
Linezolid-Tyramine Safety Calculator
Tyramine Safety Calculator
Calculate tyramine content in your meal to stay under the 100mg safety limit while taking linezolid. Exceeding this threshold can cause dangerous blood pressure spikes.
Total Tyramine: 0mg
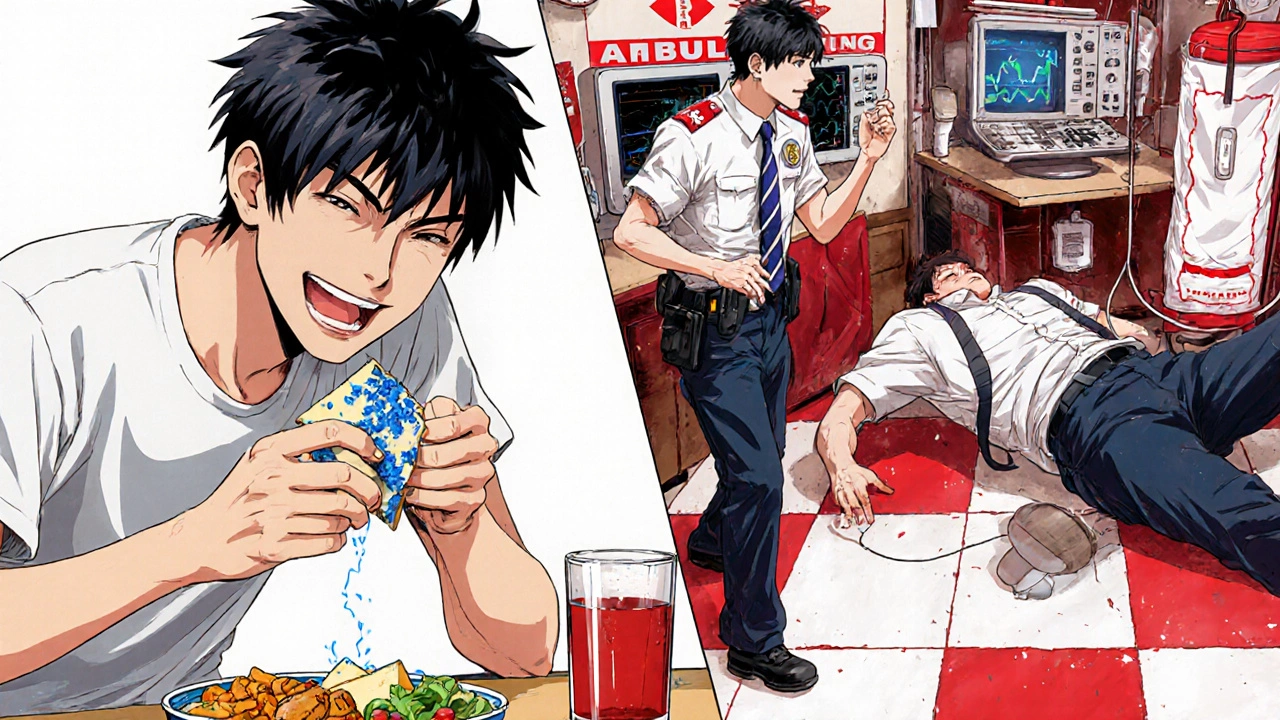
When you're prescribed linezolid for a stubborn bacterial infection - maybe MRSA or a resistant Enterococcus - your doctor focuses on killing the bug. But there's another enemy hiding in plain sight: your lunch. A slice of aged cheddar, a glass of red wine, or even leftover sausage could trigger a blood pressure spike so dangerous it lands you in the ICU. This isn't a myth. It's a documented, life-threatening interaction between linezolid and tyramine, and it's happening more often than you think.
Why Linezolid Isn't Just Another Antibiotic
Linezolid is a powerful antibiotic used when other drugs fail. It was approved in 2000 to fight superbugs like MRSA and VRE. But unlike most antibiotics that target cell walls or protein building blocks, linezolid works by jamming bacterial protein synthesis at the very start. That’s why it’s so effective against resistant strains. But here’s the catch: linezolid also weakly blocks your body’s own enzymes - monoamine oxidase A and B (MAO-A and MAO-B). These enzymes normally break down tyramine, a natural compound found in aged, fermented, or spoiled foods. When MAO is inhibited, tyramine builds up in your bloodstream. That triggers a flood of norepinephrine, which can send your blood pressure skyrocketing. This isn’t theoretical. In 2021, researchers reviewed 17 cases of linezolid-induced hypertensive crises. The average systolic blood pressure at admission? 212 mmHg. Some hit 248. That’s higher than the pressure in a car tire. One patient, after eating blue cheese while on linezolid, needed ICU care for three days. His blood pressure didn’t drop until he stopped the drug - and even then, it took 26 days to fully return to normal.What Foods Are Dangerous?
