When you feel like the room is spinning, you don’t just say you’re dizzy-you say you have vertigo. But if you just feel lightheaded, unsteady, or like you might pass out, that’s dizziness. These aren’t interchangeable terms. They’re different conditions with different causes, different treatments, and very different risks. Confusing them can delay care, waste time, and even put you in danger.
What Exactly Is Vertigo?
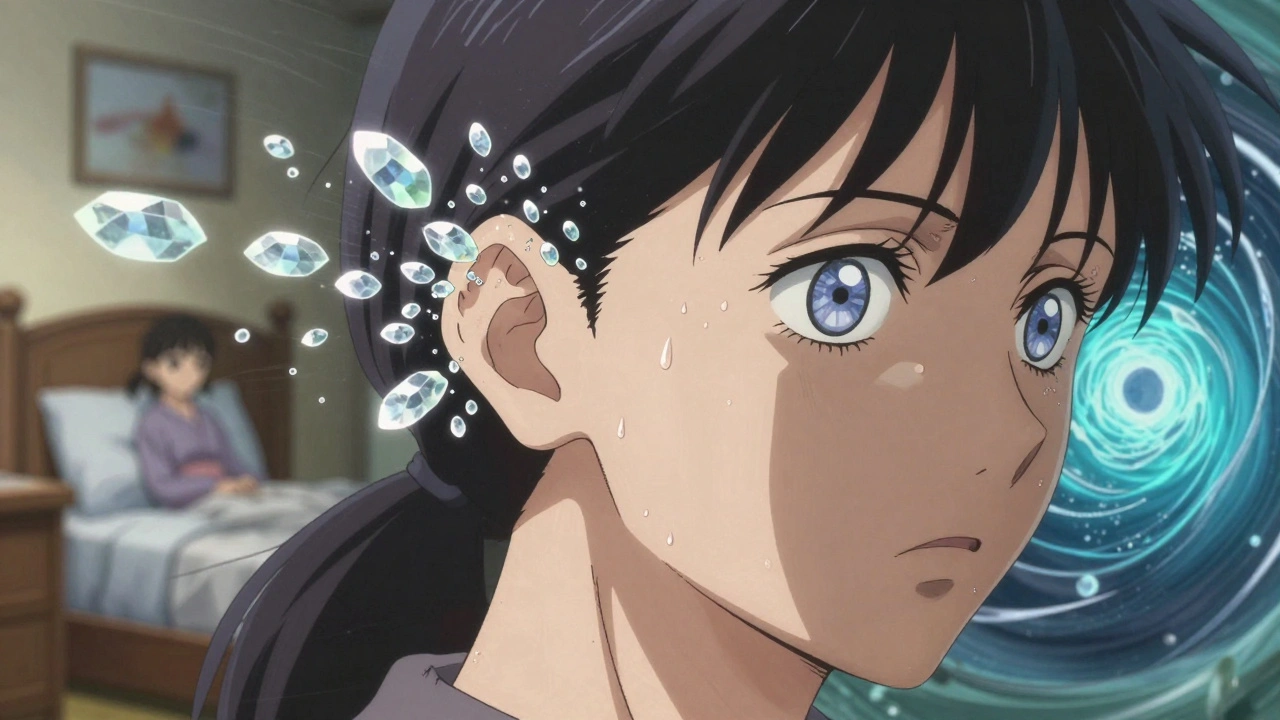
Vertigo isn’t just feeling off-balance. It’s the false sensation that you-or the world around you-is moving when you’re perfectly still. It’s the spinning feeling after you get off a merry-go-round, but it doesn’t go away. People describe it as being on a boat in rough seas, or like their bed is turning in circles. This isn’t anxiety. It’s not stress. It’s your brain getting conflicting signals from your inner ear and eyes.
The root of vertigo almost always lies in the vestibular system-the part of your inner ear that detects head movement and tells your brain where you are in space. When the semicircular canals or otolith organs in your ear send wrong signals, your brain gets confused. That’s when you feel the spin. The most common cause? Benign Paroxysmal Positional Vertigo, or BPPV. It happens when tiny calcium crystals (canaliths) break loose and float into the wrong part of your ear. A simple head movement-rolling over in bed, looking up at a shelf-triggers a sudden, intense spin that lasts less than a minute. BPPV affects 2.4% of people every year, and over half of those are over 50.
