Contraceptive Safety: Your Practical Guide
If you’re looking at birth control, safety should be the first thing on your checklist. You want something that works, doesn’t mess with your daily life, and won’t give you surprise health problems. In this guide we’ll break down the most common methods, their typical side effects, and easy ways to make a smart choice.
First off, remember that no method is 100% risk‑free. Every drug or device interacts with your body in its own way. The key is understanding what’s normal for you and what might be a red flag. Keep an eye on things like unexpected weight changes, mood swings, or unusual bleeding – those are often the first signs something needs a closer look.
Types of Birth Control and Their Safety Profiles
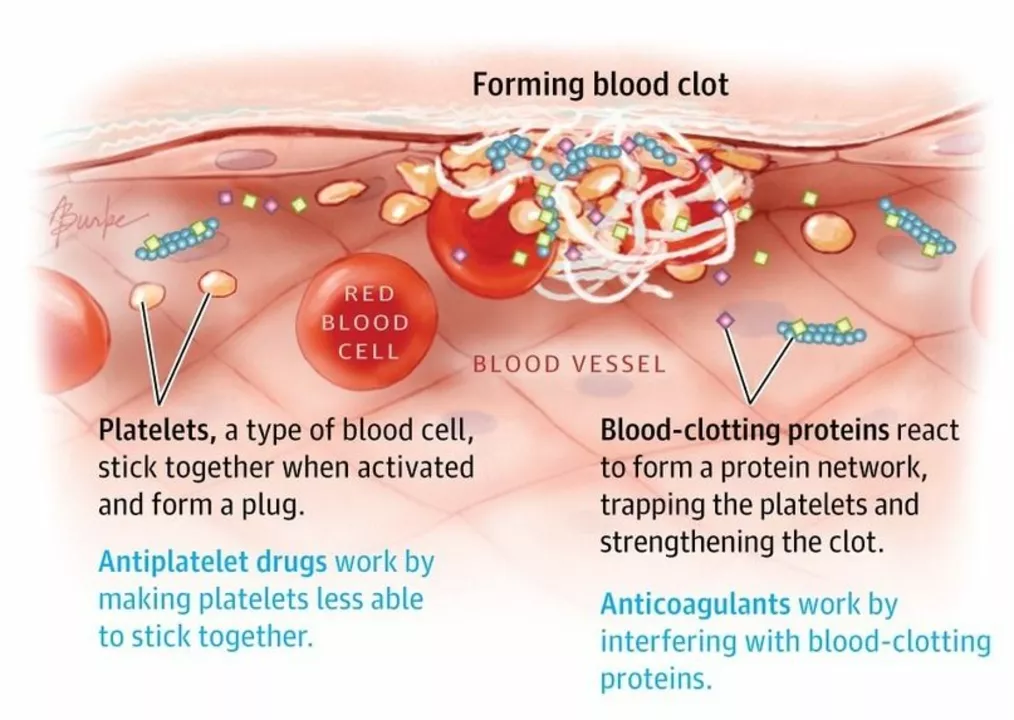
Pill (combined oral contraceptive): The most popular option. It mixes estrogen and progestin to stop ovulation. Most people handle it well, but a small group may feel nausea, breast tenderness, or slight blood‑spotting in the first months. Serious risks – like blood clots – are rare but more likely if you smoke, are over 35, or have certain genetic factors.
Progestin‑only pill: Good for people who can’t take estrogen. It often causes less spotting, but missed doses matter a lot. Side effects may include mood shifts and acne.
IUDs (copper or hormonal): Inserted by a doctor, they last years. Hormonal IUDs release small amounts of progestin locally, which means fewer systemic side effects. Copper IUDs can cause heavier periods for the first few cycles. Both types have low failure rates and are considered safe for most users.
Implants: Small rods placed under the skin that release progestin over 3‑5 years. Users often report lighter periods or no bleeding at all, which many like. Some notice weight gain or mood changes – again, it varies by person.
Barrier methods (condoms, diaphragm): No hormones, so side effects are minimal. The main safety concern is correct use; a slip can lead to an unwanted pregnancy.
How to Choose the Right Method for You
Start with a honest chat with your healthcare provider. Bring up any health conditions – like high blood pressure, migraines, or clotting disorders – because they steer which options are safe. Ask about how each method might affect things you care about: weight, mood, menstrual flow.
If you’re sensitive to hormones, consider non‑hormonal choices first (copper IUD, condoms). If you want lighter periods, hormonal IUDs or implants often deliver that benefit without daily pills.
Don’t forget lifestyle factors. Smoking? That rules out estrogen‑based pills for many adults over 35. Busy schedule? A long‑acting method like an IUD or implant removes the need to remember a daily dose.
When you start a new method, keep a simple log for the first few months. Note any bleeding patterns, mood changes, headaches, or weight shifts. If something feels off, reach out to your doctor – early tweaks can prevent bigger issues later.
Lastly, stay up‑to‑date with reputable sources. Websites that require medical review, official health department pages, and your own doctor's office are the best places for reliable info. Avoid forums that push unverified miracle cures or scare tactics.
Contraceptive safety isn’t about finding a perfect method; it’s about matching a safe option to your body and lifestyle. Use this guide as a starting point, ask questions, track how you feel, and adjust as needed. Your health and peace of mind are worth the effort.