
RA Treatment Cost Estimator
Estimate Your RA Treatment Costs
When you're living with rheumatoid arthritis (RA), the goal isn't just to manage pain-it's to stop the damage before it steals your mobility. That’s where DMARDs come in. These aren't your average painkillers. They're disease-modifying drugs designed to slow or even halt the immune system's attack on your joints. And when they don't do enough alone, doctors turn to biologics. But mixing these two types of medications isn't simple. It’s a balancing act between effectiveness, side effects, and cost-and knowing how they interact can make all the difference.
What DMARDs Actually Do
Disease-modifying antirheumatic drugs (DMARDs) are the foundation of RA treatment. They don’t just mask symptoms. They change how your immune system behaves. There are two main types: conventional synthetic DMARDs (csDMARDs) and biologic DMARDs (bDMARDs). The most common csDMARD is methotrexate. It’s been used since the 1980s, works by blocking folate metabolism, and is usually taken once a week as a pill or injection. It’s cheap-around $20 to $50 a month-and effective for many people. About 20% to 30% of early RA patients reach remission on methotrexate alone. Other csDMARDs like sulfasalazine, hydroxychloroquine, and leflunomide are often used in combination. These aren’t new drugs; they were originally made for malaria or cancer. But their immune-suppressing side effects turned out to help RA. They work broadly, slowing down the whole immune system. That’s why they’re called “conventional.” They’re not picky. They hit multiple targets.How Biologics Are Different
Biologics are a newer generation of DMARDs. Unlike pills, they’re made from living cells and are large protein molecules. Because of their size, they can’t be swallowed-they have to be injected or infused. You’ll get them as a shot under the skin (like adalimumab or etanercept) or through an IV (like infliximab or rituximab). They’re expensive-$1,500 to $6,000 a month-but they’re precise. Instead of suppressing your whole immune system, they target one specific part of it. For example:- TNF inhibitors (adalimumab, etanercept, infliximab) block tumor necrosis factor, a key inflammation driver.
- Abatacept stops T-cells from activating by blocking a signal called CD80/86-CD28.
- Rituximab wipes out B-cells that produce harmful antibodies.
- Tocilizumab shuts down interleukin-6, another major inflammation signal.
- Anakinra blocks interleukin-1, but it’s less effective than the others.
These drugs are powerful. Studies show they’re about 3 to 5 times more likely than placebo to reduce RA symptoms by at least 50% (ACR50 response). But they also come with risks-especially infections. People on biologics are more likely to get pneumonia, tuberculosis, or skin infections. That’s why you need screening before starting one.
Why Methotrexate Is Still the Anchor
Even with all the fancy biologics, methotrexate is still the go-to first step. Why? Because it works well, it’s affordable, and it makes biologics work better. A 2015 study found that when biologics are combined with methotrexate, the chance of hitting a 50% improvement in symptoms jumps from 30-40% to 50-60%. That’s a big leap. Doctors don’t just add biologics randomly. They wait. If you’ve been on methotrexate for 3 to 6 months and your joint pain, swelling, or blood markers (like CRP or ESR) haven’t improved enough, that’s when they consider adding a biologic. This is called the “treat-to-target” approach. The goal isn’t just less pain-it’s remission. No swelling. No damage. Normal blood work. But here’s the twist: some people can’t tolerate methotrexate. About 20% to 30% get nauseous, tired, or have liver issues. In those cases, doctors might try other csDMARDs, lower the dose, switch to subcutaneous injections, or add folic acid (5-10 mg daily) to reduce side effects. If none of that works, they’ll start a biologic alone. About 33% of people on biologics in real-world settings are on monotherapy-mostly because methotrexate didn’t sit well with them.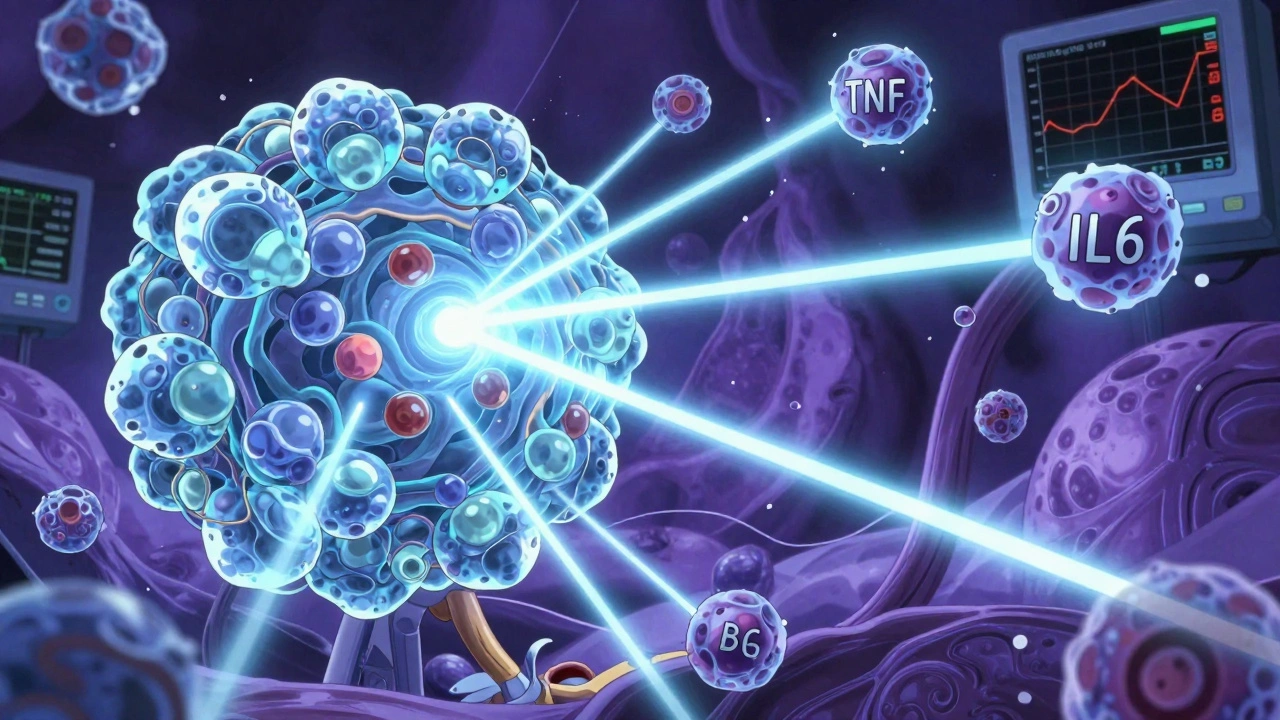
