
Post-Void Residual Volume Checker
Your Post-Void Residual Volume Analysis
Enter your post-void residual volume (in milliliters) to understand what it means for your urinary health.
When the bladder can’t empty properly, the result is urinary retention - a condition that ranges from a sudden inability to urinate to a chronic, slow‑draining bladder. While catheters and medication are common first‑line options, physical therapy for urinary retention offers a non‑invasive way to restore muscle control, improve nerve signaling, and boost quality of life.
What Causes Urinary Retention?
Understanding the root of the problem makes it easier to see why movement‑based care works. Most cases fall into two buckets:
- Obstructive - prostate enlargement, urethral strictures, or pelvic tumors that physically block urine flow.
- Neurogenic - nerve damage from spinal cord injuries, diabetes, multiple sclerosis, or post‑surgical scarring that hampers the bladder’s signal to contract.
Even when the cause is structural, the muscles surrounding the bladder often become weak or uncoordinated, creating a perfect storm for retention.
Why Physical Therapy Fits In
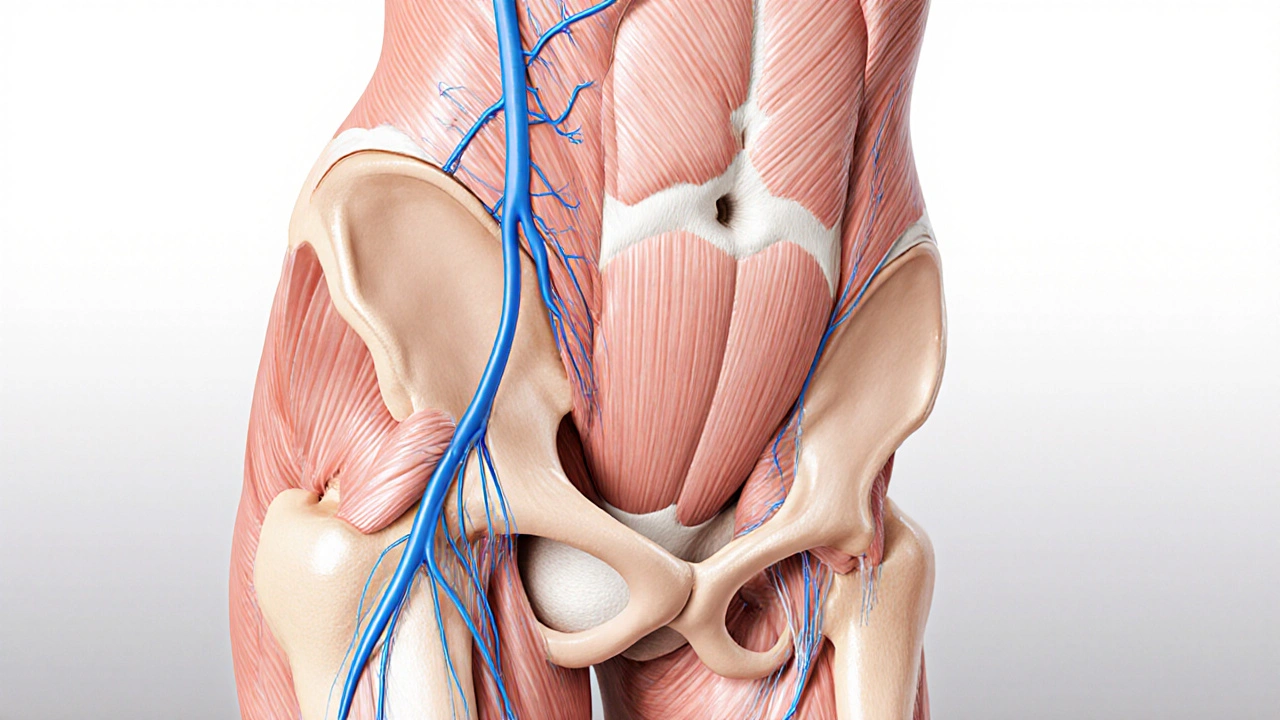
Physical therapy (PT) isn’t just about joint pain; it targets the whole neuromuscular system. In the context of urinary retention, PT aims to:
- Strengthen the pelvic floor muscles, the ring‑like group that squeezes the urethra and supports the bladder.
- Re‑teach the brain‑bladder‑spine communication pathway through neuromuscular re‑education, a series of guided movements that reset timing.
- Improve overall core stability, which indirectly influences bladder pressure.
Because PT works from the inside out, it can reduce reliance on catheters and lower the dose of prescription meds.
Core PT Techniques for Urinary Retention
Therapists usually blend several evidence‑based tools. Below is a quick rundown of the most common ones.