But vertigo can also come from your brain. Central vertigo, caused by neurological issues like stroke, multiple sclerosis, or vestibular migraine, is rarer but more dangerous. Unlike BPPV, it doesn’t always come with head movement. It can strike suddenly, even while sitting still. And it often comes with other red flags: double vision, slurred speech, weakness on one side, or trouble walking in a straight line. These aren’t just annoying symptoms-they’re warning signs.
What Exactly Is Dizziness?
Dizziness is the umbrella term for everything that isn’t vertigo. It’s the feeling of being faint, woozy, or floating. You might feel like you’re going to pass out, or that your head is light. There’s no spinning. No rotation. Just a sense of instability or disconnection from your body.
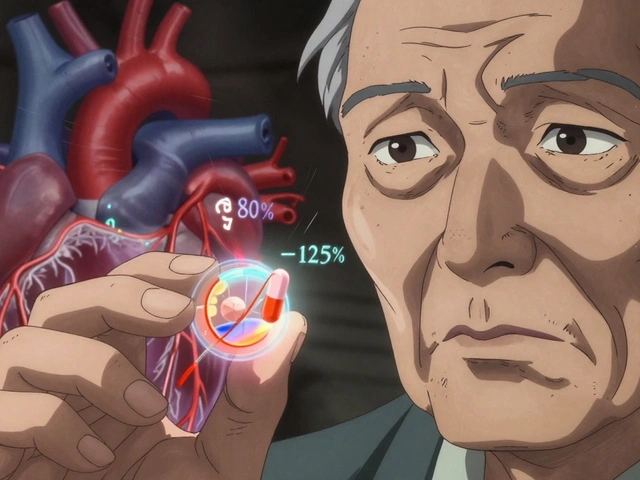
This kind of dizziness often comes from systems outside the inner ear. Low blood pressure when you stand up (orthostatic hypotension) is a big one-especially in older adults. A drop of 20 mmHg in systolic pressure can trigger it. Dehydration, anemia, low blood sugar, and even some medications like blood pressure pills or antidepressants can cause it. Anxiety and panic attacks also commonly present as dizziness, not vertigo. That’s why so many people are misdiagnosed: they’re told it’s stress, when it’s actually a metabolic or cardiovascular issue.
Here’s the catch: dizziness isn’t just one thing. It’s a symptom with dozens of possible causes. One study found that over half of older adults with dizziness have more than one cause at once-maybe low blood pressure, mild anemia, and medication side effects all adding up. That’s why treating it as a single problem often fails.
How Doctors Tell Them Apart
Doctors don’t guess. They test. The first clue? The pattern of symptoms. If spinning happens only when you move your head-rolling over, bending down, looking up-it’s almost certainly BPPV. If it happens while sitting still, or is constant, it could be neurological.
The gold standard test is videonystagmography, or VNG. It uses infrared cameras to track your eye movements. When your inner ear is damaged, your eyes jerk involuntarily in a specific rhythm-2 to 6 times per second. That’s called nystagmus. Peripheral vertigo (from the ear) produces nystagmus that changes direction with gaze. Central vertigo (from the brain) produces nystagmus that doesn’t change, or looks weirdly straight up and down. That’s a red flag for stroke.
Another quick test is the head impulse test. The doctor rapidly turns your head while you stare at their nose. If your eyes flick away and then snap back, your inner ear isn’t working properly. If your eyes stay locked on target, the problem might be in your brainstem.
And then there are the red flags that demand immediate imaging: sudden hearing loss, numbness on one side, trouble swallowing, or loss of coordination. These aren’t typical for BPPV. They point to stroke, tumor, or MS. The American Academy of Neurology says only 1-2% of vertigo cases need an MRI-but if you have those red flags, don’t wait. Get scanned now.
