Every year, thousands of people on blood thinners end up in the emergency room-not because of a missed dose or a fall, but because they took something they thought was harmless: an herbal supplement. Turmeric. Garlic. Ginkgo. Green tea. These aren’t dangerous drugs. They’re sold in health food stores, labeled "natural," and often recommended by well-meaning friends or influencers. But when you’re on warfarin, apixaban, or rivaroxaban, "natural" doesn’t mean safe.
Why Herbal Supplements Can Be Dangerous with Blood Thinners
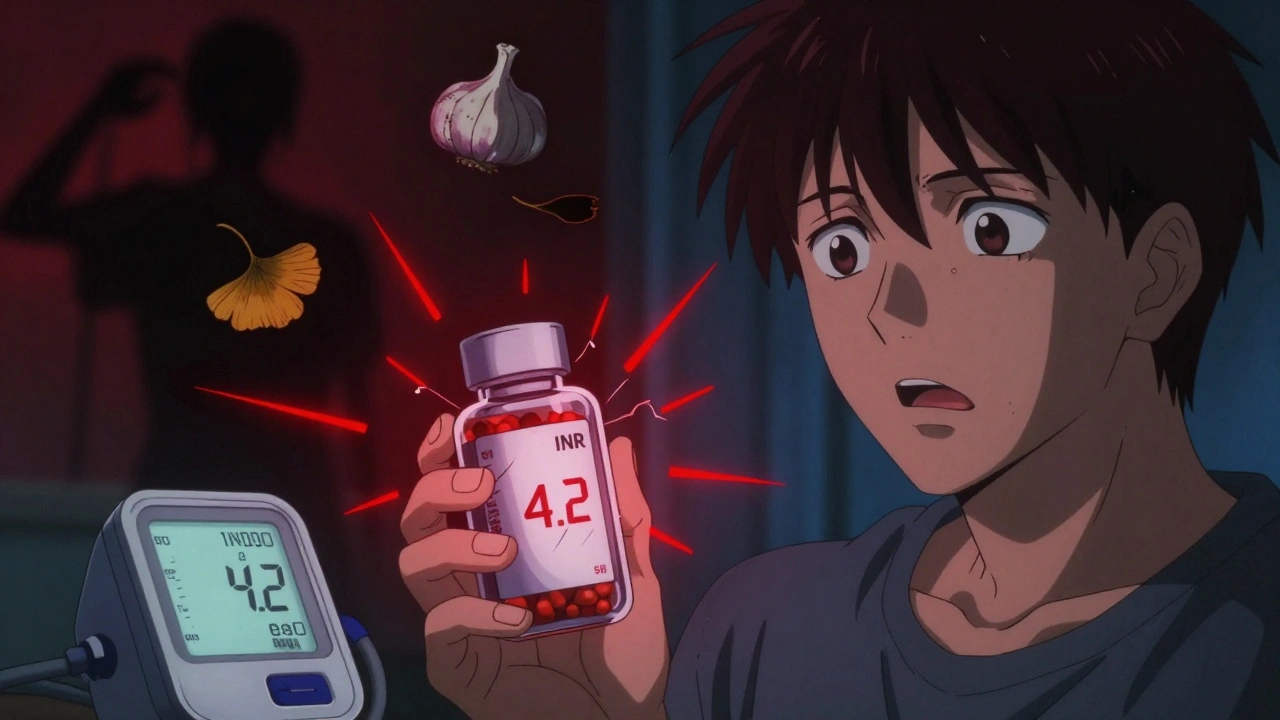
Blood thinners work by carefully balancing your body’s ability to clot. Too little, and you bleed. Too much, and you form clots. The margin for error is razor-thin. Warfarin, for example, has a target INR range of 2.0 to 3.0. A single spike above 4.0 can cause internal bleeding. A drop below 1.5 leaves you vulnerable to stroke. Herbal supplements don’t play by the same rules as prescription drugs. They’re not tested for interactions. They don’t come with warning labels. And worse-they often contain active compounds that directly interfere with how your body handles anticoagulants. There are two main ways this happens:- Pharmacokinetic interactions: Herbs change how your liver breaks down the drug. For example, St. John’s Wort speeds up the metabolism of apixaban, dropping its levels by half in just three days. That means the drug stops working-and your risk of clotting skyrockets.
- Pharmacodynamic interactions: Herbs amplify the drug’s effect. Ginkgo biloba inhibits platelet function. Garlic thins the blood. Danshen (a Chinese herb) can boost warfarin’s effect by 300-400%. That’s not a little extra thinning. That’s a hospital trip.
