-minute shift in timing can change your A1C by half a point. It’s not magic—it’s math, and your body’s rhythm.
Many patients don’t realize their doctor’s dosing advice is a starting point, not a rulebook. Real control comes from tracking your numbers after meals, noticing patterns, and adjusting when you take insulin. Some use insulin pumps that let them fine-tune delivery minute by minute. Others rely on multiple daily injections and careful food logging. The goal isn’t perfection—it’s consistency. You don’t need to guess. You need to observe.
Below, you’ll find real-world guides on how people manage insulin timing, what happens when it’s off, and how to work with your doctor to find your best schedule. No fluff. Just what works.
Insulin stacking-giving rapid-acting insulin too soon after a previous dose-can cause dangerous low blood sugar. Learn how to avoid it with safe dosing intervals, real-world examples, and practical prevention tips.