DMARD: What It Is, How It Works, and Why It Matters for Chronic Autoimmune Conditions
When your immune system turns on your own body—attacking joints, skin, or organs—you need more than painkillers. That’s where DMARD, disease-modifying antirheumatic drugs that slow or stop the progression of autoimmune diseases. Also known as disease-modifying antirheumatic drugs, these medications don’t just mask symptoms. They change the course of conditions like rheumatoid arthritis, lupus, and psoriatic arthritis. Unlike NSAIDs or steroids, which give quick relief but don’t stop damage, DMARDs work slowly, often taking weeks or months to show results. But when they work, they prevent long-term joint destruction, organ damage, and disability.
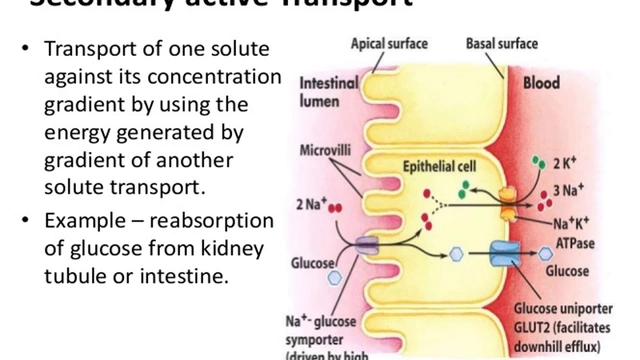
There are two main types: traditional DMARDs and biologic DMARDs. Traditional DMARDs, like methotrexate, hydroxychloroquine, and sulfasalazine, are older, cheaper, and often the first line of treatment. They work by broadly suppressing the immune system. Biologic DMARDs, like adalimumab or etanercept, target specific parts of the immune response—like TNF-alpha or B-cells. These are more powerful, but also more expensive and carry higher infection risks. Both types require regular blood tests to watch for liver or bone marrow side effects. Many people start with a traditional DMARD and add a biologic if the first one doesn’t cut it.
What you won’t find in most doctor’s offices is how often patients stop taking these drugs too soon—because they don’t feel better after two weeks. But DMARDs aren’t like antibiotics. You can’t rush them. The real win isn’t immediate pain relief. It’s avoiding a wheelchair, a joint replacement, or kidney failure five years down the line. That’s why sticking with them—even when you feel okay—is critical. And if cost or side effects are a problem, there are alternatives. Some patients switch to newer oral DMARDs like tofacitinib, which work like biologics but come as pills. Others combine them with lifestyle changes, like low-impact exercise or anti-inflammatory diets, to reduce the dose needed.
What you’ll find in the posts below is real-world insight into how DMARDs fit into daily life. From how they interact with other meds like blood thinners or antibiotics, to why some generics behave differently, to what happens when supply chains break down and patients can’t get their pills. You’ll see how pharmacist substitution rules affect access, how genetic differences change how your body handles these drugs, and why monitoring isn’t optional—it’s life-saving. These aren’t theoretical discussions. They’re stories from people managing chronic illness, trying to stay healthy while navigating a broken system. If you’re on a DMARD, or someone you care about is, this collection gives you the practical, no-fluff facts you won’t get from a drug label.