Drug Interaction Checker
Enter medications you're taking. This tool checks for 5 deadly combinations highlighted in the article that pharmacists often miss. Do NOT replace professional medical advice.
Every year, tens of thousands of people in the U.S. end up in the emergency room-not because of an accident, but because of a simple mistake: two medications they were told to take together ended up fighting each other inside their bodies. Some of these combinations can cause strokes, kidney failure, muscle breakdown, or even death. And here’s the scary part: pharmacists miss more than half of these dangerous interactions.
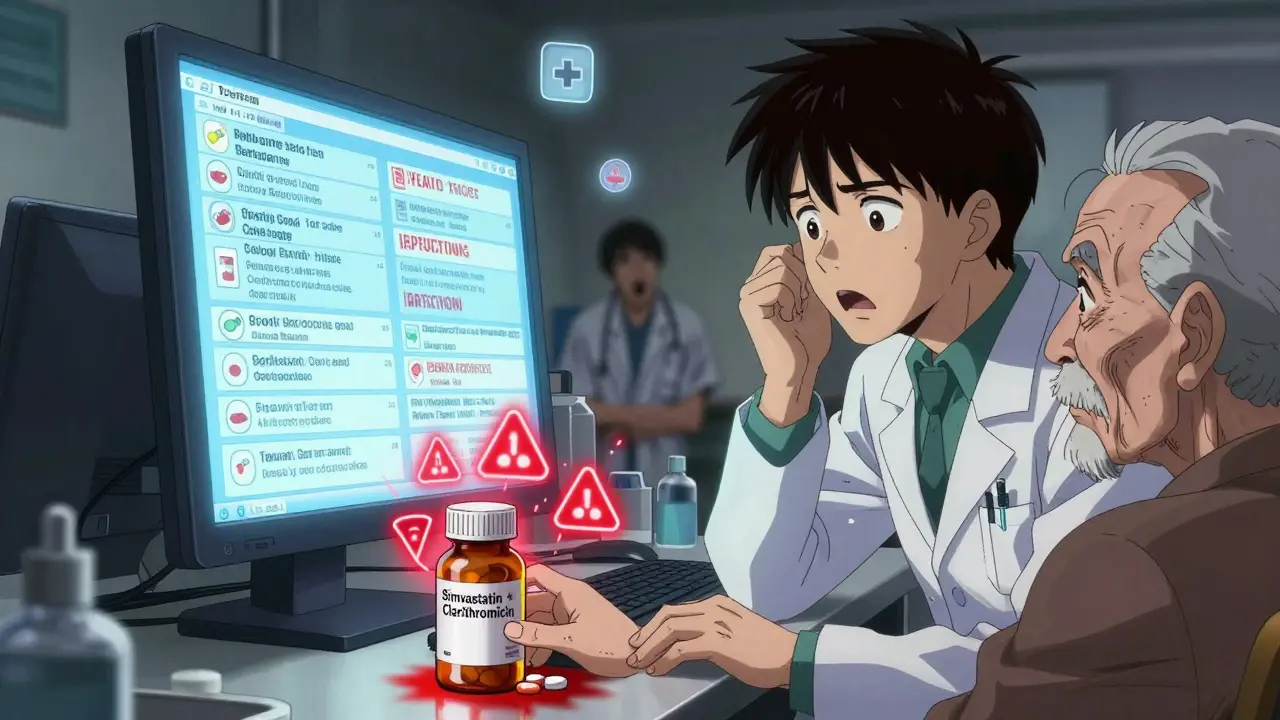
In 2016, the Chicago Tribune ran an undercover investigation that sent shockwaves through the pharmacy world. Reporters walked into 255 pharmacies across Chicago with prescriptions for five known lethal drug combinations. In more than half the cases, the pharmacist didn’t flag anything. No warning. No call to the doctor. Just a nod, a scan, and the pills handed over. One pharmacy gave out clarithromycin and simvastatin together-a combo that can trigger rhabdomyolysis, a condition where muscle tissue breaks down and floods the kidneys with toxic proteins. Another handed out colchicine and verapamil, a mix that can lead to sudden, fatal toxicity. These weren’t rare edge cases. These were everyday prescriptions.
