
When you switch to a generic drug, you expect the same effect as the brand-name version. But what if your body doesn’t respond the same way-no matter how identical the pill looks? For many people, the difference isn’t about the manufacturer. It’s about genetics.
Why Your Family’s Medical History Matters More Than You Think
You might know your mom had high blood pressure, or your dad had a bad reaction to an antibiotic. But did you know those patterns aren’t just coincidence? They’re clues. Your genes, passed down from your parents and grandparents, influence how your body breaks down and responds to almost every medication-generic or not. The science behind this is called pharmacogenetics. It’s not science fiction. It’s real, and it’s being used in hospitals right now. Studies show that genetics account for 20% to 95% of why people react differently to the same drug. That means two people taking the same generic version of a painkiller or antidepressant might have completely different outcomes-one feels relief, the other gets sick. Take warfarin, a blood thinner. Some people need just 1 mg a day. Others need 10 mg. Why? Because of variations in two genes: CYP2C9 and VKORC1. African Americans, on average, need higher doses than people of European descent-not because of weight or diet, but because of inherited genetic differences. If your family has a history of bleeding or clotting issues, that’s not just a coincidence. It could be your genes talking.The Genes That Control How Your Body Handles Drugs
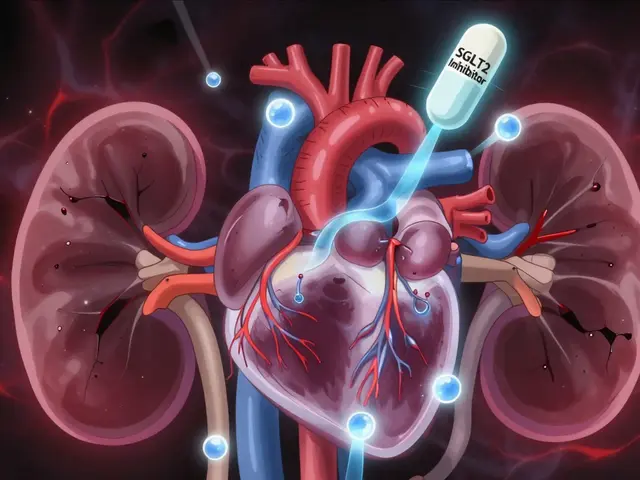
Your body uses enzymes to break down medications. The most important of these come from a family of genes called cytochrome P450. The most well-known is CYP2D6. It handles about 25% of all prescription drugs-including antidepressants like sertraline, painkillers like codeine, and beta-blockers like metoprolol. Here’s the problem: CYP2D6 has over 80 known variants. Some people have versions that work too fast. They turn codeine into morphine so quickly they get dangerously high levels. Others have versions that barely work at all. They get no pain relief, even at high doses. And because these genes are inherited, if your parent is a poor metabolizer, you might be too. Another key gene is CYP2C19. It affects proton pump inhibitors (PPIs) like omeprazole, used for acid reflux. About 15-20% of people of Asian descent are poor metabolizers of this drug. They need higher doses to get the same effect. If your family is from Southeast Asia and you’ve always needed more PPIs than others, that’s why. Then there’s TPMT. This gene breaks down thiopurines, drugs used for leukemia and autoimmune diseases. If you have two faulty copies of TPMT, even a standard dose can wipe out your white blood cells. Before treatment, doctors now test for this. In pediatric cancer centers, testing has cut severe side effects by 90%. And DPYD? That one controls how your body processes 5-fluorouracil, a chemotherapy drug. A single genetic variant can cause life-threatening toxicity. Patients who didn’t know they carried it ended up in intensive care. Now, testing before treatment is becoming standard in oncology.Why Generic Drugs Aren’t Always Interchangeable for Everyone
Generic drugs are required to have the same active ingredient as the brand-name version. That’s the law. But here’s what most people don’t realize: generics can have different inactive ingredients-fillers, dyes, coatings. For most people, that doesn’t matter. But for someone with a genetic variation that makes them ultra-sensitive to small changes in absorption? It can. A person who metabolizes drugs slowly might absorb a little more of the generic version because of a different coating. That extra amount, even 5%, could push them into toxicity. One patient in Melbourne reported switching from brand-name sertraline to a generic version and suddenly feeling dizzy, nauseous, and anxious. Her psychiatrist dismissed it as “adjustment.” But her gene test later showed she was a CYP2D6 poor metabolizer. The generic version had a slightly different release profile. It wasn’t the drug-it was how her body handled the change. That’s why some doctors now avoid switching patients on high-risk medications-like anticoagulants, antiepileptics, or psychiatric drugs-between brands and generics without monitoring. It’s not about the generic being inferior. It’s about individual biology.
What Your Family Tree Can Tell You About Your Drug Risks
Start simple. Ask your family:- Has anyone had a bad reaction to a common medication-like an antibiotic, painkiller, or antidepressant?