A 2024 FDA analysis of over 14,000 adverse events found that just 10 herbs-ginkgo, garlic, ginger, ginseng, St. John’s Wort, chamomile, cranberry, green tea, Chinese wolfberry, and dong quai-were responsible for nearly 70% of all serious cases. These aren’t rare outliers. They’re common.
The Top 5 Most Dangerous Herbal Supplements
Not all herbs are equal. Some are low risk. Others are ticking time bombs. Here are the five with the strongest evidence of danger:- Ginkgo biloba: The most common culprit. It blocks platelet-activating factor, making your blood less likely to clot. In 287 documented cases, it caused major bleeding when taken with warfarin or DOACs. One patient in Australia developed a brain hemorrhage after adding ginkgo to his daily routine for memory.
- Garlic: Not just in your pasta. Garlic supplements contain allicin, which inhibits platelet aggregation. A 2023 study showed 60% of patients taking more than 1,000 mg/day of garlic had INR levels rise above 4.0. Even a single clove of raw garlic daily can cause issues.
- Ginseng: It’s in energy drinks, teas, and tonics. But ginseng can either increase or decrease INR unpredictably. One patient saw his INR jump from 2.8 to 5.1 after taking a ginseng supplement for three weeks. Another saw it drop to 1.2-putting him at risk for stroke.
- St. John’s Wort: This one’s sneaky. It doesn’t make you bleed more. It makes your blood thinner less effective. It triggers liver enzymes that flush out apixaban and rivaroxaban. Within days, your protection vanishes. A 2021 clinical trial showed apixaban levels fell by 50% after just 72 hours of St. John’s Wort use.
- Danshen (Salvia miltiorrhiza): A cornerstone of traditional Chinese medicine. It’s sold as a heart health supplement. But in 12 documented cases across five countries, it caused INR spikes so severe that patients needed transfusions. It’s not just risky-it’s deadly.
What About "Safe" Herbs Like Turmeric or Ginger?
You’ve probably heard turmeric is anti-inflammatory and ginger helps digestion. Both are popular. But here’s the truth: they’re not safe if you’re on a blood thinner. Turmeric contains curcumin, which inhibits platelet aggregation. A Reddit user in Melbourne posted about his INR rising to 4.2 after adding turmeric capsules to his morning routine. He ended up in the hospital with a gastrointestinal bleed. He didn’t know it was the turmeric. His doctor didn’t ask. Ginger is trickier. Low doses-under 1 gram per day-may be okay for some people under close monitoring. One study on PatientsLikeMe found 28% of users maintained stable INR with small amounts. But that’s not a green light. It’s a caution sign. Dose matters. Timing matters. And most people don’t know how much they’re actually taking. A ginger tea bag can contain 500 mg. A capsule can have 1,000 mg. You’re not in control.
Why Doctors Don’t Always Ask
You’d think your doctor would know. But here’s the uncomfortable truth: most don’t ask. A 2024 Medscape survey of 1,247 patients on anticoagulants found that 69% took herbal supplements without telling their doctors. Why? Because they assumed:- "Natural" means safe.
- "It’s just a supplement. It’s not medicine."
- "My doctor only cares about my pills."
And doctors? They’re busy. They ask about prescriptions. They rarely ask about supplements. A 2022 study showed that while 89% of doctors asked about prescription drugs, only 37% asked about herbal products. And only 27% documented the answers in the chart.
This isn’t negligence. It’s systemic. Medical training barely covers herbal interactions. Pharmacies don’t flag them. Insurance doesn’t pay for screening tools. So the gap stays wide.
What You Can Do Right Now
You don’t need to quit all supplements. You need to be smart.- Make a list. Write down every pill, powder, tea, or tincture you take-even if you think it’s "just for sleep" or "for joint pain." Include brands and doses.
- Bring it to every appointment. Don’t wait for your doctor to ask. Hand them the list. Say: "I’m on a blood thinner. Are any of these dangerous?"
- Check the Natural Medicines Database. It’s the gold standard. It rates interactions on a 1-7 scale. Level 7 = life-threatening. Ginkgo? Level 7. Garlic? Level 6. St. John’s Wort? Level 7. You can access it through many hospital systems or ask your pharmacist for a printout.
- Don’t start anything new without checking. Even if it’s "organic" or "FDA-approved" (it’s not-supplements don’t need FDA approval before sale).