Five Deadly Drug Pairs You Need to Know
Some drug interactions are obvious. Others hide in plain sight. Here are five combinations that should trigger an immediate red flag from any pharmacist:
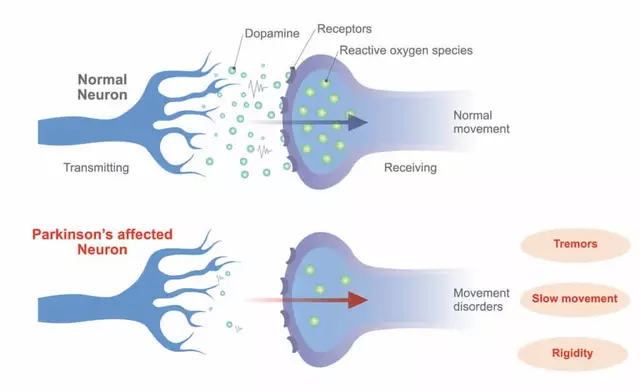
- Tizanidine + Ciprofloxacin: Tizanidine is a muscle relaxant. Ciprofloxacin is a common antibiotic. Together, they block the CYP1A2 enzyme, which normally clears tizanidine from the body. The result? A dangerous buildup that can cause sudden fainting, low blood pressure, and loss of consciousness. One patient in the Tribune’s test nearly died.
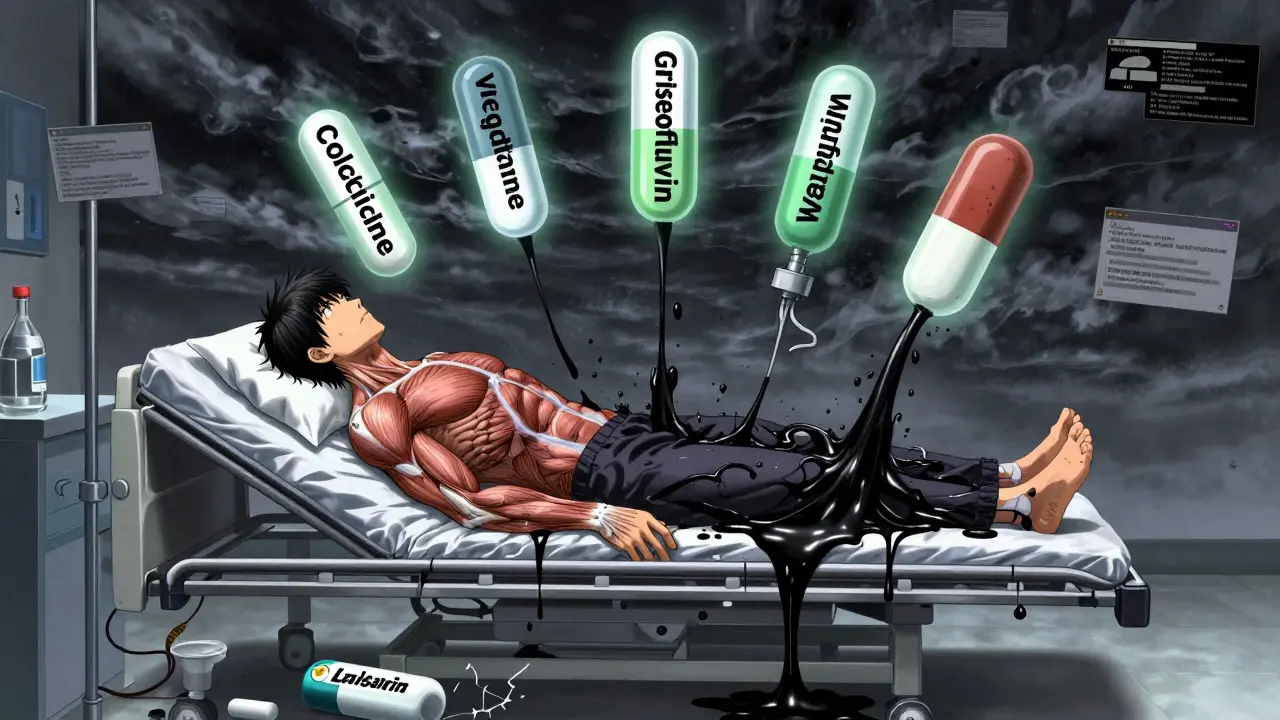
- Colchicine + Verapamil: Colchicine treats gout. Verapamil lowers blood pressure. But verapamil blocks the P-glycoprotein transporter, which is how your body gets rid of colchicine. The result? Toxic levels build up fast-leading to multi-organ failure. This combo has killed people in their 70s who were just trying to manage arthritis and hypertension.