- Pelvic floor muscle training, also called Kegel exercises, teaches patients to contract and relax the correct muscle group in a timed pattern. Sessions start with biofeedback to confirm the right muscles are firing.
- Bladder training involves scheduled voiding and progressive lengthening of intervals, helping the bladder tolerate larger volumes before the urge to go.
- Biofeedback uses surface EMG sensors or a perineal probe to give real‑time visual or auditory cues, ensuring patients aren’t contracting surrounding thigh or abdominal muscles instead of the pelvic floor.
- Kinesiology taping can be applied around the lower abdomen to provide gentle proprioceptive feedback, reminding the nervous system to initiate a coordinated voiding effort.
- Intermittent catheterization training is taught to patients who still need occasional catheter use, focusing on proper technique to avoid infection while PT works on muscle recovery.
Comparison: Physical Therapy vs. Other Treatments
| Approach | How it works | Main Benefits | Typical Course |
|---|---|---|---|
| Physical therapy | Strengthens pelvic floor, retrains nerve‑muscle pathways, improves bladder capacity. | Non‑invasive, low side‑effects, improves overall core health, may reduce medication. | 1-2 sessions/week for 6-12 weeks, plus home exercises. |
| Medications (alpha‑blockers, cholinergics) | Relax urethral sphincter or stimulate bladder muscle. | Quick symptom relief, easy prescription. | Daily pills; effectiveness may wane over months. |
| Surgery (e.g., TURP, bladder augmentation) | Physically removes obstruction or enlarges bladder capacity. | Definitive solution for structural blockages. | One‑time procedure, weeks of recovery, possible complications. |
When to Seek a PT Evaluation
Not every case of urinary retention needs a therapist right away. Look for these red flags that signal PT could add value:
- Persistent post‑void residual volume over 150mL measured by ultrasound.
- Frequent urgency or leakage despite medication.
- History of pelvic surgery, childbirth, or spinal injury with lingering bladder issues.
- Desire to wean off catheters or reduce drug side‑effects.
If you tick any of these boxes, ask your urologist for a referral to a licensed pelvic‑floor specialist.
Step‑by‑Step PT Session Blueprint
A typical first visit looks like this:
- Assessment: The therapist measures bladder volume, evaluates pelvic‑floor strength with a perineometer, and checks posture and core stability.
- Education: You learn the anatomy of the bladder‑pelvic floor‑nerve triangle and why timing matters.
- Biofeedback Setup: EMG pads are placed, and a screen shows muscle activation patterns.
- Exercise Prescription: A set of 10-15 pelvic‑floor contractions, each held for 5seconds followed by a relaxed count, performed three times daily.
- Home Plan: A printable log, video links for proper form, and a reminder schedule on your phone.
Follow‑up visits adjust the program based on progress, often adding bladder‑training intervals or taping as confidence grows.

Potential Pitfalls and How to Avoid Them
Even with the best plan, mistakes happen. Here are common obstacles and quick fixes:
- Training the wrong muscles - Use biofeedback early to confirm you’re targeting the pelvic floor, not the glutes.
- Skipping home exercises - Set a timer or pair the routine with daily habits (e.g., after brushing teeth).
- Over‑relying on catheters - Work with your clinician to gradually increase voiding intervals, aiming for at least 4-6 attempts per day.
- Ignoring pain - Discomfort beyond mild fatigue may signal an underlying injury; pause and reassess with your therapist.
Key Takeaways
- Urinary retention often involves weakened or uncoordinated pelvic floor muscles.
- Physical therapy strengthens these muscles, retrains nerve pathways, and can reduce the need for catheters or high‑dose meds.
- Core PT tools include pelvic‑floor training, bladder training, biofeedback, and occasionally kinesiology taping.
- Typical therapy lasts 6-12 weeks with regular home practice.
- Consult a urologist or pelvic‑floor specialist if residual volumes stay high, symptoms persist, or you want to minimize medication.
Frequently Asked Questions
Can physical therapy completely cure urinary retention?
Physical therapy can resolve many functional cases, especially when the problem stems from weak pelvic‑floor muscles or disrupted nerve signals. Structural blockages often still need surgery or medication, but PT can improve outcomes and reduce reliance on invasive treatments.
How long does it take to see results?
Most patients notice a measurable drop in post‑void residual volume after 4‑6 weeks of consistent exercises. Full bladder‑control improvement usually appears around the 10‑week mark.
Is biofeedback necessary?
Biofeedback isn’t mandatory, but it speeds up learning by showing you exactly which muscles are activating. Many clinicians start with it for the first few sessions and then transition to “hands‑free” practice.
Can I do these exercises if I have a urinary catheter?