Common Causes Compared
Not all vertigo is the same. Not all dizziness is the same. Here’s what actually causes them:
| Condition | Type | Prevalence | Key Features |
|---|---|---|---|
| Benign Paroxysmal Positional Vertigo (BPPV) | Vertigo | 20-30% of vertigo cases | Spinning triggered by head movement, lasts seconds, resolves with Epley maneuver |
| Vestibular Neuritis | Vertigo | 5-10% of vertigo cases | Sudden, severe spinning lasting days, no hearing loss, often follows virus |
| Ménière’s Disease | Vertigo | 10-15% of vertigo cases | Spinning + ringing ears + hearing loss + fullness, episodes last hours |
| Vestibular Migraine | Vertigo | 7-10% of vertigo cases | Spinning with headache sensitivity to light/sound, often misdiagnosed as sinus |
| Orthostatic Hypotension | Dizziness | 20-30% of dizziness cases | Lightheadedness when standing, improves when sitting |
| Anemia or Low Blood Sugar | Dizziness | 15-20% of dizziness cases | Weakness, pale skin, sweating, improves after eating or iron supplements |
| Medication Side Effects | Dizziness | 5-10% of dizziness cases | Starts after new drug, improves after stopping |
| Anxiety/Panic Disorders | Dizziness | 10-15% of dizziness cases | Feeling unreal, chest tightness, rapid breathing, worsens with stress |
Treatment: What Actually Works
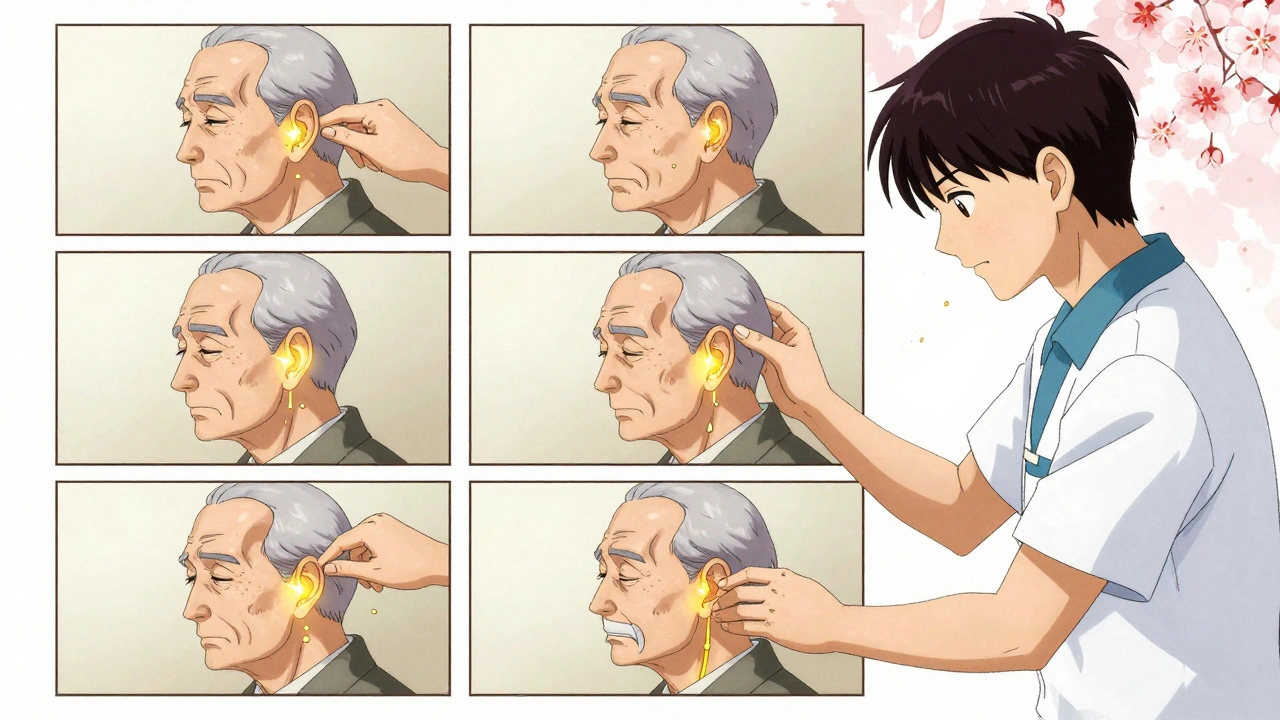
Wrong diagnosis = wrong treatment. If you have BPPV and take anti-nausea pills, you’ll feel better for a day. But the spinning will come back. The cure? A 5-minute maneuver.
