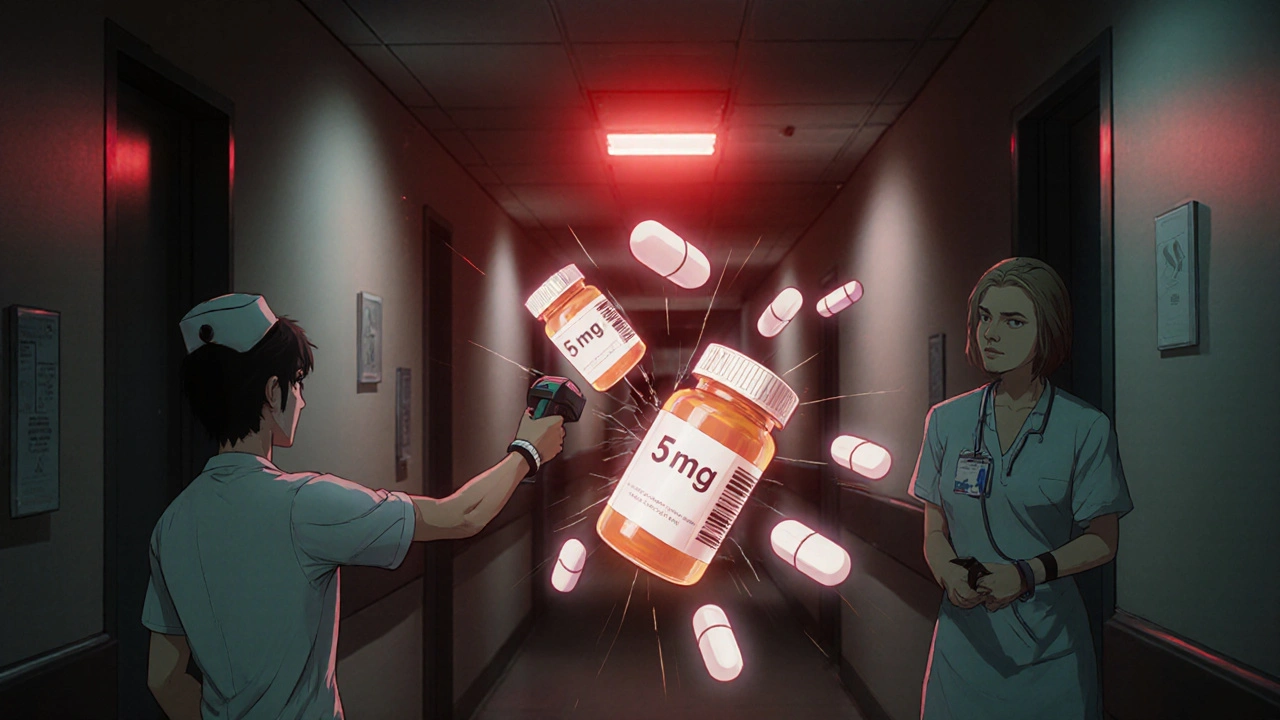
Identify Medication Mistakes: Avoid Dangerous Errors with Smart Practices
When you take medication, identify medication mistakes, errors in how drugs are prescribed, dispensed, or taken that can lead to serious harm or death. Also known as drug errors, these aren’t just accidents—they’re often preventable, and they happen more often than you think. A 2023 study in the Journal of Patient Safety found that over 7 million medication errors occur in the U.S. each year, and nearly half involve drugs people are already taking. Many of these mistakes happen because patients don’t know what to watch for—or how to ask the right questions.
One major type of error is duplicate medications, when a patient gets the same drug or a very similar one from different doctors without realizing it. This happens often after specialist visits, especially for seniors. For example, someone might get metformin from their primary care doctor and another diabetes pill from an endocrinologist, not knowing both raise the same risk of low blood sugar. Another common mistake is drug interactions, when two or more medications react in a way that makes one less effective or dangerously strong. Think of mixing PDE5 inhibitors like Viagra with nitrates—this combo can drop blood pressure to life-threatening levels. Or taking linezolid while eating aged cheese, which can trigger a sudden, deadly spike in blood pressure.
Then there’s the growing problem of counterfeit medications, fake pills sold online that look real but contain fentanyl, no active ingredient, or the wrong dose. These aren’t rare outliers—they’re everywhere. A single pill bought from an unlicensed website could kill you. Even generic drugs aren’t always safe if you switch between different brands without monitoring, especially for drugs like digoxin, where tiny changes in blood levels can cause toxicity or treatment failure.
It’s not just about what you take—it’s about how you take it. Insulin stacking—giving another dose too soon after the last one—is a silent killer for diabetics. Taking aspirin daily when you’re over 60 might do more harm than good. Herbal supplements like garlic or turmeric can thin your blood as much as warfarin, and no one tells you that until you’re bleeding internally. These aren’t theoretical risks. People die from them every day.
You don’t need to be a doctor to stop these mistakes. You just need to know what to look for: mismatched pill colors, unexplained side effects, multiple prescriptions for the same condition, or a pharmacy that doesn’t ask questions. Keep a written list of everything you take—including vitamins and herbs—and bring it to every appointment. Ask your pharmacist: "Is this new drug safe with what I’m already on?" Use one pharmacy so they can flag conflicts. Don’t assume your doctor knows how much your meds cost—many don’t, and that affects what they prescribe.
Below, you’ll find real cases and clear advice on how to spot and stop these errors before they hurt you. From how to avoid duplicate pills after a specialist visit, to why your generic digoxin might be riskier than you think, to what foods can turn your antidepressant into a heart attack waiting to happen—this collection gives you the tools to take control. No fluff. No jargon. Just what you need to stay alive and well.