You don’t need to avoid every food with tyramine. But you must avoid the ones with more than 100mg per serving. Here’s what’s on the danger list:- Aged cheeses: Blue cheese (900-1,500mg/100g), cheddar (150mg/oz), parmesan, gouda, Swiss, brie, and camembert. Even a small wedge can push you over the limit.
- Fermented soy: Soy sauce, miso, tempeh, and fermented tofu. A tablespoon of soy sauce can contain 100mg or more.
- Tap beer and draft beer: Up to 200mg per 100ml. Bottled or canned beer is usually safer, but check labels - some craft brews are high.
- Red wine: 5-100mg per 100ml. White wine and champagne are lower risk.
- Dried or cured meats: Salami, pepperoni, liverwurst, and air-dried sausages. Even leftovers stored too long can develop dangerous levels.
- Overripe or spoiled foods: Any fruit or vegetable left too long can start fermenting. A banana with brown spots? Skip it.
- Yeast extracts: Marmite, Vegemite, and similar spreads. One teaspoon can have 50-100mg.
And here’s the sneaky part: it’s not just about what you eat - it’s about how it’s stored. Aged cheese in a proper fridge? Fine. That same cheese left on the counter for a week? Dangerous. Leftover stew in the fridge for five days? Potentially toxic.
How Much Is Too Much?
The FDA and Infectious Diseases Society of America agree: avoid foods with more than 100mg of tyramine. But recent NIH research suggests the real threshold might be lower - as low as 50mg - for some people. Why? Because sensitivity varies. A 2006 study at the University of Toronto showed that linezolid produces about 85% of the tyramine pressor effect seen with moclobemide, a known MAO inhibitor. That’s not weak. That’s clinically significant. And body weight matters. People with higher BMI showed greater tyramine sensitivity. Age, liver function, and even genetics play a role. You might be fine with a bit of salami. The person next to you could have a stroke. That’s why blanket advice like “just avoid cheese” isn’t enough. You need specifics. One ounce of aged cheddar = 150mg tyramine. One cup of tap beer = 200mg. One tablespoon of soy sauce = 100mg. Write those numbers down. Keep them in your wallet.When Do You Start and Stop the Diet?
This isn’t a lifelong restriction. But it’s not optional while you’re on the drug.- Start the diet 24 hours before your first dose. Tyramine builds up fast.
- Continue for at least 14 days after your last dose. Linezolid’s effect on MAO enzymes lasts longer than the drug stays in your blood. It takes time for your body to rebuild new enzymes.
- Some hospitals, like UCSF, recommend 14 days post-treatment. Others say 7. Stick with the longer window. It’s safer.
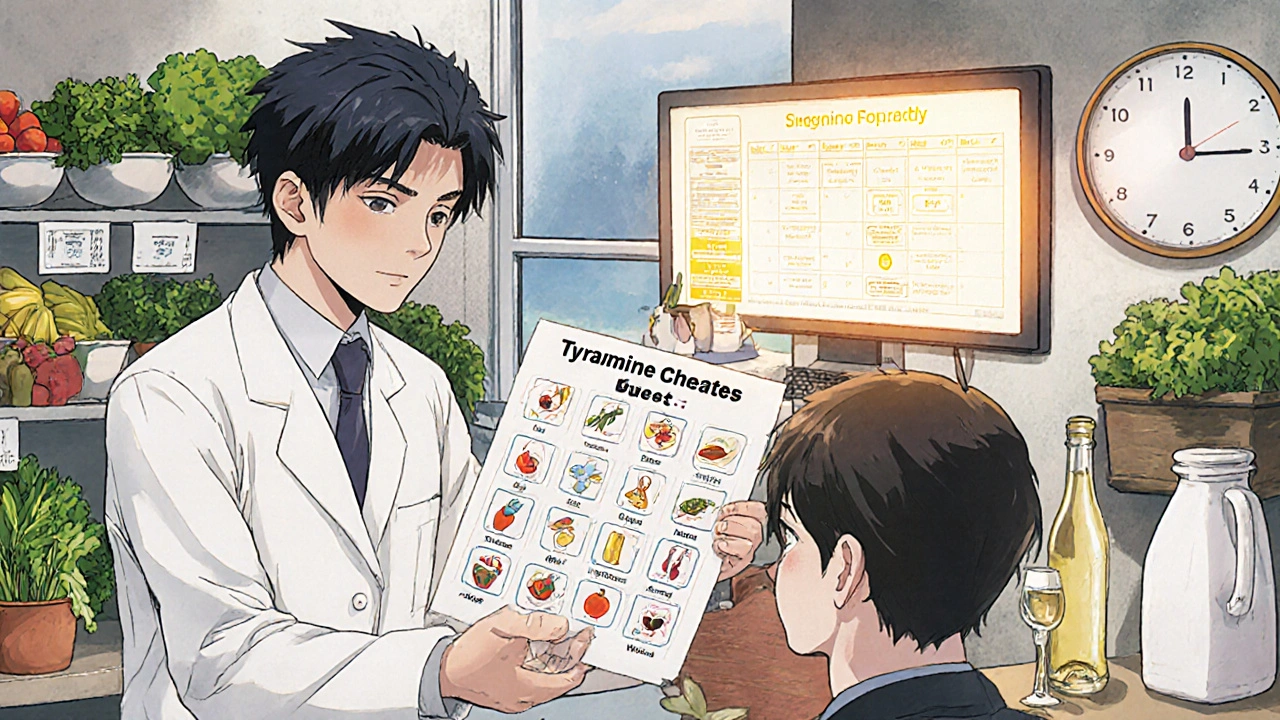
Don’t assume your doctor told you this. A 2022 study found only 43.7% of patients received written dietary instructions. That’s not good enough. Ask for a handout. Ask for a dietitian. If your pharmacy doesn’t give you one, request it.
