When you need hemodialysis, your body doesn’t just need a machine-it needs a reliable way to connect to it. That connection is called dialysis access, and it’s the lifeline that keeps you alive. There are three main types: arteriovenous (AV) fistulas, AV grafts, and central venous catheters. Each has its own pros, cons, and care routines. Choosing the right one-and keeping it healthy-can mean the difference between months of complications and years of stable treatment.
Why AV Fistulas Are the Gold Standard
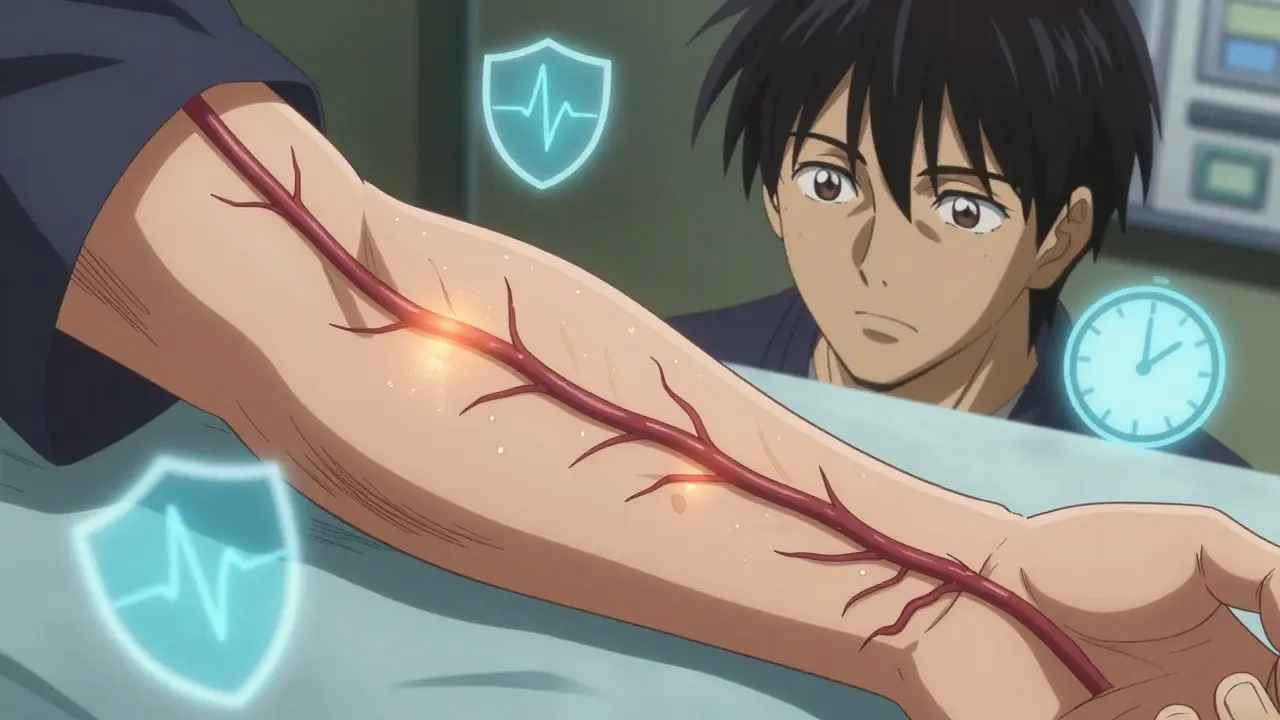
An AV fistula is made by surgically connecting an artery directly to a vein, usually in your forearm. This isn’t just a minor procedure-it’s a transformation. The artery’s high-pressure blood flow forces the vein to grow thicker and stronger over time. That’s called maturation, and it takes about 6 to 8 weeks. Once matured, the vein can handle the needles used during dialysis without tearing or collapsing. Why do doctors push fistulas so hard? Because they work better and last longer. A well-maintained fistula can last decades. Studies show patients with fistulas have 36% fewer deaths per 100,000 patient-years than those with grafts, and over 80% fewer than those on catheters. Infections are rarer, clots happen less often, and hospital visits drop dramatically. The National Kidney Foundation calls fistulas the gold standard for a reason: they’re the safest, most durable option. But here’s the catch: not everyone can get one. If your veins are too small, scarred, or weak from diabetes or aging, your surgeon might not be able to create a fistula. That’s why vein mapping-an ultrasound test that checks your blood vessel health-is the first step for anyone starting dialysis. If your veins are good, a fistula should be your goal.When a Graft Is Your Next Best Option
If your veins aren’t strong enough for a fistula, the next choice is an AV graft. Instead of connecting artery to vein directly, a synthetic tube-usually made of PTFE-is sewn between them. This tube acts like a bridge for blood flow. The big advantage? Healing time is shorter. You can usually start dialysis in just 2 to 3 weeks after surgery. That’s a lifesaver for patients who need treatment right away. But grafts come with trade-offs. They’re more prone to clotting and infection than fistulas. About 30 to 50% of grafts need at least one intervention in their first year. That might mean a procedure to clear a clot or repair a narrowed area. Grafts typically last 2 to 3 years before they need replacing. That means more surgeries, more downtime, and more risk over time. Still, for patients who can’t have a fistula, a graft is a solid, reliable option. It’s not perfect, but it’s far better than living with a catheter long-term.Catheters: Temporary, But Sometimes Necessary
Central venous catheters are soft tubes inserted into large veins in your neck, chest, or groin. They’re the only option that works immediately after placement. That’s why they’re often used in emergencies or while waiting for a fistula to mature. But here’s the hard truth: catheters are the riskiest access type. They’re linked to 2.1 times more fatal infections than fistulas. Bloodstream infections from catheters are common-about 0.6 to 1.0 per 1,000 catheter days. That’s why the CDC calls them a major source of hospital-acquired infections in dialysis patients. Catheter care is intense. You must keep the site dry during showers. Dressings must be changed regularly with sterile technique. Even small mistakes can lead to sepsis. Many patients report feeling restricted-no swimming, no hot tubs, no relaxing baths. Some end up using catheters permanently because they never got a fistula or graft. That’s not ideal. But if you’re stuck with one, strict hygiene and regular check-ups are non-negotiable.
