Bioavailability: What It Means for Your Medications and Why It Matters
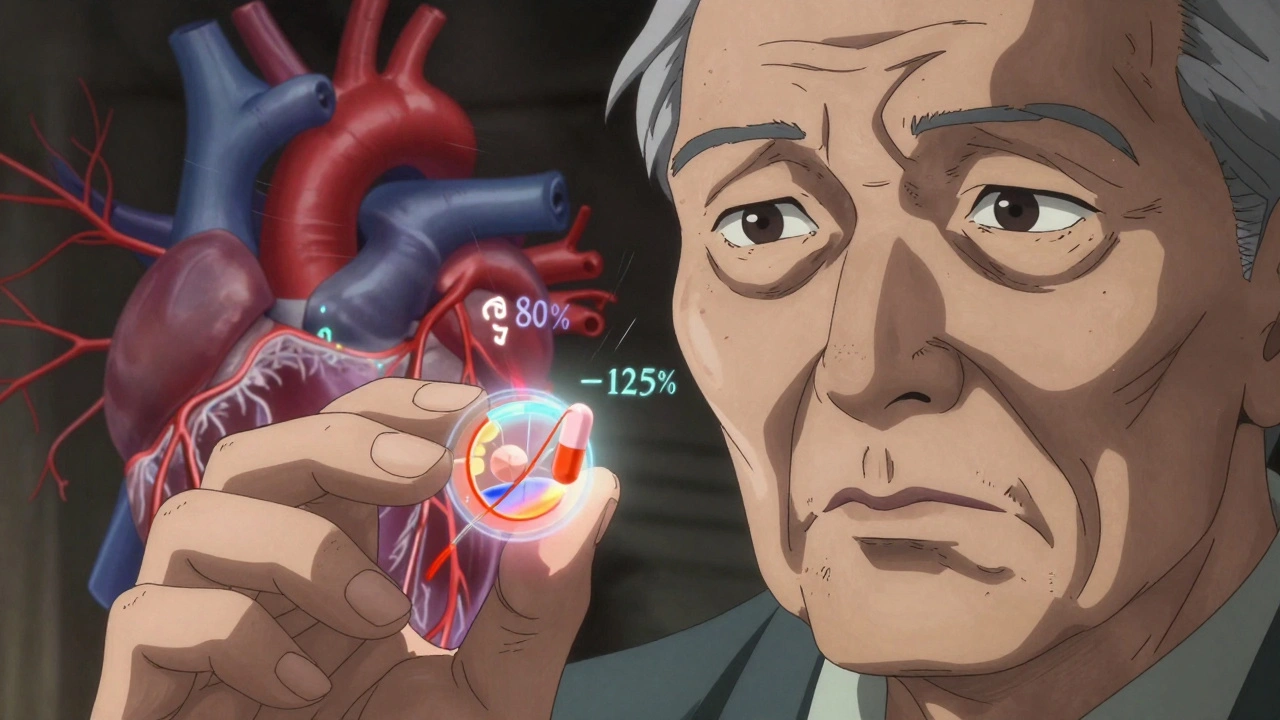
When you take a pill, not all of it actually makes it into your bloodstream—that’s where bioavailability, the portion of a drug that enters circulation and has an active effect. Also known as drug absorption, it determines whether your medicine works as expected or falls short. Two people taking the same dose of the same drug can have totally different results, not because one is "stronger," but because of bioavailability.
It’s not just about the pill you swallow. Bioavailability changes based on how your body handles the drug—whether it’s broken down by stomach acid, filtered by your liver before reaching your blood, or absorbed slowly because of what you ate. That’s why some generics work fine for you while others don’t. It’s also why a drug taken on an empty stomach might hit harder than one taken with food. This isn’t magic—it’s pharmacokinetics, how your body moves a drug through absorption, distribution, metabolism, and excretion. And if you’re on something like Xanax or a blood thinner, even small drops in bioavailability can mean the difference between control and crisis.
Some medications are designed to bypass these issues—sublingual strips, patches, or injections—because their makers know bioavailability matters. That’s why Tastylia OD Strip works faster than a swallowed tablet, or why the Emsam patch avoids first-pass liver breakdown. Meanwhile, drugs like linezolid or venlafaxine demand strict dosing because their bioavailability shifts with diet or other meds. Even something as simple as grapefruit juice can wreck your bioavailability by blocking enzymes your liver needs to process drugs.
When you see posts about duplicate medications, generic vs brand-name differences, or how family genes affect drug response, they’re all connected to this one thing: bioavailability. If your body doesn’t absorb the drug properly, nothing else matters. You might be taking the right medicine at the right dose, but if bioavailability is low, you’re not getting the benefit. That’s why checking your meds with your pharmacist isn’t just smart—it’s essential.
Below, you’ll find real-world examples of how bioavailability plays out in daily treatment—from insulin stacking and anticoagulant interactions to why some people react badly to generics. These aren’t theory pieces. They’re stories of what happens when bioavailability gets ignored, misunderstood, or mishandled. And they’re here to help you avoid the same mistakes.