- Track your INR. If you’re on warfarin, know your numbers. A sudden jump? Look at what changed in the last 3-5 days. A new supplement? That’s your first suspect.

New Tools Are Coming-But Don’t Wait
There’s hope. In 2025, the FDA started requiring all anticoagulant prescriptions to include a standardized herbal interaction checklist. In Europe, AI tools like MedCheck AI are being rolled out in clinics with 92% accuracy in flagging dangerous combos. But these aren’t magic. They’re tools. They only work if you tell your doctor what you’re taking. Genetic testing for CYP2C9 and VKORC1 genes can now predict how you’ll respond to warfarin-and whether herbs will push you over the edge. It’s available in Australia and the U.S. But only 12% of patients on anticoagulants have been tested. Why? Because most doctors don’t know it exists.What About Newer Blood Thinners Like Apixaban?
Yes, newer drugs like apixaban, dabigatran, and rivaroxaban have fewer interactions than warfarin. But they’re not immune. St. John’s Wort still slashes apixaban levels by half. Ginkgo still increases bleeding risk. Green tea can interfere with absorption. Even CBD oil-now sold everywhere-has been shown in a 2024 JAMA trial to increase INR by 2.8 times in nearly 70% of warfarin users. The idea that "newer = safer" is misleading. It’s more accurate to say: "newer = less studied." And that’s dangerous.Final Reality Check
You’re not alone. Over 47% of Americans over 65 take a blood thinner. Nearly half of them also take herbal supplements. The number is rising fast. The problem isn’t the herbs. It’s the silence around them. Your health isn’t a gamble. You don’t have to choose between natural remedies and safety. You just need to speak up. Ask your doctor. Ask your pharmacist. Ask again. And if you’re taking anything herbal while on a blood thinner-stop. Wait. Check. Then decide. Because in this case, "natural" doesn’t mean gentle. It means unpredictable. And unpredictability kills.Can I take turmeric if I’m on warfarin?
No-not safely. Turmeric contains curcumin, which can increase your INR and raise your risk of bleeding. At least 12 documented cases show INR levels spiking above 4.0 after starting turmeric supplements. Even small amounts can be dangerous. If you want to use turmeric for inflammation, talk to your doctor first. Never start it without checking your INR and monitoring closely.
Is ginger safe with blood thinners?
Low doses (under 1 gram per day) may be tolerated by some people under strict medical supervision, but it’s not risk-free. Ginger can inhibit platelet function and increase bleeding time. A 2023 study found that 30% of patients taking ginger supplements experienced INR rises above the target range. Avoid ginger supplements entirely. If you eat fresh ginger in food, keep it consistent-don’t suddenly eat a lot one day and none the next.
Does St. John’s Wort affect all blood thinners?
Yes, especially apixaban, rivaroxaban, and dabigatran. St. John’s Wort activates liver enzymes that break down these drugs too quickly, reducing their levels by up to 50% in just three days. This leaves you unprotected against clots. Even if you’ve been on the same dose for years, adding St. John’s Wort can cause a stroke. Avoid it completely if you’re on any direct oral anticoagulant (DOAC).
Can I use CBD oil with my blood thinner?
No. A 2024 clinical trial found that CBD oil increased INR by 2.8 times in 68% of patients taking warfarin. It blocks the liver enzymes that metabolize warfarin, causing dangerous buildup. Even topical CBD products may be absorbed enough to cause issues. If you’re using CBD for pain or anxiety, stop it immediately and get your INR checked. There is no safe dose established yet.
What should I do if I accidentally took a risky herb?
Stop taking the supplement immediately. Contact your doctor or pharmacist right away. If you’re on warfarin, get an INR test within 24-48 hours. Watch for signs of bleeding: unusual bruising, nosebleeds, blood in urine or stool, severe headaches, or dizziness. If you have any of these, go to the ER. Don’t wait. The longer you wait, the higher the risk of serious bleeding.
Are there any herbs that are safe with blood thinners?
There’s no definitive list of "safe" herbs for people on anticoagulants. Even herbs like chamomile or licorice have been linked to interactions in rare cases. The safest approach is to avoid all herbal supplements unless your doctor or pharmacist has reviewed them individually. Vitamins like vitamin K (in consistent amounts) and vitamin D are generally fine, but always check with your provider before starting anything.
How often should I get my INR checked if I’m on supplements?
