Pelvic Inflammatory Disease (PID): What It Is and How to Treat It
If you’ve ever heard doctors mention PID, you probably wondered what it really means. Pelvic inflammatory disease is an infection that spreads to a woman’s uterus, fallopian tubes, or ovaries. The infection usually starts with sexually transmitted bacteria like chlamydia or gonorrhea, but other germs can cause it too.
Why does PID matter? Left untreated, the inflammation can scar the reproductive organs, making pregnancies harder and increasing the risk of chronic pelvic pain. Knowing the warning signs early helps you get treatment before any lasting damage occurs.
Common signs you shouldn’t ignore
The symptoms often feel like a bad menstrual cramp or a simple bladder infection, which is why they can be missed. Most women notice one or more of these clues:
- Pain in the lower belly that gets worse during sex or when you pee.
- Unusual vaginal discharge—yellow, gray, or with an odd smell.
- Irregular periods, spotting between cycles, or heavier bleeding.
- Fever, chills, or feeling generally run down.
If you have any of these signs, especially after a recent STI test or treatment, call your health provider right away. Early testing can confirm PID and start the right antibiotics fast.
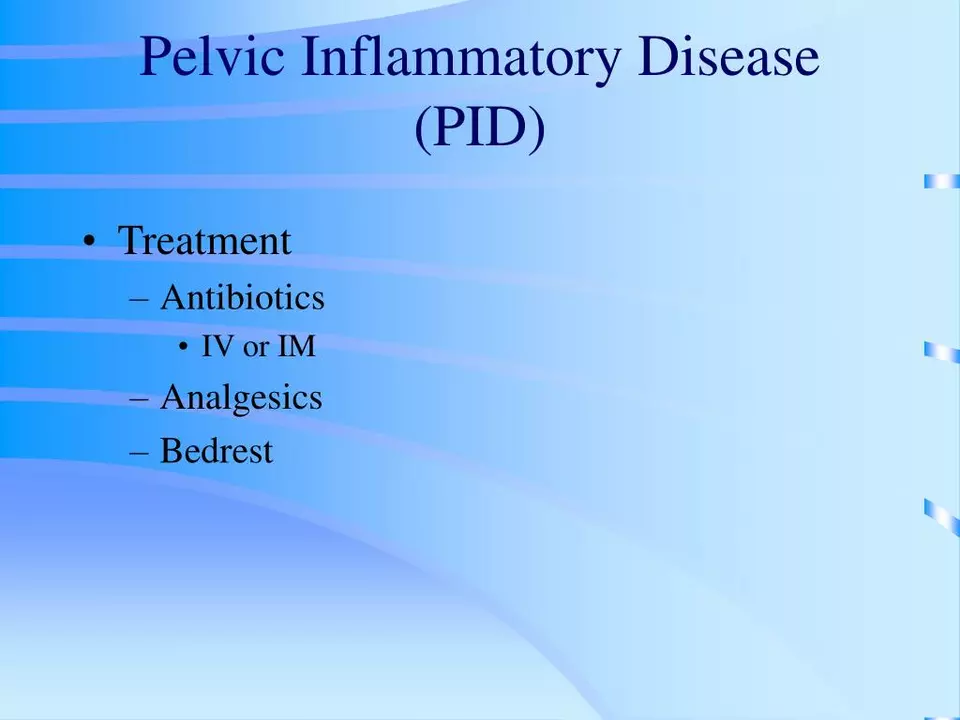
How doctors treat PID and what meds work best
Treatment focuses on wiping out the infection and preventing it from coming back. Doctors usually prescribe a combination of antibiotics that cover both chlamydia and gonorrhea, plus any other bacteria that might be involved. A typical regimen includes an oral dose of azithromycin or doxycycline together with an injection of ceftriaxone.
Finish the full course even if you feel better after a few days—stopping early can let hidden germs survive and cause a repeat infection. Your doctor may also recommend pain relievers like ibuprofen to calm inflammation while the antibiotics do their work.
Because PID often spreads from a partner’s infection, it’s smart to have your sexual partner tested and treated at the same time. This stops the cycle of reinfection and protects both of you.
Follow‑up visits are key. After finishing antibiotics, the doctor will check if symptoms disappeared and may do an ultrasound to see whether any scarring formed. If pain persists, additional treatments such as hormonal therapy or surgery might be discussed.
Preventing PID in the first place is easier than fixing it later. Use condoms consistently, get regular STI screenings, and treat any chlamydia or gonorrhea right away. Even a single untreated infection can trigger PID.
If you’re pregnant or think you might be, tell your provider immediately. Some antibiotics are safe during pregnancy, while others aren’t, so the treatment plan may change to protect both you and the baby.
Living with PID doesn’t have to ruin your life. With quick diagnosis, proper medication, and partner cooperation, most women recover fully and go on to have healthy pregnancies later on.
Bottom line: notice the pain, watch for unusual discharge, get tested fast, and follow through with the full antibiotic plan. Those steps keep PID from causing long‑term problems and put you back in control of your health.