- Did anyone need a very high or very low dose of a drug to make it work?
- Has anyone had unexplained side effects-like severe fatigue, nausea, or bleeding-after starting a new drug?
- Has anyone been hospitalized because of a medication?
Testing Is Available-But It’s Not Everywhere
You can get a pharmacogenetic test now. Companies like Color Genomics and OneOme offer panels that check 10-20 key genes for under $300. Some insurance plans cover it if you’re on high-risk meds. The U.S. FDA now lists over 300 drugs with pharmacogenetic information on their labels. That includes antidepressants, statins, blood thinners, and cancer drugs. The Clinical Pharmacogenetics Implementation Consortium (CPIC) has 24 official guidelines telling doctors exactly what to do based on test results. But here’s the catch: most primary care doctors haven’t been trained to use this data. A 2022 survey found that only 32% of clinicians felt confident interpreting results for certain gene-drug pairs. Many don’t know how to read a CYP2D6 diplotype or what “ultrarapid metabolizer” means. If you’ve been tested and your doctor ignores the results, you’re not alone. One patient shared on Reddit that her $350 GeneSight test showed she was a CYP2D6 poor metabolizer. Her psychiatrist still prescribed sertraline. She ended up in serotonin syndrome. The solution? Bring your results. Ask: “Based on my genetics, is this the right drug and dose?”
What You Can Do Right Now
You don’t need to wait for a crisis. Here’s what you can do today:- Write down your family’s medication history-especially reactions, doses, and hospitalizations.
- If you’re on a high-risk drug (warfarin, clopidogrel, SSRIs, chemotherapy), ask your doctor if pharmacogenetic testing is right for you.
- If you’ve switched generics and noticed new side effects, don’t assume it’s “all in your head.” Talk to your pharmacist. They can check for known gene-drug interactions.
- Use free resources like PharmGKB or the NIH’s Pharmacogenomics Research Network to learn what your genes might mean.
What’s Next for Genetic Drug Testing
The field is growing fast. The NIH spent $127 million on pharmacogenomics research in 2023. The All of Us program plans to return genetic results to 1 million Americans by 2026. Hospitals like Mayo Clinic and Vanderbilt are already testing patients preemptively-before they even get a prescription. Soon, your electronic health record might automatically flag: “Patient is CYP2D6 poor metabolizer. Avoid codeine, tramadol, and paroxetine.” But for now, the power is still in your hands. Knowing your family’s history and understanding your own genetic risks can prevent a bad reaction before it happens.Can family history alone tell me how I’ll respond to generic drugs?
Family history gives you strong clues-like if relatives had bad reactions, needed unusually high or low doses, or were hospitalized for drug side effects. But it can’t give you the full picture. Two people with the same family history can have different gene variants. Genetic testing is the only way to know for sure how your body metabolizes drugs.
Are generic drugs less effective because of genetics?
No. Generic drugs are required to be bioequivalent to brand-name versions. But if your genes make you a slow or fast metabolizer, even small differences in how the drug is absorbed-due to different fillers or coatings-can affect you more than others. That’s not about effectiveness of the generic, but about how your body handles the specific formulation.
Which drugs are most affected by genetic differences?
The most well-studied include warfarin (blood thinner), clopidogrel (antiplatelet), SSRIs like sertraline and paroxetine, codeine and tramadol (painkillers), statins like simvastatin, and chemotherapy drugs like 5-fluorouracil and thiopurines. These have strong gene-drug links backed by clinical guidelines.
Is pharmacogenetic testing covered by insurance?
In the U.S., Medicare covers certain tests under the Molecular Diagnostic Services Program if ordered for specific drugs. Private insurers vary. In Australia, testing is mostly out-of-pocket unless part of a clinical trial or hospital program. Costs range from $200-$500. Ask your doctor or pharmacist about coverage options.
What if my doctor doesn’t believe in genetic testing for drugs?
Bring printed CPIC guidelines or FDA labeling that mentions your gene-drug pair. Many doctors are unaware of the evidence. You can also ask for a referral to a clinical pharmacist who specializes in pharmacogenomics-they’re trained to interpret results and work with prescribers.


Kihya Beitz
November 14, 2025So let me get this straight - we’re now supposed to gene-test before taking a generic ibuprofen? Next they’ll be scanning our DNA before we buy cough syrup. 🤦♀️ I swear, if I have to pay $300 just to find out if I can take Tylenol without turning into a zombie, I’m just gonna drink whiskey and hope for the best.
Jennifer Walton
November 15, 2025Genetics shape biology. Biology shapes experience. Experience shapes identity. But the system treats us like interchangeable parts. The pill doesn’t care who you are. Your body does.
