Blood Thinners and Herbs: Risks, Interactions, and What You Need to Know
When you’re on blood thinners, medications that prevent dangerous clots by slowing down your blood’s ability to coagulate. Also known as anticoagulants, they’re prescribed for conditions like atrial fibrillation, deep vein thrombosis, or after a heart valve replacement. Many people don’t realize that what they eat or take as a supplement can turn a safe dose into a life-threatening one. herbs, natural plant-based products often used for health support. Also known as botanicals, they’re not regulated like drugs, but they can still change how your body handles medication. This isn’t theory—it’s a real, documented danger.
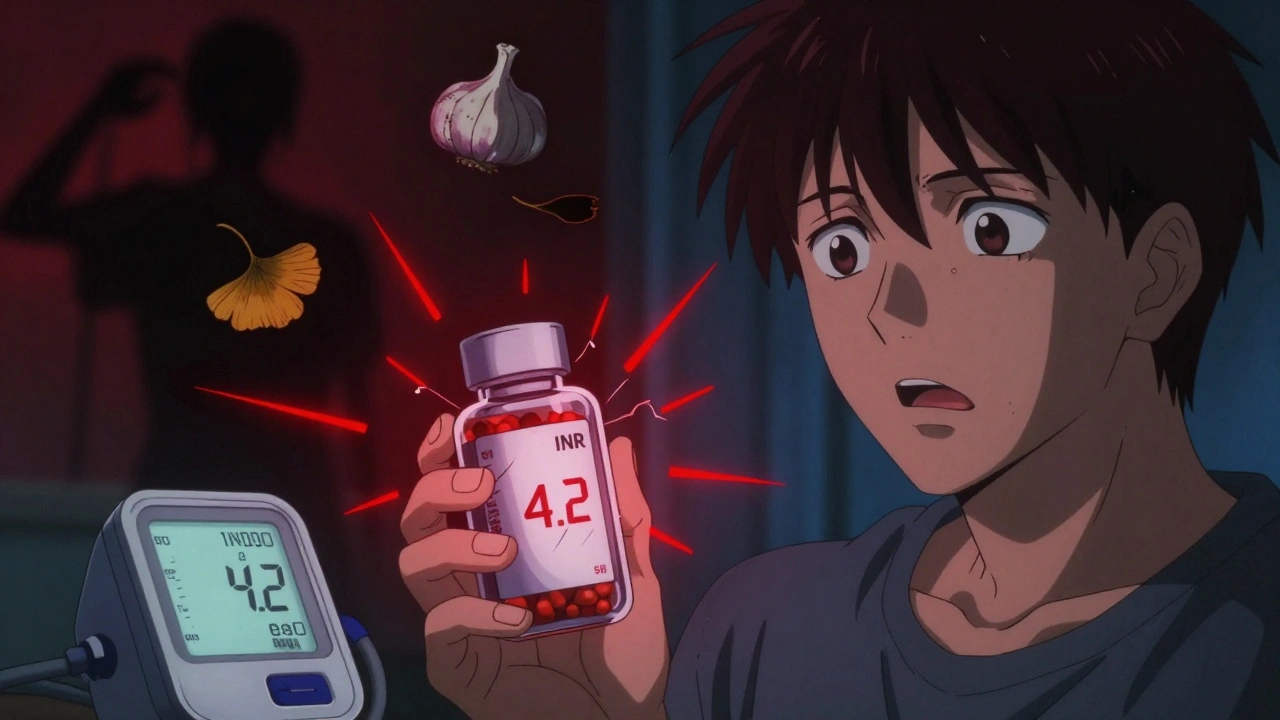
Take garlic, for example. It’s common in kitchens and supplements for heart health. But garlic can thin your blood even more than your prescription. One study showed people on warfarin who started taking garlic supplements had bleeding times that increased by over 30%. Same with ginger—popular for nausea and inflammation. It blocks platelet aggregation, just like aspirin. Combine that with a blood thinner, and you’re stacking effects you didn’t ask for. Even green tea, often seen as harmless, contains vitamin K in variable amounts. That can directly oppose the action of warfarin, making your INR levels swing unpredictably.
Then there’s ginkgo biloba. It’s marketed for memory and circulation, but it’s one of the most dangerous herbs to mix with anticoagulants. The FDA has received dozens of reports of brain bleeds and internal bleeding linked to ginkgo combined with blood thinners. St. John’s wort? It doesn’t thin blood directly, but it speeds up how fast your liver breaks down drugs like rivaroxaban and apixaban. That means the drug leaves your system too fast, leaving you unprotected from clots.
It’s not just about what you take—it’s about timing, dosage, and your body’s unique chemistry. Two people can take the same herb and the same dose of blood thinner, and one might bleed while the other doesn’t. Why? Genetics, liver function, even gut bacteria play a role. That’s why you can’t rely on internet advice or a pharmacist’s generic warning. You need to know exactly what’s in your supplements and tell your doctor every single thing you’re using.
And here’s the kicker: many people don’t even realize they’re taking something risky. A bottle labeled "natural" or "herbal blend" might contain multiple herbs you’ve never heard of. One person took a joint pain supplement that included turmeric, ginger, and cayenne—all blood-thinning herbs—and ended up in the ER after a minor fall. No one asked him what he was taking. He didn’t think it mattered.
That’s why the posts below matter. You’ll find real cases like how venlafaxine affects blood pressure and can complicate clotting risks, or how digoxin generics need careful monitoring because small changes in absorption can throw off your whole treatment. You’ll see how aspirin for heart health is no longer a blanket recommendation, and why PDE5 inhibitors like Viagra can crash your blood pressure when mixed with nitrates. These aren’t isolated issues—they’re all connected by the same principle: what you take doesn’t act alone.
Whether you’re on warfarin, Eliquis, Xarelto, or any other anticoagulant, your safety depends on knowing what to avoid. This isn’t about fear—it’s about control. You’re not giving up herbs or natural remedies. You’re learning how to use them without putting yourself at risk. Below, you’ll find practical, real-world advice from people who’ve been there, and the science that backs it up. No fluff. Just what you need to stay safe.