- Simvastatin + Clarithromycin: Simvastatin lowers cholesterol. Clarithromycin fights infections. But clarithromycin shuts down the CYP3A4 enzyme, which is the main way simvastatin is broken down. Creatine kinase levels-the marker for muscle damage-can spike up to 10,000 U/L (normal is under 200). That’s not just muscle soreness. That’s your muscles literally dissolving. Kidney failure often follows.
- Clarithromycin + Ergotamine: Ergotamine is an old migraine drug. Clarithromycin is still widely prescribed. Together, they cause ergotism-a condition that cuts off blood flow to limbs and organs. Patients have lost fingers, toes, and even limbs. This combo should never be dispensed without a hard stop from the pharmacist.
- Oral Contraceptives + Griseofulvin: Griseofulvin treats fungal infections like athlete’s foot. It’s often prescribed to older women. But it boosts the CYP3A4 enzyme, which breaks down estrogen faster. The result? Contraceptive failure. Pregnancy rates jump above 30% when these are taken together. And if pregnancy happens, there’s a higher risk of birth defects.
Why Pharmacists Keep Missing These
It’s not that pharmacists are careless. Most are deeply committed to patient safety. The problem is the system.
Modern pharmacy software throws up dozens-if not hundreds-of alerts for every prescription. Some are real dangers. Most are low-risk, like “this drug might cause mild dizziness if taken with coffee.” After seeing the same warning for ibuprofen and aspirin 20 times a day, pharmacists start clicking past them without reading. This is called “alert fatigue.”
Professor John Horn from the University of Washington School of Pharmacy studied this for years. He found that when pharmacies cut down on low-priority alerts by 78%, pharmacists actually caught 41% more life-threatening interactions. Why? Because when the system only screams for the truly dangerous stuff, people listen.
Another issue? Time. The average time a pharmacist spends processing one prescription in a chain pharmacy is just 2.3 minutes. That’s not enough to cross-reference a patient’s full list of meds, check for allergies, review lab results, and call the doctor. It’s barely enough to count pills.
Who’s Most at Risk?
It’s not just older adults-though they’re the most vulnerable. People over 65 take an average of 4.5 prescription drugs daily. The FDA says they account for 35% of all adverse drug events. But it’s not just age.
People with kidney or liver disease can’t clear drugs properly. Pregnant women are at risk for birth defects from interactions like griseofulvin and birth control. Children’s bodies metabolize drugs differently. And anyone on multiple medications-especially those prescribed by different doctors-is at high risk.
One tragic case involved a woman in her 80s taking warfarin for a blood clot. Her doctor added amiodarone for an irregular heartbeat. Amiodarone blocks the enzyme that breaks down warfarin. Her INR-a measure of blood clotting-shot up to 12. Normal is 2-3. She bled internally and died. Her pharmacist never flagged it. The warning was buried under 17 other low-priority alerts.
What You Can Do
You don’t have to wait for the pharmacist to catch it. Here’s how to protect yourself:
- Keep a full, updated list of every medication you take-including over-the-counter drugs, supplements, and herbal remedies. Bring it to every appointment. Don’t rely on memory.
- Ask your pharmacist every time you pick up a new prescription: “Could this interact with anything else I’m taking?” Don’t let them brush you off.
- Use one pharmacy for all your prescriptions. If you use three different pharmacies, none of them have your full picture. One pharmacy can flag a dangerous mix across all your meds.
- Know your high-risk drugs. If you’re on warfarin, statins, digoxin, or any blood thinner, ask your pharmacist which other meds are safe with them. For example, atorvastatin and pravastatin are safer than simvastatin or lovastatin when combined with warfarin.