Shyamal Spadoni
November 15, 2025you know what this is really about? big pharma and the FDA are scared of personalized medicine because if everyone starts testing their genes, they’ll realize most drugs are just expensive placebos with a fancy label. they want you to keep buying the same crap over and over. and now they’re pushing these ‘gene tests’ to make you think you need more meds instead of fixing the real problem - corporate greed. also, i heard the cyp2d6 gene was planted by aliens in 1987 during a secret moon mission. dont trust the fda. they’re not your friends. 🛸
Ogonna Igbo
November 16, 2025in nigeria we dont even have access to brand name drugs most times so why are you talking about generics like theyre some kind of conspiracy? we take what we get and pray. your genetics dont matter when you're choosing between a real pill and nothing. you people in the west think medicine is a luxury. its not. its survival. stop overcomplicating what is already broken
BABA SABKA
November 18, 2025the real issue here is pharmacogenomic equity. we’re talking about a biological reality that disproportionately impacts marginalized populations - African, Asian, Indigenous - whose genetic variants are underrepresented in clinical trials. if your ‘generic’ was tested on 90% white Europeans, and you’re South Asian, you’re basically a beta tester for someone else’s drug policy. this isn’t science. it’s colonialism with a lab coat. and yes, i’m calling it out.
Chris Bryan
November 19, 2025so now the government wants to track our DNA to control what meds we take? next they’ll implant microchips in our teeth so they can monitor our serotonin levels. this is how they start mandatory genetic profiling. you think this is about health? it’s about control. they want to know your weaknesses before you even know them. and don’t get me started on the data brokers selling your CYP2C19 results to insurance companies. you’re not a patient. you’re a dataset.
Jonathan Dobey
November 20, 2025ah yes - the sacred alchemy of modern medicine: grind a molecule into a powder, slap on a generic label, and pretend the universe doesn’t whisper your ancestral secrets through every enzyme in your liver. we’ve turned the human body into a vending machine - insert pill, receive outcome. But the machine doesn’t know you’re the child of a woman who bled out on warfarin, or the grandson of a man who turned blue on codeine. We are not pills. We are echoes. And the echoes are screaming.
ASHISH TURAN
November 20, 2025I’ve seen this in my family - my uncle took clopidogrel and had a stroke. My cousin took the same drug and was fine. We didn’t know why until my aunt got tested. Turns out, he was a CYP2C19 poor metabolizer. The doctor didn’t even know what that meant. Took us 3 years and $2K to find out. If you’re on blood thinners or SSRIs, just ask. No one’s coming to save you. You have to be your own advocate.
Ryan Airey
November 21, 2025Stop pretending this is about ‘personalized medicine.’ It’s about liability. If you die on a generic because your doctor didn’t test you, the hospital gets sued. So now they’re pushing genetic testing to cover their asses. Don’t be fooled. This isn’t care - it’s legal insurance dressed up as science.
Hollis Hollywood
November 22, 2025I used to think my anxiety was just stress. Then I switched from brand sertraline to a generic and suddenly couldn’t leave the house for a week. My therapist said it was ‘adjustment.’ I didn’t believe her. I got tested. CYP2D6 poor metabolizer. The generic had a different coating - slowed absorption just enough to spike my levels. I cried when I read the results. Not because I was broken - because no one had ever asked me how my body felt. Just what pills I was taking. I’m not mad at the system. I’m sad for everyone who never got the chance to be heard.
Aidan McCord-Amasis
November 23, 2025my grandma took warfarin for 20 years. never bled. then switched to generic. ended up in ER. they said ‘coincidence.’ lol. 🤡 gene test later confirmed: VKORC1 variant. now i test before any new med. no cap. 🧬💊
Adam Dille
November 25, 2025my cousin got tested after her dad had a bad reaction to statins. turns out she’s a SLCO1B1 slow transporter. her doc didn’t even know what that meant. so she found a pharmacist who did. now she takes a different statin and feels amazing. it’s not magic. it’s just… listening. 🤝
Katie Baker
November 26, 2025my mom’s side of the family has a history of bad reactions to antidepressants. I got tested before starting anything - and wow, what a relief. I didn’t have to guess. I didn’t have to suffer through 3 bad meds. I just walked into my doctor’s office with my report and said, ‘this is me.’ She actually listened. It felt like being seen for the first time. You’re not broken. You’re just different. And that’s okay.
John Foster
November 27, 2025The tragedy of modern pharmacology is not that we lack knowledge - it’s that we refuse to integrate it into the human condition. We have mapped the genome, yet we still treat the patient as an abstraction. We have guidelines that could prevent death, yet we outsource decision-making to algorithms written by corporate lawyers. The body remembers. It remembers your mother’s pain. It remembers your grandfather’s silence. It remembers the drug that made you weep in the shower. And yet, the system asks: ‘Are you compliant?’ Not: ‘Are you alive?’