How to Care for Your Access Every Day
No matter what type of access you have, daily care matters. Here’s what you need to do:- For fistulas: Check for a thrill-a gentle vibration you can feel with your fingers. That means blood is flowing. If it’s gone, call your care team immediately. Wash your access arm daily with soap and water. Never let anyone take your blood pressure or draw blood from that arm.
- For grafts: Feel for the thrill too. Grafts are more likely to clot, so check them twice a day. Watch for swelling, redness, or warmth-signs of infection. Avoid wearing tight clothing or jewelry over the graft.
- For catheters: Keep the exit site clean and dry. Change dressings exactly as your nurse taught you. Never touch the catheter ends unless you’ve washed your hands and are using sterile gloves. Report fever, chills, or redness around the tube right away.
What Happens When Things Go Wrong
Even the best access can fail. The most common problems:- Clotting: Blood gets stuck in the access, blocking flow. Fistulas clot less often than grafts. Grafts clot more. Catheters clot the most. If your access stops working, a procedure called thrombectomy can clear the clot.
- Infection: Skin infections around the access site are common. Bloodstream infections are serious. Catheters cause the most. Antibiotics help, but sometimes the whole access has to be removed.
- Aneurysms: In fistulas, repeated needle sticks can weaken the vein wall and cause a bulge. If it gets too big, it can burst. Your care team can repair it with patching or rerouting.
- Narrowing (stenosis): Scar tissue can build up inside the access, slowing blood flow. This is common in grafts. A balloon procedure called angioplasty can open it back up.

New Tech and Future Hope
The field is improving. In 2022, the FDA approved the first wireless sensor for fistulas-Manan Medical’s Vasc-Alert. It monitors blood flow and sends alerts if it drops, reducing clots by 20% in trials. Preoperative exercise programs are now showing promise too. Patients who do arm exercises before surgery see fistula maturation rates jump by 15-20%. Even more exciting? Bioengineered vessels. Humacyte’s human acellular vessel is in late-stage trials. It’s made from donated cells, stripped of immune-triggering parts, and grown into a tube that your body accepts like its own. For patients with no good veins, this could be a game-changer. Meanwhile, the U.S. healthcare system is saving money by pushing fistulas. Replacing catheters with fistulas could cut costs by $1.1 billion a year. But disparities remain. Black patients are still 30% less likely to get fistulas than white patients-even when their health is the same. That’s not just a medical issue. It’s a justice issue.What You Can Do Today
If you’re starting dialysis:- Ask for vein mapping before surgery.