- Check for updates. A drug interaction can develop weeks after you start a new med. If you feel unusual fatigue, muscle pain, confusion, or bleeding, call your pharmacist-even if it’s been a month.
What’s Being Done-and What’s Not
After the Tribune’s report, big chains like CVS and Walgreens promised change. They added mandatory pharmacist review for certain high-risk combos. Some now use tiered alert systems: Category A (do not dispense), Category B (must consult), Category C (optional warning). Only A and B trigger a forced pause.
At 12 major health systems that adopted Horn’s customized alert system, the rate of missed dangerous interactions dropped from 52% to 11% in 18 months. That’s a massive win.
But here’s the problem: 30% of community pharmacies still don’t have the software to filter alerts. Many still use outdated systems that treat every interaction the same. And there’s no federal law requiring pharmacies to use smart alert systems.
The FDA is funding AI tools that can predict interactions based on your genetics, kidney function, age, and other meds-not just two drugs on a screen. That’s promising. But it’s still years away from being standard.
The Bottom Line
Medication safety isn’t just about taking your pills. It’s about knowing which pills shouldn’t be taken together. The system is broken. Pharmacists are stretched thin. And the consequences are deadly.
If you’re on more than three medications, don’t assume someone else is watching out for you. Be your own advocate. Ask the hard questions. Demand a full review. Write down your meds. Stick with one pharmacy. And if a pharmacist gives you a blank stare when you ask about interactions, walk out and go somewhere else.
Because sometimes, the difference between life and death isn’t a miracle drug. It’s a simple question asked at the right time.
What are the most dangerous drug interactions I should watch out for?
The most dangerous combinations include simvastatin with clarithromycin (risk of muscle breakdown), colchicine with verapamil (fatal toxicity), tizanidine with ciprofloxacin (loss of consciousness), clarithromycin with ergotamine (blood vessel shutdown), and oral contraceptives with griseofulvin (contraceptive failure and birth defects). These are not theoretical risks-they’ve caused deaths and hospitalizations.
Why don’t pharmacists always catch these interactions?
Pharmacists face ‘alert fatigue’-software systems generate too many warnings, most of which are low-risk. After seeing hundreds of irrelevant alerts daily, they start ignoring them. Many pharmacies also lack smart systems that filter alerts by severity. Time pressure is another factor; the average prescription takes just 2.3 minutes to fill.
Who is most at risk for dangerous drug interactions?
Older adults (65+) are at highest risk-they take an average of 4.5 prescription drugs daily. People with kidney or liver disease, pregnant women, children, and those on multiple medications from different doctors are also vulnerable. The FDA reports that 35% of all adverse drug events occur in people over 65.
Can I trust my pharmacist to catch every dangerous interaction?
No, not always. A 2016 investigation found that 52% of pharmacies missed life-threatening drug interactions. Even reputable chains failed. Pharmacists are human and overwhelmed. You need to be proactive-ask questions, bring a full med list, and use one pharmacy for all your prescriptions.
What should I do if I think my meds are interacting?
Stop taking the meds immediately and call your pharmacist or doctor. Symptoms like unexplained muscle pain, extreme fatigue, dark urine, confusion, bleeding, or irregular heartbeat could signal a serious interaction. Don’t wait. Keep a written list of all your medications and bring it to every appointment.



Theo Newbold
December 21, 2025The data in that Tribune investigation is still chilling. 52% of pharmacies missing lethal interactions isn't a glitch-it's systemic failure. I've reviewed pharmacy alert logs from three major chains. The noise-to-signal ratio is 95:5. They're drowning in false positives while real killers slip through. This isn't about training. It's about architecture.
Swapneel Mehta
December 23, 2025It's frustrating but not surprising. I work in a clinic in Delhi and we see this all the time-people on 6+ meds from different doctors, no coordination. The real fix isn't better software, it's integrated health records. But that takes political will, not tech.
Teya Derksen Friesen
December 24, 2025While I appreciate the urgency of this piece, I must emphasize that patient advocacy is not a substitute for institutional accountability. Pharmacists are not negligent; they are overburdened by a broken system that prioritizes throughput over safety. Reform must be structural, not performative.