What About Other Medications?
Linezolid doesn’t just clash with food. It clashes with other drugs too.- Serotonin boosters: SSRIs, SNRIs, tramadol, dextromethorphan. Combine these with linezolid and you risk serotonin syndrome - a potentially fatal condition with high fever, seizures, and muscle rigidity.
- Decongestants: Pseudoephedrine, phenylephrine. These can double your blood pressure when MAO is blocked.
- Dopamine agonists: Used for Parkinson’s. Linezolid can turn them into a dangerous cocktail.
- Stimulants: Adderall, Ritalin. Avoid them completely.
Always give your pharmacist your full medication list - including over-the-counter and supplements. Even herbal products like St. John’s Wort can interact. Don’t assume they’re safe just because they’re natural.
What If You Accidentally Eat Something?
If you eat a slice of blue cheese or drink a pint of draft beer while on linezolid, don’t panic - but act fast.- Check your blood pressure immediately if you have a home monitor.
- Watch for symptoms: severe headache, chest pain, rapid heartbeat, blurred vision, nausea, sweating.
- If your systolic pressure is over 180 or you feel unwell, go to the ER. Don’t wait. Don’t call your doctor first. Go.
There’s no antidote. Treatment is supportive: IV antihypertensives, monitoring, and stopping linezolid. The sooner you get help, the better your outcome.
Who’s at Highest Risk?
Not everyone who eats tyramine while on linezolid has a crisis. But some people are far more vulnerable:- People with pre-existing high blood pressure
- Those over 65
- People with kidney or liver disease
- Patients on prolonged linezolid therapy (more than 2 weeks)
- Those taking other medications that raise blood pressure or serotonin
Even if you’re young and healthy, don’t gamble. The risk might be low - but the consequence is catastrophic. Three documented deaths since 2018 weren’t accidents. They were preventable.
How to Stay Safe - Practical Tips
You don’t need to starve. You just need to be smart.- Use a tyramine cheat sheet. Print one from your hospital’s pharmacy website. Keep it in your kitchen.
- When in doubt, throw it out. If food looks, smells, or tastes off - don’t risk it.
- Choose fresh over aged. Fresh chicken, plain yogurt, milk, and raw vegetables are safe.
- Stick to bottled beer, white wine, or non-alcoholic options.
- Ask your pharmacist for a list of safe alternatives. They’ve seen this before.
- Use your phone. Take a picture of your meal before you eat it. If you’re unsure, send it to your pharmacist.
- Ask for an electronic alert in your medical record. Many hospitals now flag linezolid prescriptions with pop-up warnings for pharmacists.
And if you’re on linezolid for more than two weeks - insist on seeing a dietitian. Nutrition matters. You can still eat well. You just need guidance.