What Happens When You Combine Them?
Combining a biologic with methotrexate isn’t just about doubling up. It’s about synergy. Methotrexate helps your body tolerate the biologic better. It reduces the chance your immune system will make antibodies against the biologic drug-which can make it stop working. That’s called immunogenicity. Studies show biologics last longer and work better when paired with methotrexate. But it’s not always better. A 2013 trial called CAMERA-II found that a triple csDMARD combo (methotrexate + sulfasalazine + hydroxychloroquine) worked just as well as adalimumab plus methotrexate over two years. That surprised a lot of doctors. It means for some people, especially those without aggressive disease, you might not need a biologic at all. Then there’s the 2023 CAMERA-III trial, which showed the same thing over four years. The csDMARD combo matched the biologic combo in remission rates and joint damage prevention. So if cost or access is an issue, a triple DMARD combo is a valid, evidence-backed alternative. But if you have high-risk features-like high levels of rheumatoid factor or anti-CCP antibodies, early joint erosion, or very high disease activity-then biologics give you a better shot at ACR70 (70% improvement). That’s the kind of response that means you can actually go back to work or play with your kids without pain.The Rise of JAK Inhibitors
There’s a third category now: targeted synthetic DMARDs, or tsDMARDs. These are the JAK inhibitors-tofacitinib, baricitinib, and upadacitinib. They’re pills, like methotrexate, but they work inside cells to block signaling pathways that cause inflammation. They’re faster-acting than biologics and don’t need injections. Upadacitinib (Rinvoq) got FDA approval in 2023 for early RA as a standalone treatment-and it matched methotrexate in remission rates at six months. That’s huge. It means for patients who can’t take methotrexate or don’t want injections, there’s now a powerful oral option. But JAK inhibitors come with serious warnings. The FDA added a black box warning in 2021 after the ORAL Surveillance trial showed higher risks of heart problems, cancer, and blood clots, especially in people over 50 with heart disease risk factors. So they’re not first-line for everyone. They’re usually reserved for patients who haven’t responded to biologics or can’t use them.Cost, Access, and Biosimilars
Biologics are expensive. A single dose of adalimumab can cost over $6,000 a month. That’s why many patients skip doses or stop taking them. In a 2022 survey, 28% of RA patients admitted they didn’t take their meds because of cost. That’s dangerous-it leads to flare-ups and permanent joint damage. Enter biosimilars. These are near-identical copies of brand-name biologics, approved after patents expired. The first one, Amjevita (adalimumab biosimilar), came out in 2016. Now, biosimilars make up 28% of the U.S. biologic market. They cost 15% to 30% less. For some patients, that’s the difference between staying on treatment and quitting. In countries like India, where a biologic can cost 300% to 500% of a monthly household income, csDMARDs are the only realistic option. Even in the U.S., many insurers require you to try methotrexate first before approving a biologic. It’s not just medical-it’s economic.