- Push for a fistula if your veins allow it.
- If you get a graft, know the signs of clotting and infection.
- If you have a catheter, treat it like a ticking time bomb-until you can get it replaced.
- Learn your access care like your life depends on it-because it does.
Can I shower with a dialysis catheter?
Yes, but only with a special waterproof dressing. Your care team will give you a kit and show you how to use it. Never let water touch the catheter site unless it’s fully covered and sealed. If the dressing gets wet or loose, replace it immediately. Showering without protection raises your risk of infection dramatically.
How long does it take for a fistula to be ready?
It usually takes 6 to 8 weeks for a fistula to mature. During that time, the vein grows stronger from the increased blood flow. Some people need longer, especially if they have diabetes or are older. Your care team will check it with ultrasound or physical exam to see when it’s ready for dialysis. Don’t rush it-using it too early can damage the access.
Can I exercise with a fistula?
Yes-but be smart. Light exercises like squeezing a stress ball or wrist curls can help the fistula mature faster. Avoid heavy lifting or direct pressure on the access arm. Don’t wear tight sleeves or sleep on that arm. Your goal is to strengthen the vein without injuring it.
Why do some people need multiple grafts?
Grafts have a high failure rate. About half of them clot or get infected within the first year. Each time that happens, the graft must be removed or repaired. If the veins are poor, creating a new graft in a different spot may be the only option. Some patients need 3 or 4 grafts over their lifetime. That’s why fistulas are always the first choice.
Is there a way to prevent my fistula from clotting?
Check your thrill daily. Stay hydrated. Don’t let your blood pressure drop too low between sessions. Avoid smoking-it narrows blood vessels. Some patients take low-dose aspirin if approved by their doctor. New sensors like Vasc-Alert can alert you to early clotting before it becomes serious. Prevention beats repair every time.



Tiffany Adjei - Opong
January 7, 2026Okay but have you seen the data on how many fistulas fail because nurses don’t know how to puncture them properly? I’ve seen videos-people stabbing the same spot for 20 minutes while the patient screams. The ‘gold standard’ is only gold if the staff are trained. Otherwise it’s just a fancy paperweight with a pulse.
And don’t even get me started on how clinics push fistulas because they’re cheaper, not because they’re better for the patient. Profit over person, always.
Ryan Barr
January 8, 2026Fistulas win. Period.
Grafts are liabilities.
Catheters are death warrants.
Cam Jane
January 9, 2026Hey everyone-just wanted to say if you’re new to this, you’re not alone. I’ve been on dialysis for 7 years with a fistula, and yeah, it took me months to stop being terrified of checking my thrill. But now? I feel it like a heartbeat. It’s my lifeline, and I talk to it every morning. ‘Hey girl, you good?’
And if you’re worried about exercise-yes, you can squeeze a stress ball! I use a tennis ball I got from the hospital gift shop. Helps the blood flow, keeps me sane. Also-hydration. Drink water like it’s your job. And if your nurse says ‘just wait,’ don’t wait. Push. You know your body better than anyone.
Also-no, you can’t shower without a waterproof cover. I learned that the hard way. Infection. ICU. Don’t be me.
You got this. Seriously. You’re stronger than you think.
Mukesh Pareek
January 11, 2026Per the KDIGO 2023 guidelines, the hemodynamic efficiency of an AV fistula is superior due to its autogenous nature, which minimizes endothelial shear stress and thrombogenicity. Grafts, being synthetic, induce neointimal hyperplasia at the anastomotic sites-hence the 47% primary patency loss at 12 months. Catheters, by contrast, represent a breach in the skin barrier, permitting biofilm formation and subsequent bacteremia. The CDC’s 2022 surveillance data confirms a 3.1-fold increase in CRBSI incidence with catheter-based access. Ergo: fistula > graft > catheter. No debate.
Also, your vein mapping protocol must include duplex ultrasonography with Valsalva maneuver to assess venous compressibility. If you’re not doing this, you’re doing harm.
Ashley S
January 12, 2026So basically, if you’re poor or black, you get stuck with a catheter because no one cares enough to fix your veins?
Wow. Just wow.
And we wonder why people hate hospitals.