The Epley maneuver is the most effective treatment for BPPV. It’s not surgery. It’s not medication. It’s a series of controlled head positions that guide the loose crystals back to where they belong. Studies show it works in 80-90% of cases after one or two sessions. Many people feel better within hours. One patient in Melbourne told me: “After 9 months of spinning every time I turned over, my physio did the Epley. I slept through the night for the first time in a year.”
For vestibular neuritis, the body usually heals itself over weeks. But vestibular rehabilitation therapy (VRT) helps speed it up. VRT isn’t just balance exercises. It’s a personalized program-starting with sitting still with eyes open, then closed, then standing, then walking while turning your head. It retrains your brain to rely on other senses when your inner ear is damaged. Most people see big improvement in 6-8 weeks. But only 12% of primary care doctors feel confident diagnosing this. That’s why so many people wait months.
Vestibular migraine? That’s trickier. It’s not a headache disorder. It’s a vestibular disorder that sometimes includes headaches. Common triggers: sleep changes, stress, certain foods like aged cheese or MSG. Treatment includes migraine preventatives like beta-blockers or topiramate, plus avoiding triggers. But 30% of cases are misdiagnosed as sinus infections or anxiety. If you’ve had “sinus dizziness” for years and antibiotics didn’t help, ask about vestibular migraine.
For dizziness from low blood pressure, simple steps help: drink more water, stand up slowly, wear compression socks. For anemia, iron supplements can fix it. For medication side effects, talk to your doctor about alternatives. And for anxiety-related dizziness? Cognitive behavioral therapy (CBT) works better than pills.
What to Do If You’re Still Struggling
Too many people suffer for months because they’re told it’s “just stress” or “aging.” But dizziness and vertigo aren’t normal. If you’ve had symptoms for more than a week, especially if they’re getting worse, see a specialist.
Look for a neurotologist or vestibular physiotherapist. They’re trained in these disorders. Ask for VNG testing. Ask about the Epley maneuver. Don’t accept a diagnosis of “anxiety” without ruling out physical causes first.
And if you’re experiencing red flags-sudden weakness, double vision, trouble speaking, loss of balance-you need to go to the ER. Stroke-related vertigo is rare, but it’s deadly if missed. The Johns Hopkins study found that only 12% of ER doctors correctly spot stroke vertigo using standard tools. That’s not your fault. It’s a system failure. But you can protect yourself: know the signs, speak up, and demand a brain scan if something feels wrong.
The good news? Most cases are treatable. BPPV? Usually fixed in one visit. Vestibular neuritis? Usually gone in weeks. Vestibular migraine? Manageable with lifestyle changes. Even chronic conditions like PPPD (persistent postural-perceptual dizziness) can improve with targeted therapy.
You don’t have to live with dizziness. You don’t have to be told it’s all in your head. There’s a reason for it. And there’s a way to fix it.
Is vertigo the same as dizziness?
No. Dizziness is a general term for feeling lightheaded, unsteady, or faint. Vertigo is a specific type of dizziness that feels like spinning or movement when you’re still. Vertigo is caused by inner ear or brain issues; dizziness can come from blood pressure, anemia, anxiety, or medications.
Can stress cause vertigo?
Stress doesn’t cause true vertigo, but it can trigger vestibular migraine-which feels like vertigo. Stress can also worsen existing vestibular disorders or make dizziness feel worse. But if you’re spinning, there’s a physical cause in your inner ear or brain, not just anxiety.
How long does BPPV last?
Without treatment, BPPV can last weeks to months. But with the Epley maneuver, most people feel better within 24 to 48 hours. About 85% of cases resolve after one or two sessions. Recurrence is common-about 50% of people have it come back within 5 years-but it’s treatable again.