The Future: New Antibiotics Without the Risk
Linezolid has saved lives. But its MAO inhibition is a flaw we’ve learned to manage - not ignore. A new antibiotic, contezolid (MRX-I), is in Phase III trials and expected to be submitted to the FDA in mid-2025. It kills the same superbugs - without touching MAO enzymes. That means no tyramine restrictions. No blood pressure spikes. No ICU stays. But until then, linezolid remains a critical tool. And with antibiotic resistance rising, we’ll keep using it. That means we must use it safely.Bottom Line
Linezolid isn’t dangerous because it’s a bad drug. It’s dangerous because we treat it like a regular antibiotic. It’s not. It’s a weak MAO inhibitor with real, life-threatening dietary risks. You can’t just take it and hope for the best. Know the foods. Know the timeline. Know the symptoms. Ask for help. Write it down. Share it with your family. This isn’t about being perfect. It’s about being informed. One wrong bite can change everything - but one smart choice can save your life.Can I drink wine while taking linezolid?
Red wine contains 5-100mg of tyramine per 100ml. A single glass could push you over the 100mg safety limit, especially if you’ve eaten other tyramine-rich foods. White wine and champagne are lower in tyramine and generally safer in small amounts, but it’s best to avoid all alcohol while on linezolid. If you do drink, limit it to one small glass of white wine and check your blood pressure afterward.
Is it safe to eat cheese if it’s not aged?
Yes. Fresh cheeses like ricotta, cottage cheese, mozzarella, cream cheese, and mascarpone are low in tyramine and safe to eat. Avoid any cheese that’s been stored for weeks, has mold, or is labeled “aged,” “sharp,” or “blue.” If you’re unsure, ask the deli counter - fresh mozzarella is fine. Parmesan that’s been aged for 18 months? Skip it.
How long does linezolid stay in my system?
Linezolid’s half-life is about 5 hours, meaning most of it leaves your blood within a day. But its effect on MAO enzymes lasts much longer. Your body needs time to produce new enzymes - typically 10 to 14 days. That’s why dietary restrictions continue for two weeks after your last dose. Stopping the drug doesn’t instantly undo the inhibition.
Can I take linezolid if I have high blood pressure?
Yes - but with extreme caution. The 2024 IDSA guidelines recommend checking your blood pressure before starting linezolid and monitoring it twice daily during treatment. If your blood pressure is already elevated, your doctor may choose a different antibiotic. If linezolid is necessary, strict dietary control and close monitoring are non-negotiable. Don’t assume you can manage it on your own.
What should I do if I forget and eat something risky?
Don’t wait for symptoms. Check your blood pressure right away. If it’s above 180/120, or if you feel dizzy, have a headache, chest pain, or blurred vision, go to the emergency room immediately. Don’t call your doctor first - go. There’s no home remedy. The only treatment is stopping linezolid and using IV medications to lower your blood pressure. Delaying care can be fatal.
Are there any safe alternatives to linezolid?
Yes - but only if your infection allows it. For MRSA, alternatives include daptomycin, vancomycin, or ceftaroline. For VRE, options include daptomycin or tigecycline. But not all infections respond to these. Linezolid is often the last effective option. Your doctor will weigh the risks: the danger of the infection versus the risk of dietary restrictions. Never refuse linezolid without discussing alternatives - but always insist on full education about tyramine.
Why do some people say they ate cheese and had no problem?
Some people do tolerate small amounts of tyramine without symptoms. But that doesn’t mean it’s safe. Individual sensitivity varies based on genetics, liver function, BMI, and other medications. One person might eat blue cheese with no issue. Another - even with the same dose - could have a stroke. Anecdotes aren’t evidence. The data shows clear, documented cases of death. That’s why guidelines are strict: to protect everyone, not just the most sensitive.



Rachel Villegas
November 22, 2025Just got prescribed linezolid yesterday. I’m printing out that tyramine cheat sheet and taping it to my fridge. No more blue cheese for me - I loved it, but not enough to end up in the ICU. Thanks for the clarity.
Also, I’m showing this to my mom. She’s the one who always insists on ‘just one bite’ of everything. Not this time.
prasad gaude
November 24, 2025Man, this hits different. In India, we don’t think of cheese as dangerous - we eat paneer daily. But then again, we don’t age it for months like they do in Europe. This is a global health blind spot. Your body doesn’t care where you’re from - MAO inhibition doesn’t respect borders.
Also, I just remembered my uncle had a stroke after eating leftover sausage while on antibiotics. No one connected the dots. We need public awareness campaigns, not just pharmacy flyers.