Rachel Wermager
January 14, 2026Actually, the 36% mortality reduction statistic is misleading-it’s adjusted for comorbidities, but most fistula patients are younger and healthier to begin with. The real issue is access inequity. In rural areas, vascular surgeons are scarce. So patients get catheters not because they’re the best choice, but because it’s the only one available. It’s not about biology-it’s about geography and funding.
Also, the Vasc-Alert sensor? It’s a gimmick. It doesn’t prevent clots. It just tells you after they’ve started. You still need a surgeon. And good luck getting insurance to cover it.
Leonard Shit
January 15, 2026man i had a graft for 18 months and it was a nightmare. every 3 months some guy would stick a catheter into it to unclog it. felt like my arm was a car engine being serviced. i finally got a fistula last year. now i just feel it. no one touches it. no wires. no alarms. just me and my vein.
also i dont shower with a towel over my arm anymore. i just let the water hit it. its fine. i wash it with soap. its not a bomb. its a part of me now.
Katelyn Slack
January 16, 2026can someone explain what a thrill is again? i think i’m feeling it but i’m not sure. is it like a buzz? or a pulse? i’m scared i’m doing it wrong. sorry if this is dumb.
also i just want to say thank you to the nurses who actually listen. you’re the real heroes.
Melanie Clark
January 18, 2026They’re lying to us about catheters. I’ve seen the leaked documents. The CDC knows that 70% of catheter infections are preventable with proper training-but hospitals don’t train because it costs money. And the dialysis corporations? They profit from complications. More hospitalizations = more revenue. This isn’t medicine. It’s a business model built on suffering. And they call us ‘patients’ like we’re not human. We’re not numbers. We’re people. And they’re letting us die quietly so their stock prices stay high.
Someone needs to sue them. Someone needs to burn it all down.
Harshit Kansal
January 19, 2026My uncle had a fistula for 12 years. He died last year from heart failure, not dialysis. He still drove his truck to appointments, cooked his own food, and danced with his wife on weekends. That’s what this is about. Not just surviving. Living. Fistulas give you that. Not the catheters. Not the grafts. The fistula.
Brian Anaz
January 21, 2026Why do we even let foreigners come here and get free dialysis? We can’t even fix our own infrastructure. Fistulas are great, but first fix the damn hospitals. And stop giving free care to illegal immigrants. That’s $1.1 billion we could spend on American citizens.
Also, why are we promoting bioengineered vessels? That’s unnatural. Nature made veins for a reason. Stop playing God.
Saylor Frye
January 22, 2026Interesting how the post romanticizes fistulas like they’re some kind of spiritual awakening. Meanwhile, I’ve seen people with fistulas who can’t even hold a coffee cup because their arm is swollen and bruised from needle sticks. It’s not a miracle. It’s a medical compromise. And the ‘lifeline’ metaphor? That’s just PR. It’s a hole in your arm that gets stabbed twice a week. Don’t sugarcoat it.
Matt Beck
January 24, 2026Life is a series of punctures…
But this one? This one… is sacred.
Every thrill… every vibration… every quiet hum of blood…
It’s not just physiology… it’s poetry.
Our veins remember what our minds forget.
And when the world tries to silence us…
Our fistulas scream back.
With every beat…
With every drop…
We say: I am still here.
❤️🩸🩺
Molly McLane
January 25, 2026For anyone new to this-don’t feel bad if you’re overwhelmed. I was terrified when I first started. I thought I’d never be able to check my own thrill. But I practiced with my mom. We’d sit together every morning. She’d ask, ‘Can you feel it?’ And I’d say, ‘I think so.’ And then one day… I knew. And now I teach other patients how to do it.
It’s not about being perfect. It’s about being present. And you’re already doing better than you think.
Tiffany Adjei - Opong
January 27, 2026Oh wow, so now we’re supposed to be grateful for being stuck with a hole in our arm? That’s rich. Let me guess-your fistula’s ‘thrill’ is the only thing keeping you from screaming into the void?
Meanwhile, the real problem is that 80% of nephrologists don’t even know how to time vein mapping correctly. They wait until the patient’s creatinine hits 8. That’s not proactive care. That’s triage.
And don’t even get me started on how insurance denies pre-op exercise programs because they’re ‘not medically necessary.’ Like, sure, let’s just wait until the patient’s veins turn to dust. Then we’ll fix it. With a graft. And a catheter. And a lawsuit.