Secondary Hyperparathyroidism – What It Is and How to Manage It
If you’ve ever heard the term “secondary hyperparathyroidism” and felt confused, you’re not alone. It’s a condition where your parathyroid glands over‑produce hormone because something else in your body is wrong—not because the glands themselves are faulty. The extra hormone tries to fix low calcium levels, but that can create new problems if left unchecked.
Why Does Secondary Hyperparathyroidism Occur?
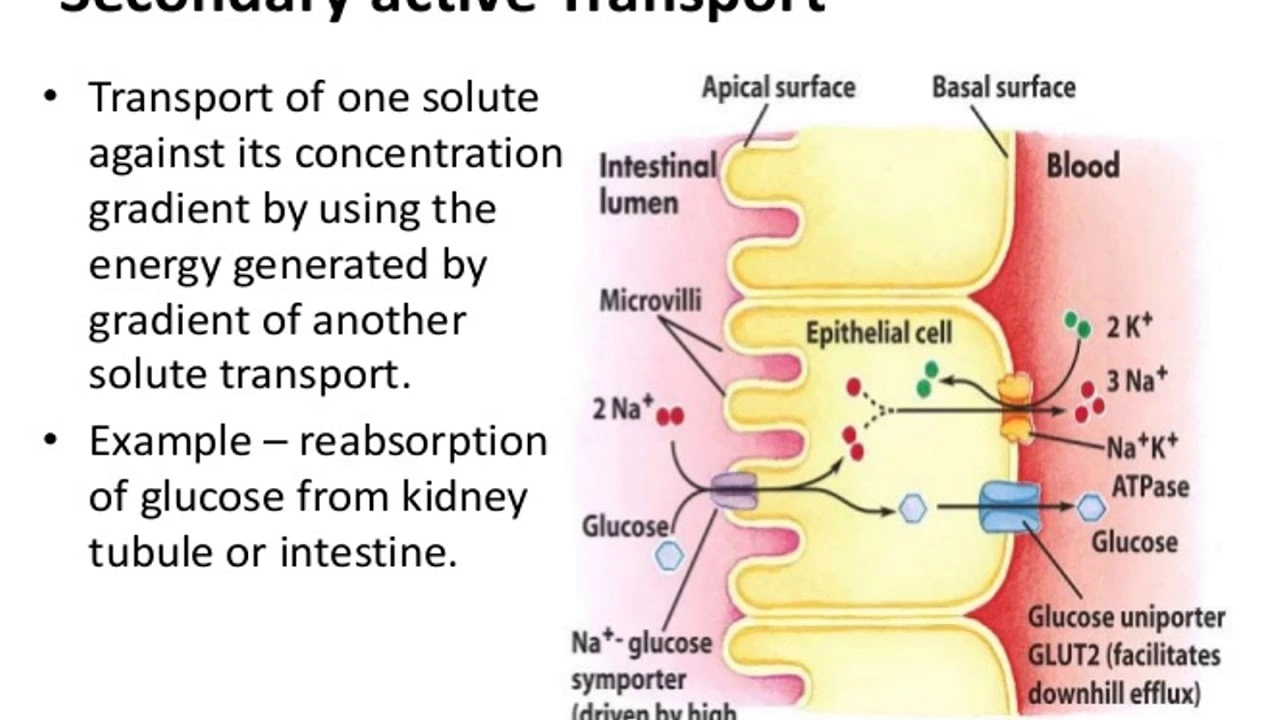
The most common trigger is chronic kidney disease. When kidneys can’t filter waste properly, they lose the ability to turn vitamin D into its active form and they fail to excrete phosphate. Low vitamin D and high phosphate both push calcium down, prompting the parathyroids to release more hormone.
Other culprits include severe vitamin D deficiency from lack of sunlight or poor diet, malabsorption disorders like Crohn’s disease, and certain medications that affect calcium metabolism. In every case, the body senses low calcium and reacts by cranking up parathyroid hormone (PTH) production.
How to Diagnose and Treat It
Doctors start with blood tests: they check PTH, calcium, phosphate, and vitamin D levels. A high PTH combined with low or normal calcium usually points to secondary hyperparathyroidism. Imaging of the parathyroid glands isn’t always needed, but a bone density scan can show if excess hormone is weakening bones.
Treatment focuses on fixing the root cause. For kidney‑related cases, controlling phosphate intake and using phosphate binders helps. Vitamin D supplements (usually active forms like calcitriol) raise calcium absorption, which often lowers PTH levels. In advanced kidney disease, dialysis or a kidney transplant can dramatically improve the hormonal imbalance.
Lifestyle tweaks also matter. Aim for 800–1,000 IU of vitamin D daily if you’re low, get safe sunlight exposure, and keep dietary phosphate in check by limiting processed foods and soda. Regular exercise supports bone health, while staying hydrated helps kidneys work better.
If medication and diet aren’t enough, doctors may prescribe calcimimetics—drugs that trick the parathyroid glands into thinking calcium is higher than it really is, thus dialing down PTH production. Surgery to remove part of the parathyroids is rare for secondary cases but can be considered when other measures fail.
Bottom line: secondary hyperparathyroidism isn’t a disease on its own; it’s a signal that something else needs attention. By addressing kidney health, vitamin D status, and phosphate balance, most people can bring PTH back to normal and protect their bones and cardiovascular system.