Yes. Therapists can tailor pelvic‑floor routines around intermittent catheter use, focusing on muscle activation between catheterizations to keep the muscles responsive.
What qualifications should a therapist have?
Look for a licensed physiotherapist with additional certification in pelvic‑floor rehabilitation or a credential from a recognized body such as the International Continence Society.



Crystal Heim
October 12, 2025Physical therapy targets the pelvic floor muscles to improve bladder emptying. It uses biofeedback and manual techniques. The therapist trains you to coordinate contraction and relaxation. This can reduce post‑void residual volume. Consistent sessions are key.
Sruthi V Nair
October 20, 2025Imagine your bladder as a river finding its own path. PT helps clear the blockages and restores flow. Keep moving forward and trust the process.
Patrick Vande Ven
October 28, 2025Urinary retention is often the result of dysfunctional detrusor activity and inadequate pelvic support. Physical therapy addresses these issues through a combination of manual therapy, neuromuscular re‑education, and targeted exercises. Manual techniques, such as myofascial release, can diminish tissue adhesions that impair bladder contractility. Neuromuscular re‑education focuses on restoring the timing of sphincter relaxation and detrusor contraction. Biofeedback devices provide real‑time visual cues that enable patients to internalise proper muscle activation patterns. Studies have demonstrated that patients who engage in structured pelvic floor physical therapy exhibit a statistically significant reduction in post‑void residual volumes. Moreover, the therapeutic protocol can be customised to address comorbidities such as chronic prostatitis in men and pelvic organ prolapse in women. In clinical practice, the therapist typically begins with an assessment of bladder diary entries and uroflowmetry results. This objective data guides the selection of interventions, ensuring they are both evidence‑based and patient‑centred. Patients are instructed to perform repeated voiding drills under supervision, gradually increasing the interval between attempts. Over the course of several weeks, neural pathways are reinforced, leading to more efficient voiding cycles. It is essential to maintain adherence to home exercise programs, as the therapeutic gains can regress without reinforcement. The integration of breathing techniques further supports intra‑abdominal pressure regulation during micturition. Clinicians should also monitor for signs of over‑activity, adjusting the regimen to avoid iatrogenic detrusor instability. In summary, a comprehensive physical therapy regimen offers a non‑pharmacological avenue for ameliorating urinary retention, with measurable improvements in residual volume and patient quality of life.
Debbie Frapp
November 5, 2025I've seen patients who were skeptical about PT, but after a few weeks they reported a noticeable drop in voiding difficulty. The therapist often incorporates diaphragmatic breathing, which seems to help relax the pelvic floor. It's also useful to keep a bladder diary so you can track progress over time.
Michelle Abbott
November 13, 2025From a biomechanical perspective, the integration of fascial manipulation, proprioceptive neuromuscular facilitation, and viscerosomatic reflex inhibition constitutes a synergistic protocol that optimally modulates detrusor‑sphincter dynamics. However, adherence metrics frequently suffer due to suboptimal patient education.
Matt Stone
November 21, 2025Stop ignoring PT it works.
Joy Luca
November 29, 2025You're missing the point PT isn’t a gimmick it’s a science that leverages motor unit recruitment and pelvic floor proprioception to recalibrate voiding patterns.
Jessica Martins
December 7, 2025Evidence suggests that a structured pelvic floor rehabilitation program can achieve a measurable decrease in post‑void residual volume, particularly when combined with patient education.
Doug Farley
December 15, 2025Oh great another miracle cure, because we all know therapists just wave a wand and poof urine flows perfectly.
Jeremy Olson
December 23, 2025I understand the frustration many patients feel when conservative measures fail, and I appreciate the thorough explanation of how targeted physical therapy can restore normal bladder function.
Ada Lusardi
December 31, 2025Wow this is so helpful 😊 I never realized PT could make such a difference 🙌
Pam Mickelson
January 8, 2026Keep at it! The more you practice the exercises, the quicker you’ll see those numbers drop. You’ve got this!
Julie Sook-Man Chan
January 16, 2026This info is spot on.
Amanda Mooney
January 24, 2026Implementing a scheduled regimen of pelvic floor strengthening and neuromuscular re‑education has demonstrable efficacy in reducing urinary retention.
Zac James
February 1, 2026Across cultures, pelvic floor therapy is increasingly recognized as a viable complement to medical management of bladder dysfunction.
mathokozo mbuzi
February 9, 2026The patient’s adherence to the prescribed regimen was observed to correlate positively with the reduction in residual volume, thereby underscoring the importance of sustained engagement.
Penny X
February 17, 2026It is incumbent upon healthcare providers to advocate for evidence‑based, non‑invasive interventions such as physical therapy, thereby upholding the ethical duty to minimize pharmacologic dependence.