Real-Life Challenges
It’s not just about the science. It’s about living with it. Giving yourself a biologic shot every week sounds simple until you’re shaking from anxiety or the needle breaks. About 85% of patients learn to self-inject after one or two training sessions with a nurse. But 8% report injection site reactions so bad they switch meds. Infections are the biggest fear. One in five negative reviews on drug sites mention serious infections. Some people get pneumonia. Others get reactivated TB. That’s why you need a chest X-ray and TB test before starting. You also need blood tests every few months to check liver and kidney function. And then there’s the mental load. Keeping track of multiple medications, appointments, insurance paperwork, and side effects is exhausting. Specialty pharmacies handle 95% of biologic dispensing. They send your meds, answer questions, and help with prior authorizations. Patient assistance programs can cover 30% to 50% of out-of-pocket costs if you qualify. But you have to ask.What’s Next?
The future is moving toward more targeted therapies. New drugs are being tested that block GM-CSF or use even more selective JAK inhibitors like deucravacitinib. Ultrasound and MRI are now being used to measure remission-not just how you feel, but whether the inflammation is truly gone in your joints. The 2024 draft of the ACR guidelines now includes imaging-based remission as a goal. That’s a shift. We’re no longer just guessing if treatment is working. We’re seeing it. But the core hasn’t changed. Methotrexate is still the anchor. Biologics are the boosters. JAK inhibitors are the oral alternative. And biosimilars are making all of this more accessible.What Should You Do?
If you’ve just been diagnosed with RA:- Start with methotrexate unless you can’t tolerate it.
- Ask about folic acid to reduce side effects.
- Don’t rush to biologics-give it 3 to 6 months.
- If you’re not improving, talk about adding a biologic or switching to a JAK inhibitor.
- Ask about biosimilars-they’re just as effective and cheaper.
- Use patient support programs. You’re not alone.
If you’re already on a biologic:
- Don’t skip doses-even if you feel fine.
- Report any fever, cough, or skin changes right away.
- Keep your blood work appointments.
- If cost is a problem, talk to your pharmacist about biosimilars or assistance programs.
RA treatment isn’t one-size-fits-all. But it’s not random either. It’s science, strategy, and sometimes, survival. The right combination can mean years of mobility. The wrong one? It can mean irreversible damage. Talk to your rheumatologist. Ask questions. Push for answers. Your joints will thank you.




David Brooks
December 8, 2025Just got my biologic shot last week and I swear I can feel my fingers moving again. Like, actually moving. No more waking up with my hands glued shut. This stuff isn't magic, but damn if it isn't close. Keep going, warriors. You got this. 🙌💪
Jennifer Anderson
December 9, 2025sooo i started methotrexate last month and yeah it made me feel like a zombie for like 2 days but then i started taking folic acid and omg it’s a whole different vibe. also my dr said to drink like 3 liters of water a day and that helped too. not perfect but way better than before. 💕
Sadie Nastor
December 9, 2025i know it sounds crazy but i’ve been on the triple DMARD combo for 18 months now and my joints feel better than they have in years. no injections, no crazy costs, just pills i can swallow before coffee. i still get tired sometimes but i’m not crying in the shower anymore. also, i made a spreadsheet to track my symptoms. it’s weirdly satisfying. 📊❤️
Nicholas Heer
December 10, 2025THEY WANT YOU TO TAKE THESE DRUGS BECAUSE THE PHARMA COMPANIES OWN THE FDA. WHY DO YOU THINK THEY LET BIOLGICS COST 6K A MONTH? IT’S A SCAM. I’VE BEEN CURED BY CANNABIS OIL AND CRYOTHERAPY. THE SYSTEM IS DESIGNED TO KEEP YOU DEPENDENT. THEY DON’T WANT YOU HEALING. THEY WANT YOU PAYING. WATCH THE DOCUMENTARY ‘THE RA CONSPIRACY’.