If you’re taking any herbal supplement while on warfarin, you should get your INR checked every 1-2 weeks for the first month after starting the supplement. After that, continue checking every 2-4 weeks. If you stop the supplement, check your INR again within 5-7 days. For DOACs like apixaban, INR isn’t used-but if you’re taking something that affects liver enzymes, your doctor may order blood tests to check drug levels.



Arun kumar
December 3, 2025man i just started taking garlic pills for my cold and didn't even think twice
now i'm reading this and my stomach dropped
why does no one talk about this? i'm gonna stop tomorrow and call my doc
Alicia Marks
December 3, 2025Thank you for posting this. So many people don't realize supplements aren't harmless. You're doing important work.
Shannara Jenkins
December 4, 2025My grandma took ginkgo for memory and ended up in the ER with a brain bleed. She never told her doctor. I wish I'd known sooner.
Now I make sure everyone in my family knows: if you're on blood thinners, skip the herbal stuff unless your pharmacist says it's okay.
Jay Everett
December 6, 2025Bro. St. John’s Wort is the silent assassin of anticoagulants. I saw a guy on Reddit who was on apixaban, started it for depression, and two weeks later had a pulmonary embolism. He thought it was "just herbal."
It’s not. It’s a metabolic grenade. 🚨
And CBD? Don’t even get me started. That stuff is like pouring gasoline on your INR. Stop. Just stop.
Steve Enck
December 7, 2025While the anecdotal evidence presented here is compelling, the methodological rigor is severely lacking. The reliance on case reports and uncontrolled observational data from platforms like Reddit undermines the scientific validity of the claims. Without controlled trials, peer-reviewed meta-analyses, or pharmacokinetic modeling across diverse populations, this constitutes alarmist speculation masquerading as clinical guidance. The conflation of pharmacodynamic effects with clinical outcomes is particularly egregious. One must exercise extreme caution before converting anecdotal correlations into population-wide prohibitions.
Laura Baur
December 8, 2025You think this is bad? Try telling a 72-year-old diabetic with arthritis that she can't take turmeric because it "might" increase bleeding risk. She’s been taking it for 15 years. Her joints don’t ache anymore. Her doctor doesn’t ask. Her pharmacist doesn’t flag it. The FDA doesn’t regulate it. And now you want her to stop because of a 2024 FDA analysis? That’s not safety. That’s medical paternalism wrapped in a lab coat.
There’s a difference between risk and harm. Risk is statistical. Harm is personal. She’s lived longer with turmeric than she has with warfarin. You want to take that away from her because of a 0.8% chance of INR crossing 4.0? Where’s the compassion? Where’s the shared decision-making? You’re not protecting people. You’re infantilizing them.
And let’s be real-how many doctors even know what CYP2C9 does? If your provider can’t explain how your liver metabolizes drugs, why are they the one deciding what you can and can’t take? You’re not empowering patients. You’re replacing one form of ignorance with another.
Let people make informed choices. Give them the data. Don’t scare them into compliance. That’s not healthcare. That’s fearmongering dressed as education.
ATUL BHARDWAJ
December 9, 2025in india we use ashwagandha for stress
no one ever says anything
but now i think i will ask my doctor
thank you
मनोज कुमार
December 10, 2025the whole post is just fear porn
ginkgo bad garlic bad st johns bad cbd bad
where are the numbers
how many deaths
how many cases
no stats no context just scare tactics
and you expect people to believe this? lol
Jack Dao
December 12, 2025People who take supplements while on anticoagulants are either dangerously naive or actively reckless. This isn’t a gray area. It’s a red zone. If you can’t follow basic safety protocols-like disclosing everything you ingest to your provider-you don’t deserve to be trusted with your own health. You’re not just risking yourself. You’re overloading the system with preventable ER visits. This isn’t about natural vs synthetic. It’s about responsibility. And you’re failing.
Zed theMartian
December 13, 2025Oh wow. So turmeric is now the new nicotine? Garlic is the new cigarettes? I can't believe I trusted my grandma's herbal tea recipe. Next you'll tell me sunlight causes bleeding because it 'boosts circulation.'
Let me guess-next article: 'Why Breathing Might Interfere With Your DOACs.'
Look, I'm not saying herbs are magic. But this is the same panic that led to the 1990s 'vitamin overdose hysteria.' You're turning wellness into witchcraft. The real danger isn't ginkgo-it's the cult of medical absolutism that treats every herb like a poison. I'll take my chances with nature over a pharmaceutical cartel any day.