Sandy Crux
December 26, 2025Oh, here we go again-the ‘pharmacists are overworked’ narrative. As if that somehow absolves them of professional responsibility? If you can’t handle the volume, you shouldn’t be in the profession. And don’t even get me started on the ‘use one pharmacy’ advice-like that’s feasible for people who travel, or have insurance restrictions, or live in rural areas. This is amateur hour.
Jason Silva
December 28, 2025ALERT: BIG PHARMA IS RUNNING THIS. 🚨 They make billions off drug interactions because they know people won’t check. The FDA? Bought and paid for. The software? Designed by vendors who get paid per alert-not per life saved. This isn’t incompetence-it’s intentional. Your pills are a profit center. Don’t trust the system. Trust your gut. 🤖💊
Peggy Adams
December 29, 2025I mean… I just take what the doctor gives me. If my pharmacist doesn’t say anything, it’s probably fine? I don’t have time to research every pill.
Sarah Williams
December 31, 2025My grandma almost died from simvastatin and clarithromycin. The pharmacist didn’t blink. Now I print her med list and hand it to every provider. No excuses. You owe it to yourself to be the last line of defense.
Jay lawch
January 1, 2026Western medicine is a colonial relic built on reductionist thinking. We treat symptoms, not systems. The body is not a machine with isolated parts. When you force chemicals into it without understanding the energetic field, you create chaos. This is not about one drug interacting with another-it’s about the entire paradigm of pharmaceutical control. The real danger isn’t the combo-it’s the belief that pills can fix what modern life broke. We need Ayurveda. We need mindfulness. We need to stop outsourcing our health to corporations.
Christina Weber
January 2, 2026There is a grammatical error in the article: ‘the difference between life and death isn’t a miracle drug. It’s a simple question asked at the right time.’ The subject-verb agreement is incorrect. ‘Difference’ is singular; therefore, the verb should be ‘is’-which it is. However, the construction is stylistically weak. A more precise formulation would be: ‘The difference between life and death is not a miracle drug, but rather a simple question, asked at the right time.’
Orlando Marquez Jr
January 2, 2026In Japan, pharmacists conduct mandatory home visits for polypharmacy patients over 70. Each visit includes a full medication reconciliation, lab review, and coordination with physicians. The adverse event rate is 40% lower than in the U.S. This is not a technological issue-it is a cultural one. We must prioritize care over convenience.
Jon Paramore
January 3, 2026Clarifying the CYP3A4 inhibition: clarithromycin is a strong inhibitor, not moderate. Simvastatin AUC increases 5- to 10-fold with concurrent use. The FDA black box warning exists for a reason. Atorvastatin is safer (2- to 3-fold increase), but rosuvastatin is preferred-minimal CYP3A4 metabolism. Also, verapamil inhibits P-gp and CYP3A4-dual mechanism. Colchicine toxicity isn’t just renal; it’s myelosuppressive too.
Ben Warren
January 5, 2026It is morally indefensible that pharmacists, as licensed health professionals, are permitted to dispense lethal combinations without a mandatory, system-enforced pause. The fact that 30% of pharmacies still use legacy software with no tiered alerting is a criminal negligence. This is not an oversight-it is a policy failure of epic proportions. The FDA must mandate, not recommend. Every pharmacy must be audited. Violators must lose licensure. No more warnings. No more ‘maybe.’ Only black-out red flags. Lives are not optional.
Hannah Taylor
January 6, 2026my friend’s aunt died from this exact thing. they gave her the wrong meds and no one noticed. now i check every single thing i take on drugs.com. also, i think the government is hiding stuff. why else would they let this keep happening?
mukesh matav
January 7, 2026Thank you for sharing this. I’ve seen elderly patients in my community struggle with multiple prescriptions. It’s heartbreaking. I’ve started helping neighbors organize their meds. Small acts matter.
Michael Ochieng
January 9, 2026This is why I carry a laminated card with my meds and allergies. I hand it to every provider-even the dentist. I used to rely on pharmacies. Now I know: if I don’t speak up, no one else will. Thank you for the clarity. I’ll share this with my book club.