Leisha Haynes
November 25, 2025So let me get this straight - I can’t have wine, cheese, soy sauce, or leftover pizza from Tuesday? What am I supposed to eat? Boiled water and regret?
Also, why is the FDA okay with letting this drug exist without a mandatory warning label on the bottle? This isn’t a side effect - it’s a landmine.
And don’t even get me started on the ‘ask your pharmacist’ advice. Half the time they’re too busy ringing up cough syrup to care.
Elise Lakey
November 27, 2025Thank you for writing this. I’ve been on linezolid for 10 days and I’ve been terrified to eat anything. I didn’t know fresh mozzarella was safe - I thought all cheese was off-limits. This list saved me from a lot of unnecessary stress.
Also, I took a photo of my lunch every day and sent it to my pharmacist. She replied every time. That tiny bit of human connection made me feel less alone.
Patricia McElhinney
November 27, 2025It is imperative to underscore that the failure of primary care providers to adequately counsel patients on monoamine oxidase inhibition constitutes a systemic breach of the standard of care. The prevalence of non-compliance is not attributable to patient negligence alone - it is a direct consequence of institutional negligence. The FDA’s labeling requirements remain woefully inadequate. A black box warning is not sufficient when the risk is both quantifiable and catastrophic.
Furthermore, the anecdotal tolerance cited by laypersons does not negate the statistical probability of adverse events - a fallacy of composition. This is not a matter of personal liberty; it is a matter of public health ethics.
Archana Jha
November 28, 2025Wait - so this is why my cousin died after a 'little bit' of cheddar? They said it was a 'stroke' - but no one said it was the antibiotic? I’m starting to think this whole thing is being hidden. Big Pharma doesn’t want you to know how dangerous their drugs are. They profit from ICU stays.
And why are they still selling linezolid? There’s gotta be a cover-up. They’ve been doing this for years. They know. They just don’t care.
Josh Zubkoff
November 29, 2025Okay, so let’s break this down. You’re telling me that if I eat a sandwich with aged cheddar and soy sauce on it, while drinking a craft IPA and eating a banana with brown spots, I’m basically playing Russian roulette with my brain? And the only way to know if I’m safe is to check my blood pressure every hour?
And yet, I’m supposed to trust my doctor who prescribed this without even mentioning any of this? I mean, come on. This isn’t medicine - it’s a horror show with a prescription pad.
And don’t even get me started on the ‘14-day wait’ after the last pill. That’s longer than my last relationship. I’m gonna be paranoid for months. My therapist is gonna need a raise.
Amy Hutchinson
December 1, 2025My mom took linezolid and ate a slice of salami. She didn’t say anything until her head felt like it was going to explode. We rushed her to the ER - they had to hook her up to a drip for 12 hours. She’s fine now but she won’t eat anything that’s been in the fridge longer than 2 days.
Now she’s sending me pics of every meal. I’m not even allowed to order sushi anymore because ‘wasabi might be fermented.’ I love her but I miss tacos.
Sharley Agarwal
December 3, 2025Typical. Another post full of fear-mongering. People die from falling in the shower. Should we ban showers?
My aunt took linezolid and ate blue cheese. Nothing happened. You’re scaring people for clicks. Just take the pill and stop overthinking.
Dolapo Eniola
December 5, 2025Bro, in Nigeria we don’t even know what ‘aged cheese’ is. We eat fresh shaki and pap. But I saw this post and I’m like - this is why Western medicine is so extra. You people make a drug that works and then act like it’s a bomb.
My cousin took this in Lagos, ate pepper soup with fermented beans - no problem. You guys need to chill. Your bodies are too soft.
Arup Kuri
December 5, 2025Why do people always act like this is new? MAO inhibitors have been a thing since the 60s. We used to have to avoid bananas and beer back then. Now we just pretend we’re smarter because we have Google.
Doctors don’t care. Pharmacies don’t care. You think they’re gonna stop selling linezolid because some blog post scared you? Wake up.
Just don’t eat anything that looks like it’s been through a war.
Roscoe Howard
December 6, 2025While the author presents a compelling case regarding the pharmacodynamic implications of linezolid-induced MAO inhibition, the underlying assumption that dietary compliance is a viable public health strategy is empirically dubious. The cognitive load required to maintain a tyramine-restricted diet - particularly among elderly, low-literacy, or economically disadvantaged populations - renders this intervention inherently inequitable. A more ethical approach would be to develop and deploy MAO-sparing analogs - not to burden patients with behavioral constraints that are neither scalable nor sustainable.