When should I get an MRI for dizziness?
You need an MRI if you have red flags: sudden hearing loss, double vision, slurred speech, weakness on one side, trouble walking, or numbness. These suggest a stroke or neurological problem. If your dizziness is only triggered by head movement and you’re otherwise healthy, an MRI isn’t needed.
Can vertigo be cured?
Many forms of vertigo can be cured. BPPV is almost always cured with the Epley maneuver. Vestibular neuritis usually resolves on its own. Vestibular migraine can be managed long-term. Some conditions, like Ménière’s disease, can’t be cured but can be controlled. The key is getting the right diagnosis first.
What’s Next If You’re Still Dizzy
If you’ve been told it’s stress and you still feel off, ask for a referral to a vestibular specialist. Request a VNG test. Ask if you have BPPV. Ask if your symptoms match vestibular migraine. Don’t settle for vague answers.
If you’re over 65 and dizzy, get checked for orthostatic hypotension and medication interactions. If you’ve had a concussion and now feel unsteady, vestibular rehab can help-even years later.
The numbers don’t lie: 33% of adults over 65 have dizziness. But only 12% of primary care doctors feel confident diagnosing it. That gap is closing-more hospitals now have vestibular clinics, more therapists are certified, and insurance is covering more tests. You don’t have to suffer silently. There’s help. And you deserve to feel steady again.



Ada Maklagina
December 5, 2025I used to think I was just clumsy until I learned the difference between vertigo and dizziness. Now I know my morning spins were BPPV. Did the Epley maneuver at home with a YouTube video and slept through the night for the first time in years. No meds needed.
Harry Nguyen
December 7, 2025Of course the medical industrial complex wants you to believe there's a $500 test for something that's just your body telling you to stop drinking coffee and sleep better. They make money off confusion. The real cause? Modern life. Your inner ear doesn't know what to do with screens and processed food.
Stephanie Fiero
December 7, 2025OMG YES THIS. I was told it was anxiety for 3 years. Turns out I had vestibular neuritis after a bad cold. VRT saved me. If you're reading this and still feel off-go find a vestibular PT. Don't let doctors dismiss you. You're not crazy. Your brain just needs retraining. I'm proud of you for making it this far.
sean whitfield
December 9, 2025So we're supposed to believe that tiny rocks in your ear cause spinning? That's like saying a glitch in your phone's GPS causes you to think you're on Mars. The real issue? Your brain is tired of being lied to by the system. The crystals are just a metaphor for societal dissonance. You're not dizzy. You're awake.
Norene Fulwiler
December 9, 2025As someone from a culture where dizziness is often brushed off as 'too much thinking'-this article is a gift. My grandmother suffered for years because no one took it seriously. Now I tell everyone: if your head feels like it's underwater, get checked. It's not weakness. It's biology.
William Chin
December 9, 2025I must respectfully request that you clarify whether the referenced Johns Hopkins study was peer-reviewed and whether the 12% ER accuracy rate was adjusted for confounding variables such as patient presentation bias and diagnostic time constraints. The statistical validity of this assertion requires further scrutiny before it can be accepted as authoritative.
Chris Brown
December 10, 2025Let me be clear: if you're not willing to undergo an MRI for every instance of dizziness, you're putting your family at risk. This isn't about convenience. It's about moral responsibility. You think you're saving money by skipping the scan? You're gambling with your life-and everyone who loves you.
Krishan Patel
December 10, 2025In India, we have a term for this: 'bhram'. But modern medicine ignores our ancient wisdom. Ayurveda has treated vertigo with herbal oils and breathwork for 5000 years. Why are we trusting infrared cameras over centuries of tradition? The West keeps rebranding old knowledge as new science. It's arrogance disguised as progress.
Stephanie Bodde
December 11, 2025I just wanted to say thank you for this. 💙 My mom had BPPV and we thought it was just old age. After the Epley maneuver? She cried because she could finally turn her head without fear. You’re not alone. There’s help. And you’re stronger than you think.