Sangram Lavte
December 12, 2025In India, methotrexate costs less than $2 a month. Biosimilars are starting to appear, but still out of reach for most. We don’t have MRI machines in every clinic. We don’t have specialists everywhere. But we have people who still walk, still work, still care for their families-on cheap pills and sheer will. Respect to everyone fighting this fight, no matter the country.
Oliver Damon
December 12, 2025The real insight here isn’t just the pharmacology-it’s the epistemology of treatment. We’re moving from symptom management to systems-level intervention. The shift from ACR50 to imaging-based remission represents a paradigm shift in rheumatology: from patient-reported outcomes to objective, quantifiable biological endpoints. This isn’t just better medicine-it’s a redefinition of what ‘remission’ even means.
Kurt Russell
December 14, 2025LOOK. I was in a wheelchair in 2020. Now I hike. I play with my niece. I lift weights. I didn’t just get lucky-I followed the protocol. Methotrexate first. Folic acid daily. Biologic after 6 months. Blood tests every 8 weeks. No skipping. No excuses. You think this is hard? Try living with broken joints at 35. You can do this. I did. You will too. 💥
Stacy here
December 15, 2025They say ‘treat to target’ but what they really mean is ‘treat to profit.’ Biologics? Overpriced. JAK inhibitors? FDA black box warnings you won’t hear on TV. And don’t get me started on how they push methotrexate because it’s cheap, not because it’s best. The system is rigged. They want you dependent, not healed. Wake up. You’re being played.
Kyle Flores
December 16, 2025I had a bad reaction to the first biologic I tried-rash, fever, the whole thing. Switched to another one and now I’m good. But the real hero? My nurse. She walked me through every injection. Taught me how to store it right. Called me every month to check in. That human touch? That’s what kept me going. Medicine’s tech is great-but care is what heals.
Ryan Sullivan
December 17, 2025Let’s be honest: most of these patients are just chasing a placebo effect. Methotrexate? Overrated. Biologics? Overpriced. JAK inhibitors? Dangerous. The real treatment is acceptance. Stop fighting your body. Stop chasing remission. Live with the pain. It’s less expensive and statistically, you’ll live longer. This whole ‘cure’ narrative is a capitalist fantasy.
Wesley Phillips
December 19, 2025Okay so I’m on Rinvoq now and honestly it’s kinda wild how fast it works like I woke up one day and my knees didn’t sound like a rusty hinge? Mind blown. Also I don’t need shots? That’s basically the future right? Also I’m basically a genius for figuring this out myself
Olivia Hand
December 19, 2025I’ve been on methotrexate for 5 years. I’m in remission. But I’ve never had an MRI. My doctor says I’m fine. But what if I’m not? What if the damage is silent? How do we know when ‘feeling better’ is just adaptation? I need data. Not guesses. Where’s the science in that?
Desmond Khoo
December 21, 2025Just wanted to say-my mom’s on a biosimilar now and it cut her monthly bill from $5K to $3K. She cried. Not because she was sad. Because she could finally afford to buy groceries again. This isn’t just medicine. It’s dignity. Thank you for writing this. 🙏❤️
Louis Llaine
December 21, 2025So… you’re telling me the entire RA treatment algorithm is just ‘try methotrexate until you hate it, then try something that costs a mortgage payment’? Cool. Cool cool cool. And we wonder why people quit.
Jane Quitain
December 21, 2025i just started biologics and i was so scared but my nurse gave me this little sticker that says ‘i am brave’ and i put it on my injection pen and now i feel like a superhero. also i’m not gonna lie i cried the first time i did it myself. but i did it. 💪