Furthermore, the reliance on self-reported blood pressure monitoring introduces significant measurement bias. The notion that a layperson can accurately diagnose a hypertensive crisis without clinical context is not merely misguided - it is dangerous.
Jennifer Griffith
December 6, 2025Wait so no soy sauce? But that’s like… everything? I just ordered pho for lunch. I’m gonna die. I didn’t even know soy sauce had tyramine. I thought it was just salt.
Also, I think the guy who wrote this is just trying to sell a diet plan. Why does he care so much about cheese?
Agastya Shukla
December 6, 2025As a pharmacologist, I appreciate the precision here. The 85% MAO inhibition equivalence to moclobemide is critical - it’s not a ‘mild’ effect. The 100mg threshold is outdated; recent studies show 50mg can trigger pressor response in CYP2D6 poor metabolizers.
Also, the 14-day post-treatment window is conservative but necessary. MAO enzyme turnover is ~10 days, but tissue-specific regeneration varies. Liver MAO rebuilds slower than platelet MAO. That’s why some patients have delayed reactions.
Pharmacists need to be trained to flag this. Not just print a flyer. Train them.
Aki Jones
December 8, 2025STOP. STOP. STOP. I can’t believe people are still eating ‘safe’ cheeses like mozzarella. What about cross-contamination? What if the deli slicer was used for blue cheese 2 hours ago? What about the packaging? What if the cheese was stored near aged parmesan? WHAT ABOUT THE AIR? Tyramine can linger in the environment! I’ve read studies - it’s airborne in high-humidity environments! You’re not safe unless you’re in a vacuum chamber with a food analyzer!
And don’t even get me started on the ‘bottled beer is safer’ myth - that’s just what the brewers want you to believe. They’re in cahoots with Big Pharma. I’ve seen the documents.
Jefriady Dahri
December 9, 2025Bro, I’m from India and I’ve seen this happen. My uncle had a hypertensive crisis after eating fermented fish curry with linezolid. No one told him. He thought ‘curry is just spice.’
But here’s the thing - we’re not helpless. I made a simple poster with pictures: red X on cheese, soy, wine. Green check on rice, eggs, fresh veggies. I gave it to 5 people in my village. One saved their dad.
You don’t need a PhD. You need a picture. And someone to care enough to show it to you.
❤️
Shivam Goel
December 10, 2025Let’s analyze the data: 17 documented cases. 3 deaths. 212 mmHg average systolic. That’s a 95th percentile hypertensive crisis. The odds of this happening are low - but the consequence is 100% catastrophic. Risk ≠ probability. This isn’t gambling - it’s a single-point failure mode.
And yet, we still prescribe linezolid like it’s amoxicillin. Why? Because we’re addicted to broad-spectrum solutions. We don’t want to wait for daptomycin culture results. We want to kill it now.
But ‘now’ can kill you too. The real failure isn’t the drug - it’s our impatience.
Timothy Sadleir
December 11, 2025The entire paradigm of pharmaceutical risk management is fundamentally flawed. The notion that individual behavioral modification - particularly in the context of complex, culturally embedded dietary practices - can serve as a reliable safety mechanism is not only naive, it is ethically indefensible. One cannot expect a patient to become a biochemist, a nutritionist, and a pharmacokineticist simultaneously, while managing a life-threatening infection. The onus must shift from patient compliance to drug design. Until then, we are merely administering a placebo of safety.
Erika Hunt
December 13, 2025I think this is one of the most important posts I’ve read in years. I’ve been on linezolid for 12 days and I’ve been terrified - not because I don’t trust the drug, but because no one explained how deep the rabbit hole goes.
I had no idea that even ‘safe’ foods like yogurt could be dangerous if they’re old. Or that leftover chicken soup could turn toxic after 4 days. I’ve been eating like a rabbit - steamed veggies, plain rice, boiled eggs. It’s boring, but I’m alive.
And I’m sharing this with my whole family. My sister just got prescribed it too. We’re all going to print this out and hang it on the fridge. Not because we’re paranoid - because we’re smart.
Lisa Odence
December 13, 2025Thank you for this 🙏 I’ve been on linezolid for 8 days and I’ve been avoiding everything - even my favorite soy-ginger stir fry. I didn’t know white wine was safer - I thought all alcohol was banned. I’m so relieved.
Also, I just sent this to my pharmacist. She said she’s going to update the warning pop-up in the system. That’s huge. We need more people like you who actually care.
❤️